Challenges in Hearing Aid Fitting in Older Adults
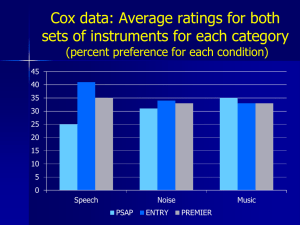
advertisement

Alison M. Grimes, AuD University of California, Los Angeles They work! People who wear properly fitted hearing aids, and who have been counseled regarding reasonable expectations, and who have undergone audiologic rehabilitation, are satisfied with hearing aids Hearing aids do not mean that you’re getting old, senile, incapable, stupid, infirm and all of those other negative stereotypes Their hearing aid is less obvious than their hearing loss Lots of people wear hearing aids, but lots more need to and don’t The cost of NOT wearing hearing aids is potentially much greater than the dollars spent to purchase them Denial Stigma Unawareness that there is a problem Avoidance of Diagnosis ◦ Subsequent avoidance of treatment Minimizing the Problem Friend/relative who had hearing aids that “didn’t work”; subsequent generalized belief that hearing aids don’t work Confusion and distrust about hearing aid salespeople Cost vs perceived benefit “My hearing is normal for my age” “I don’t have a hearing loss—s/he mumbles!” “I hear what I need to hear” First, get them through the door! Appropriate and thorough counseling following diagnosis, prior to hearing aid selection ◦ Reasonable expectations ◦ Listening strategies ◦ Other hearing assistance technologies Hearing aid selection based on ◦ Specific patient variables and needs/desires ◦ Effectiveness over cosmetics Verification of audibility using evidence-based procedures Patient/family counseling NIDCD/VA Hearing Aid Trial (Larson, et al., 2000) published in Journal of the American Medical Association Landmark clinical study Double-blind, three-period, three treatment crossover design. Conclusion: Hearing aids work! No significant difference among three hearing aid circuits ◦ WDRC ◦ Linear compression-limiting ◦ Linear peak-clipping Subjects showed significantly improved aided vs unaided communication ◦ In Quiet ◦ In Noise Kricos, et al., 2007 (part of the report of the update of JAMA 2003 NIDCD/VA Study) “Despite considerable evidence regarding the detrimental effects of untreated hearing loss, …there continues to be an underutilization of hearing aids by adults” CPHI (measure of handicap) scores significantly poorer in non-users than in users ◦ That is, greater handicap in the non-users. Participants benefited from extensive auditory rehabilitation and expert fitting techniques Significant long-term subjective benefit and satisfaction with hearing aids. Subjects weren’t different—but their management was Intensively managed by Audiologists Patients afforded the opportunity to evaluate different hearing aid fittings ◦ Fittings based on prescriptive targets verified with probe-microphone measures Given extended periods of trial use Able to select their preferred fitting (This is not how hearing aids are typically fitted and dispensed!) Intensive Management Patient involvement in the selection and fitting process Probe Microphone measures to ensure maximum audibility ◦ Every time “Trial Period”— ◦ What does this mean? ◦ Are we stuck with this forever? Legally, perhaps Can we term it something different? Denial/Stigma Belief that hearing aids are ineffectual Medical/audiological professionals who downplay significance of hearing loss Cost Sales aspects Cultural/Linguistic Issues Hearing aids = badge of aging and senility Denial ◦ Hearing loss is gradual in onset ◦ Don’t know what you don’t hear because you can’t hear it! ◦ Tendency to externalize problem “she mumbles” Lack of awareness of the psychological, social, emotional, physical and cognitive impacts of untreated hearing loss Belief that it’s OK to procrastinate Perceived poor performance in noise Friend/family member who has had poor outcomes with hearing aids Real-world performance doesn’t match exaggerated advertising claims Lack of pre-fitting counseling regarding reasonable expectations Physicians fail to inquire or screen for hearing loss “It’s normal for your age” If not surgically treatable, HNS physicians may be uninterested Audiologists may downplay significance of “mild” hearing loss ◦ (tentative counseling) Perceived high cost for value Lack of third-party funding Bundled hearing aid pricing model ◦ Bad for consumers? ◦ Bad for audiologists? Unrealistic advertising Confusion about who sells hearing aids ◦ What are their qualifications? From whom should hearing aids be purchased? Audiologist? Hearing aid salesperson? Physician? Internet? Mail-order? Any device that’s sold with a 30-day “trial period” sets up expectation of failure Long history of sales abuses Well known that intervention including