J Anx Disord - Portland State University
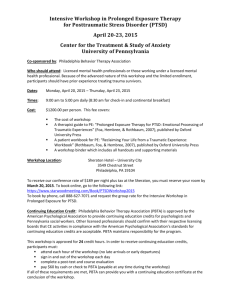
advertisement

Irene Powch, Ph.D. Portland State University and Mental Illness Research, Education and Clinical Center, Northwest June 16, 2011 Knowledge, Perceptions, and Utilization Poll How many… Know very little about PE—just curious? Know enough to fear PE? Know enough to be enthusiastic about PE? Know the evidence base but have little sense of what the process of PE is like? Know enough to discuss PE with veterans in a supportive, collaborative, engaging, and motivating way…and make good referrals? Consider themselves competent practitioners of PE? Goals of Today’s Presentation To give you a sense of: How the treatment rationale is discussed with veterans in a supportive, collaborative, engaging, and motivating way What goes on in PE sessions How the therapeutic relationship is used in PE The evidence base that supports PE as an effective treatment for PTSD What kinds of changes do real clients/veterans experience (videos)? Where you can learn more Practical applications would include: For anyone who works with veterans: Ability to help a veteran consider if PE is a good treatment choice for him/her For therapists: have a better sense of whether you may wish to take the intensive training to become a PE competent therapist. Overview Brief Introduction to PE Summary of the Evidence Base Supporting PE When is PE indicated? Deepen understanding of PE through session by session highlights and presentation of tx rationale Video clips (PE sessions, Recovery Interviews) Resources for further learning Questions/discussion What is PE? Prolonged Exposure Therapy (PE) is a Cognitive-Behavioral Treatment for PTSD, developed by Edna Foa, Ph.D., Director of the Center for the Treatment and Study of Anxiety 8 to 12 sessions of 1.5 hour duration, with 2 hours of daily practice and typically one phone contact between sessions. In the context of a supportive therapeutic alliance, the trauma survivor intentionally approaches the trauma memory and reminders long enough and often enough to experience a reduction in anxiety that opens the door to new learning. The memory and reminders lose their power to elicit a trauma response. Evidence for Effectiveness Over 20 years of research supports the effectiveness of exposure therapy for PTSD. By 2000, 12 studies had tested exposure therapy. All finding positive results; 8 of these received the highest AHCPR rating for methodological rigor. Based on this, the Practice Guidelines for the International Society of Traumatic Stress Studies (Foa, Kean, & Friedman, 2000, p79) concluded that “exposure therapy shouldbe considered as the first line of treatment unless reasons exist for ruling it out” A 2010 meta-analytic review of 13 published RCTs of PE for PTSD (675 participants) found that the average PE treated patient faired better than 86% of patients in control conditions at posttreatment on PTSD symptoms. Real World and Beyond PTSD PE is effective in “real world” VA clinical contexts, not only in pristine clinical trials. Turek et al., J Anx Disord 2010 PE results in clinical improvements on many dimensions in addition to PTSD symptoms, including decreased depression, increased quality of life, improved sleep, improvement in reported physical health symptoms, improved social function, and posttraumatic growth, including increased sense of new possibilities and personal strength. Powers et al., Clin Psych Review, 2010; Hagenaars et al., JTS, 2010; Rauch et al. Depr & Anx 2009 How Does PE Work? Theoretical base: Emotional Processing Theory (Foa & Kozak, 1986). PTSD emerges due to development of a pathological fear structure concerning the traumatic event. (Includes representations about stimuli, responses, and their meaning) Foa & Kozak, 1986; Steketee & Rothbaum, 1989 Attempts to avoid this activation result in avoidance sxs Fear reduction requires activation & integration of corrective information. Repeated imaginal approach in the context of a therapeutic, supportive setting: 1. promotes habituation & corrects belief that anxiety lasts forever 2. blocks the short term reward of avoidance 3. promotes realization that remembering is not dangerous 4. helps survivor differentiate the trauma from the rest of the world 5. sense of personal incompetence becomes sense of mastery How Does PE Work? Theoretical base: Emotional Processing Theory (Foa & Kozak, 1986). Reminders of the trauma trigger distressing thoughts and feelings, including a “fight/flight/freeze” response