Aboriginal Psychiatry Mentoring Program - Donna
advertisement

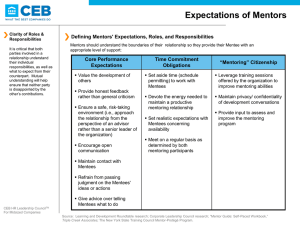
Aboriginal MHDA Psychiatry Mentoring Program Donna Stanley Clinical Leader Aboriginal MHDA Orange Western NSW LHD Acknowledgment of Country With respect I honour the traditional owners of the land upon which we meet today. Acknowledging the Gumbaynggirr Peoples thousands of years of spiritual connection to this country and for welcoming us here to enjoy and celebrate this beautiful place. I honour and pay my respect to Elders past & present, all other Aboriginal nations and our Non-Aboriginal Brothers & Sisters. Introduction • ‘Closing the Gap’ • Defining Mentoring • Historical background – Mentoring Concept – Policy Context • Mentoring Model • Mentoring Review • Future work Defining Mentoring ‘Mentoring is a mutually beneficial relationship that involves a more experienced person helping a less experienced person to achieve his/her goals.’ Historical Background • • • • Concept developed in 2007 18% of Inpatient Population Aboriginal Aboriginal Population 7.3% (ABS Data) Policy implementation by MH Teams, Strategy 5: A supported and skilled workforce (Mentoring) Historical Background The Project Aim • To develop long term sustainable models of mentoring between the Aboriginal Mental Health Workforce and psychiatrists who are current employees of [former] GWAHS Objectives • To facilitate two way learning between Aboriginal Mental Health and Psychiatry • To provide sound clinical mentoring and support to Aboriginal Mental Health Workers • To improve support structures for Aboriginal Mental Health Workers Historical Background Underlying Principles of the Project • AMHWs are essential to improving AMH [Aboriginal Mental Health] • Psychiatrists are a critical part of the process to improve AMH • Education and learning is required both ways • This work is additional to current services provided by both psychiatrists and AMHWs • The project is a long term career development process • Participation in the project is on a voluntary basis Mentoring Model Who provides the mentoring? • A consultant psychiatrist is contracted to provide mentoring for a maximum of two days per month. He is currently providing mentoring one day per month. He is flown from Sydney to Orange specifically to conduct the sessions. Mentoring Model Who attends the mentoring sessions? • Aboriginal Mental Health Clinicians and Trainees, Clinical Leader, Area Coordinator and State-wide Coordinator participate in mentoring sessions. (Voluntary) Mentoring Model Coordination The Clinical Leader coordinates • the psychiatrist’s visit • arranges the individual and group sessions • sends out a mentoring schedule for the coming year • Individuals are allocated individual sessions during each visit. Mentoring Model • • • • Individual Mentoring Group Mentoring Post Session Follow up Organisational Follow up Mentoring Review • Reviewers engaged in 2012 (Carol Watson and Nea Harrison) • Methodology based on qualitative data – One Focus Group – 39 Interviews – Lead by Clinical and Management Steering Group Mentoring Review • Mentees: Access to highly experienced, independent, supportive senior mental health clinicians and a two way learning environment • Senior MH Clinical Leaders: Time and access to independent mentors who understand the mental health context • Mentors: Time specifically allocated for mentoring and opportunity to build relationships and learn more about Aboriginal culture, and • Organisation/Management: A committed group of high calibre psychiatrists provide additional support to the Aboriginal Mental Health workforce and learning's are taken back to the team to inform practice. Mentoring Review • Building of mentees’ knowledge, skills and confidence • Mentees supported, validated and empowered • Psychiatrists’ knowledge of Aboriginal culture, community concerns, family dynamics and the role of the AMHW strengthened • Aboriginal mental health workers retained, and • Status and perceived value of Aboriginal MHDA workforce increased. Mentoring Review Issues noted were: • The lack of initial clarity around a formal program design, and some variances in the type of mentoring models conducted by different psychiatrists; this in the context that there is overall agreement to the benefits of the program. • Concerns about funding support for the program moving forward • Consideration of other clinical professional groups as mentors, and • Clarity of governance for the program – monitoring, quality processes and reporting. Future Work Challenges arising from the Review are now to ensure: • A core mentorship model is further developed • A monitoring and evaluation framework is developed • Workforce requirements are reviewed • A commitment to continue Aboriginal MHDA Mentoring Program Comments/Questions