hearing aids underutilized ◦ Lack of providers with cultural/ethnic/linguistic match ◦ Poverty ◦ Lower utilization of health systems overall ◦ Unwilling/”inappropriate” to discuss perceptions and feelings about hearing loss Auditory Deprivation: ARHL is gradually progressive ◦ Becomes a greater issue as period of time of deprivation grows ◦ Creates challenges when hearing aids first fitted Immediate restoration of sound Negative psycho-social, psychological and cognitive impacts Necessary Not sufficient to completely address multiple problems associated with speech understanding Necessary to first have audibility ◦ Insofar as properly fitted hearing aids provide audibility Then employ ◦ Other hearing assistance technologies Auditory Rehabilitation Program ◦ Counseling ◦ Communication Skills Training (Move to cochlear implant if needed) Patient Preferences ◦ What can the patient manage? ◦ What can the ear canal accept? Style ◦ Custom vs BTE Binaural vs Monaural ◦ Or other signal-routing (CROS, BICROS) Cost Program and/or Volume buttons? ◦ Multiple memories or programs—necessary or confusing Custom earmold/insert vs “dome”? Remote Control Device(s) Ear-to-ear communication—necessary or confusing? Bluetooth? Telecoil—mandatory? Auto-telecoil? “Noise reduction”? Directional microphones? Frequency transposition/compression? ◦ Insufficient evidence to judge efficacy/benefit relative to degree/configuration of hearing loss and age Patient/Family Decisions ◦ Features VC, PB, remote ◦ Color ◦ Price ◦ To some degree, style and arrangement Manufacturer ◦ Depends on the reason that a particular brand is requested Audiologist’s Decisions ◦ Signal processing scheme WDRC vs Linear Frequency Transp/Comp ◦ Gain/output requirements to assure audibility and comfort/safety across the speech spectrum ◦ To some degree, style and arrangement Based on patient needs • Audiologist Wants – Availability of appropriate gain and output across the speech spectrum based on patient’s hearing loss – Flexibility to manipulate by multiple frequency bands – Growth-room – reserve gain/output – Features and signal-processing options that are familiar and with which audiologist has had previous success – Good feedback algorithm – Responsive and responsible manufacturer with good customer support – Price that is justified by features offered – Rapid and successful patient acceptance – Cords/cables that work every time – Software that makes sense – Ability to see what the hearing aid is doing when changes are made • Patient Wants – “invisible” – “block out background noise” – “high-fidelity” with nearperfect speech understanding – Larger, longer-lasting battery – Easy to manipulate controls – Or no controls – – – – – Sturdy battery case Inexpensive Distance hearing Lack of feedback Physically and acoustically comfortable and ‘natural’ The #1 complaint of hearing aid users Latest MarkeTrak “listening in noise” shows 25% overall dissatisfied 61% overall satisfied 14% neutral Listening in noise ◦ Related to reduced speech perception The greater the degree of hearing loss, the greater the handicap associated with listening in noise Counseling to ensure reasonable expectations ◦ (the advertisements don’t tell the whole story!) An oversold technology? ◦ May lead to disappointment with hearing aids ◦ Importance of pre-fitting counseling Better termed “noise management” ◦ Makes listening in noise more comfortable Definition of noise varies ◦ Noise is the undesired signal ◦ The desired signal may have the same spectrum ◦ Noise is often others’ speech NR doesn’t improve speech perception ◦ Creates greater listening ease Highest negative rating is “use in noisy situations” Latest MarkeTrak “listening in noise” shows 25% overall dissatisfied 61% overall satisfied 14% neutral ◦ 39% neutral to dissatisfied – not a stellar statistic How can this be improved? ◦ Counseling ◦ Remote microphone technologies ◦ Communication strategies Benefit of DNR algorithm is not to make speech more intelligible ◦ Does reduce the cognitive effort involved in performing the task Shared attention extracting speech from noise ◦ Items presented in noise less likely to be remembered successfully ◦ Listening in noise: increase in listening effort Noise reduction frees resources for other, simultaneous tasks. ◦ Better auditory memory ◦ Increased speed of response to a visual task ◦ (Sarampolis, et al., 2009) Proven ability to reduce signals at specified azimuths Function less well in ◦ May or may not be “noise reduction” ◦ Distance ◦ Reverberant environment Function less well when the head is not upright Function less well when speech and noise are moving targets May be a detriment