even when there is no current danger. Escape and avoidance behaviors develop to obtain temporary relief that serves to maintain PTSD. By intentionally approaching instead of avoiding safe reminders—and staying long enough for anxiety to decrease, new learning happens: The memory is not dangerous! The reminders are not dangerous! Anxiety does not last forever! I can conquer the memory! I am competent! When Is PE Indicated? Before First Session: Assessment Is PTSD the primary problem? PCL, CAPS, BDI, PCI, chart review & psychiatric interview Are there significant more urgent or treatment interfering problems that need to be addressed first or simultaneously? Any current situation or condition that poses imminent danger or interferes with ability to engage reliably in outpatient treatment. Fine Tuning: PE vs. CPT/CPTC? Both therapies have a strong evidence base. There is not yet sufficient research to guide treatment matching. Considerations that may favor PE: Client resonates strongly with the rationale behind PE and believes PE is the more direct approach that s/he needs Therapist is more comfortable/competent with PE Fear (fight/flight/freeze) is the predominant emotion that is triggered by trauma reminders. Client has enough memory of one of the traumas that causes their PTSD symptoms to form a narrative. Client is highly motivated to “de-commission” triggers that are avoided and get in the way of enjoying highly valued activities. Fine Tuning: PE vs. CPT/CPTC? Considerations that may favor CPT: Client resonates strongly with the rationale behind CPT and believes that s/he needs to change his/her thinking before changing behavior. The client has complete amnesia for the event. Therapist is more comfortable/competent with CPT The distress is driven by something other than fear/horror/helplessness (for example, overwhelming shame at the thought of exhibiting fear; guilt about perpetration or other complications that block fear.) Session 1 Engagement through Trauma Interview Treatment Rationale round one (general) Skill-the gift of breath Practice assignment—breathing, listen to tape Session 2 Supportive and motivating review of practice (breath) Engagement through discussion of common reactions to trauma Treatment rationale round 2 (in vivo) Collaborative setting up SUDS & in vivo hierarchy Collaborative planning of in vivo practice; continue practice breathing, listen to tape Between session planned check-in call Session 3 Reassuring & helpful review of in vivo practice Engagement through treatment rationale round 3 (imaginal) First Imaginal Exposure (clinician is a reassuring presence, does not interfere with processing) Reassuring and affirming debrief Practice assignment—continue practice breathing, in vivo exposure, and add imaginal exposure, listen to tape Between session planned check-in calls as needed Intermediate Sessions Reassuring & helpful review of in vivo & imaginal practice Supportive, socratic questions regarding “gaps” or other puzzling incongruencies; collaboratively identify “hot spots” Gradually move imaginal exposure in on “hot spots” Practice assignment—continue practice breathing, in vivo exposure, and add imaginal exposure, listen to tape Between session planned check-in call Final Session (usually near 10) Celebratory review of in vivo and imaginal exposure work and progress made Drop in SUDS and PCL scores Review and celebrate addition of many enjoyable activities that veteran previously was unable to do at all Make suggestions for continued practice; plans for future Videos 10 minute segment of PE 10 minute segment of PE recovery interview More from Our Clinic PrePost (change on the PCL) 62 38 72 32 54 24 55 26 56 33 80 40 40 27 65 45 60 42 70 25 42 19 60 32 (24) (45) (30) (29) (23) (40) (13) (20) (18) (45) (23) (28) * From almost completely isolated to going back to school to become a paramedic; faced a situation similar to major trauma (burn victims) and slept like a baby the following night. * From unable to stand out on back porch at night to enjoying walks at night in safe neighborhood. * From almost completely isolated to going out to concerts with friends. * Finally able to enjoy grandkids, wife, travel. Resources for Further Learning Handout References for clinical manuals and patient manuals for PE and related evidence-based treatments. References for reviews of the evidence base and key studies. Websites for continuing education related to effective treatments for PTSD Discussion Questions and discussion from the audience