Care Coordination and Behavioral Health

Session B5a
October 18, 2014
How to Crash the Party:
Bringing Behavioral Health Specialists to the Care Coordination Team
Mary Jean Mork, LCSW
Director of Integration
MaineHealth and Maine Behavioral Helathcare
Collaborative Family Healthcare Association 16 th Annual Conference
October 16-18, 2014 Washington, DC U.S.A.
Faculty Disclosure
I have not had any relevant financial relationships during the past 12 months.
Learning Objectives
At the conclusion of this session, the participant will be able to:
Identify barriers and success factors for care coordination.
Identify a “success factor” to immediately address.
Create a plan for addressing this factor upon return to work.
Learning Assessment
A learning assessment is required for CE credit.
A question and answer period will be conducted at the end of this presentation.
Agenda
Description of Care Coordination (CC) Team
Challenges for Behavioral Health Specialists (BHS)
Role and value of BHS on the team
Success factors and strategies for maximizing team effectiveness
Activity – Developing Action Plans
Question and answer period
Patient Centered Medical Home (PCMH)
– the Concept
(Behavioral Health)
From deGruy 10.10
Internet Citation: Figure 1. Family tree of terms in use in the field of collaborative care: A National Agenda for Research in Collaborative Care. June 2011.
Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/research/findings/final-reports/collaborativecare/collab3fig1.html
Care Coordination
The deliberate organization of patient care activities between two or more participants involved in a patient’s care to facilitate the appropriate delivery of health care services.
From: Safety Net Medical Home Initiative. Care Coordination: Reducing Care
Fragmentation in Primary Care. Implementation Guide. May 2013
“ If a person doesn’t have a roof over their head, if they don’t have a meal, if they’re a victim of physical or sexual abuse if their household has a lot of stress in it, if their kids’ school is not safe, then that's going to impact their health…..that health is more than just the pill that we’re giving you or the hospital that we put you in. It’s all the other parts of your life and whether they’re working in harmony.”
Dr. Jeffrey Brenner in interview “What Primary Care has to Learn from Behavioral Health”.
National Council for Behavioral Health.
Meet George
Barriers to Care Coordination:
Roles
Rules
Arrangements
Turf
Who is involved?
Care Managers
Case Managers
Behavioral Health Clinicians
Care Coordinators
Transition coaches
Peer navigators
Health coaches
RN’s in the practice
Primary care providers
Primary care staff
Family and community supports
Other?
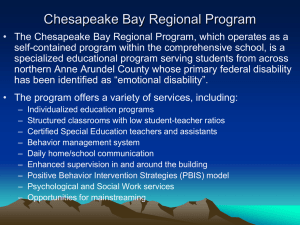
Mental Health
Treatment Team
• Case Manager
• Team Leader – LCSW
• Peer/Youth Support
• Psychiatry
• Medical Director
Preventative and
Acute Care
Chronic Care
High Utilization
Chronic Care with MH
Substance Abuse
High Utilization with
MH Dx
Primary Care
Care Team
• Provider
• Nurse
• Medical Assistant
• Integrated BH Clinician
• Nurse Care Manager
• Health coach/navigator
“We're all going to have to give up some turf. After all, it's actually the patient's turf.”
Robert McArtor, MD, CMO MaineHealth
Hospital
Patients
Patient Population
Other
Complex
Patients
Specialty Medical
Care
Primary Care
Coordinated Care Team
( Potential Team Members )
Care Manager
Behavioral Health Clinician PCP and
Clinical Care
Complex
Care
Mgmt summary of an interesting point. You can
Health Guide position the text box anywhere in the document. Use the Drawing Tools tab to
Team
Specialty Mental Health
Care
CCT social worker
Psychiatric Consultation
Care Plan Team
Care Coordination System Management
Care Coordination and
Behavioral Health
Saturday, September 20, 2014
Powered by
Q1: Describe your involvement on the care coordination team
Q2: I If you have tried to have more involvement in care coordination activities, what barriers have you experienced?
Q3: If you are presently involved in care coordination activities in your practice, what has been most successful in helping be part of these activities?
What else did I hear?
“It was horrifying. We don’t have anything in our practice.”
“We can’t coordinate unless there’s a mistake in scheduling, because she (the care manger) uses the office when I’m not there.”
“Who is my team?”
“I didn’t fill it out because it doesn’t pertain to me.”
Complex Care Teams
(Social, behavioral and medical complexities)
Behavioral
Health
Needs
Medication
Access
Community
Resource
Needs
Complex
Coordination
Needs
Providing:
• A multidisciplinary approach to complex care coordination;
• Team collaboration;
• Community resource partnerships, and
• Standardized best practice interventions
BHS’s value on CC team
Direct service to Patient
Link to specialty MH and SA treatment
Liaison to psychiatric services
“Triage” role with psychiatry referrals.
Consultation to CC team
System perspective
Behavioral lens for medical system
Medical system lens for behavioral health
Expertise with individualized care plans tailored to patient
Patient and family centered focus
Common Challenges for BHS
Population health
Using data to inform work
Understanding nuances of different care management roles
Clarifying roles around behavioral change,e.g. with health coaches
Ability to access specialty MH, SA and psych services
CC Success Factors
Clarity, connection and non-duplication of:
Roles
Functions
Responsibilities
Clarity about population being coordinated
Timely and accurate data
Tracked and shared outcomes
“Partnership” approach to care
Individualized patient centered planning process for care plans
Shared Care plans and “alerts” throughout system
Standardized coordination of care
“Team” members have assigned tasks based on individual care plan
“Team” lead to manage complex care situations
Strategies to Improve CC
Identify who is coordinating care
Identify leaders
Multidisciplinary case presentations
Target specific patients, design services around individual’s goals, coordinate care, track results
Identify impact measures, e.g. ED usage for specific populations
Make connections with community providers and continuum of care
Additional considerations for CC
Funding – are there:
New funding streams that support this work?
Cost savings and medical cost offsets?
Honor the patient voice in development of the care plans
Value and nurture the team relationships!
Resources
Websites
http://integrationacademy.ahrq.gov/ - AHRQ Academy for Integrating Behavioral Health and
Primary Care
www.uwaims.org - Advancing Integrated Mental Health Solutions – resources for implementation from University of Washington
www.integratedprimarycare.com – National clearinghouse site for information on integrated care from University of Massachusetts.
www.integration.samhsa.gov
- SAMHSA-HRSA Center for Integrated Health Solutions
www.thenationalcouncil.org
– the National Council for Community Behavioral Healthcare.
Publications
IHI Innovation Series 2011. Craig, et.al. Care Coordination Model: Better Care at Lower Cost for People with Multiple Health and Social Needs.
http://www.improvingchroniccare.org/downloads/reducing_care_fragmentation.pdf
Reducing Care Fragmentation: A Toolkit for Coordinating Care
Session Evaluation
Please complete and return the evaluation form to the classroom monitor before leaving this session.