when desired signal is from sides or rear Age does not have a significant effect on directional benefit/preference, but older adults have a lower perception of benefit in the directional mode as compared with younger listeners (Wu, 2010) Solutions? ◦ Manual switching? ◦ “Smart” automatic algorithms? ◦ What makes most sense for older user? Common in contemporary hearing aids Patient may be unaware that processing is happening Automatic vs Manual Switching? Possible disadvantages? How can we better understand how the hearing aid is working ◦ To counsel patients ◦ To manipulate variables (if possible) Assists in setting expectations and in making selection COSI Hearing Demand, Ability and Need Profile SAC/SOAC Patient Expectations Worksheet ◦ Compares what situation patient is successful in or wants to be more successful in ◦ Pre-treatment success vs level of success posttreatment ◦ Including realistic expectations counseling Provide basis for counseling and setting expectations • Tool to assist in assessing – Motivation – Interest in different types of hearing aids – Budget • Helps quickly move through some of the initial decision-making – Opportunity to discuss reasonable expectations (e.g., patient with severe-profound hearing loss wants ITC hearing aids) • Patient has already considered some of the initial questions and developed answers Please list the top three situations where you would most like to hear better. Be as specific as possible How important is it for you to hear better? How motivated are you to wear and use hearing aids? How helpful do you think hearing aids will be? What is your most important consideration regarding hearing aids? Rank order the following factors with 1 as the most important and 4 as the least important. ___ Hearing aid size and the ability of others not to see the hearing aids ___ Improved ability to hear and understand speech ___ Improved ability to understand speech in noisy situations (e.g., restaurants, parties) ___ Cost of the hearing aids Do you prefer hearing aids that: ___ are totally automatic so that you do not have to make any adjustments to them. ___ allow you to adjust the volume and change the listening programs as you see fit. ___ no preference Look at the pictures (photos of hearing aid styles) of the hearing aids. Please place an X on the picture or pictures of the style you would NOT be willing to use. Your audiologist will discuss with you if your choices are appropriate for you – given your hearing loss and physical shape of your ear. How confident do you feel that you will be successful in using hearing aids. ___ Basic digital hearing aids: Cost is between $XXXX to $XXXX ___ Basic Plus hearing aids: Cost is between $XXXX to $XXXX ___ ___ Mid-level digital hearing aids: Premium digital hearing aids: Cost is between $XXXX to $XXXX Cost is between $XXXX to $XXXX Physical fit Acoustical fit ◦ Probe microphone measures with modifications in gain/output to achieve maximum audibility and safe/comfortable MPO at initial fitting? YES! ◦ Permitting overall gain/output reduction on day one? YES Just don’t forget to subsequently increase Selection/deselection of features/options ◦ i.e, how many programs does a person need on day 1? Counseling, counseling, counseling Reasonable expectations Wearing schedule? No… If you want to ensure audibility If you want to ensure that OSPL is set appropriately Yes… If you want to get the patient out the door in a hurry If you want the hearing aids to sound “comfortable, natural” from the first wearing If you are satisfied with fitting earplugs “How does that sound?” (important, but insufficient) “Aided Audiogram” (misleading, unreliable, attractive to lay-person) ◦ Inadequate and inappropriate for making hearing aid adjustments “First-Fit” (generally inadequate gain and output, generally greater insufficiency in the high frequencies, reducing Aided Intelligibility Index) Manufacturer’s proprietary fitting algorithms ◦ Where is the independent research validating? Desired Sensation Level NAL-NL1/NAL-NL2 Ample and robust independent evidence ◦ Not just for pediatric fittings Assures maximal audibility ◦ Within the limitations of the hearing aid circuit and transducers Assures safe and comfortable OSPL Can measure the effects of features ◦ Directionality ◦ Noise reduction ◦ Amplitude Compression by frequency band ◦ Frequency transposition/compression with high frequency inputs SII 75 SII 80 SII 41 SII 68 Yes! Yes! Yes! Aided Audibility Index vs “Aided Audiogram” Use of Estimated AAI in real-ear system as counseling tool Aided vs unaided speech perception Post-fitting hearing aid outcomes measures ◦ APHAB ◦ IOI-HA Counsel, counsel, counsel 1. Conduct first-fit programming using a method that prescribes gain for average input similar to that prescribed by the NAL-RP/NL1. 2. Verify the fitting using real-ear aided response (REAR). 3. Use an authentic speechlike signal (or real speech) at an input of 65 dB SPL. 4. Adjust gain/compression parameters until a match to NAL target (or similar) within 2–3 dB has been obtained at all key frequencies. Comfort ◦ Physical ◦ Acoustic Output SPL may be uncomfortably high Audibility of speech spectrum may be inadequate Occlusion effect Feedback Lack of speech clarity/poor speech perception Environmental Noise Related to auditory impairments not amenable to treatment with hearing aids Frequency, temporal and amplitude distortion ◦ Speech A primary reason why older adults stop wearing hearing aids ◦ Non-speech First, fit the right hearing aids ◦ Appropriate style and arrangement for hearing loss ◦ Selection of features necessary; avoid unnecessary features Second, program hearing aids to ensure maximal speech audibility, comfortable/safe OSPL Ensure good feedback reduction without unnecessarily reducing high-frequency audibility If gain/output reduced to accommodate initial acceptance Ensure return to maximal audibility at a future appointment as acclimatization occurs Hearing aids don’t do it all ◦ We lose credibility and patient confidence if we declare otherwise ◦ Need to clearly outline reasonable expectations Educate patient/family that some component of hearing loss is/may be central/cognitive ◦ We hear with our brains, not our ears Importance of counseling, auditory rehabilitation Additional steps patient/caregiver/spouse can take ◦ Assistive devices ◦ Regular follow-up appointments (hearing changes) ◦ Patient/family counseling ◦ Acclimatization Referral to support group • • – Important for patient and spouse/family alike Receptive strategies: Environmental manipulation • Noise • Reverberation • Distance Interactive strategies – Repeat/rephrase – Key words – Identify change in subject or topic – – Use of “Clear Speech” by communication partner – This is trainable At least familiarize patient/family with other hearing assistance technologies – Let them make the choice whether to take up Assertive ◦ “own” the hearing loss ◦ Take responsibility for successful communication Aggressive: identify behaviors that are consistent with ◦ External locus of control ◦ “it’s your fault I can’t hear” ◦ Control the conversation—never need to listen Passive: identify behaviors that are consistent with ◦ Bluff, “smile and nod” ◦ Let others be the “ears” ◦ Withdraw, deny problems Counsel patient/family how to move to assertive communication ◦ This may be quite difficult to change Accommodation to new sensory stimuli Effects are measureable and greater in high frequencies where more “new” information is provided to the brain via the ears Evidence that this is a real phenomenon ◦ Occurs over a period of time after amplification ◦ Perceptual, physiological, neurophysiological and attitudinal How to encourage patient to persevere? ◦ Importance of counseling ◦ Gradual increase in daily wear ◦ “Train your brain” ◦ Analogies—bifocals, new dental appliances etc. Possible disappointment that things aren’t perfect ◦ Unlike eyeglasses for myopia Everything is “too loud” Occlusion effect Environmental noises Low-level noise (e.g., air-conditioning) Sounds that aren’t identifiable ◦ Turn indicator in car ◦ Refrigerator motor “I’m old” One more device to fumble with ◦ Eyeglasses, dentures, cane, medications, wig, sensible shoes, wheelchair, compression stockings, adult diapers and now HEARING AIDS! Pre-occupation with minimizing how visible hearing aids are Physical Infirmities—frustration with ◦ Seeing hearing aids ◦ Manipulating controls (dexterity, fine-motor, peripheral neuropathy Improve ◦ Noise ◦ Reverberation ◦ Distance Bluetooth FM Amplified telephone, text, visual telephone (Skype, iChat) Amplification and Captioning for TV Signaling devices ◦ Phone ◦ Doorbell (Enlist the help of the child/grandchild in anything involving a computer) Don’t assume patient “can’t afford” Demonstrate devices connected to hearing aids, in real-world environments ◦ Increases confidence in hearing aids ◦ Overcomes obstacles that hearing aids along often cannot Allow patient to experience hearing success via technology ◦ Inform them of all options ◦ Let them make the decision Great improvements in QOL shown for CI in adults Under-utilized technology Audiologists may be too slow to refer ◦ “try a better hearing aid” ◦ Lack of knowledge of referral and implantation criteria ◦ Don’t want to “lose” a HA patient Hearing aids may be effective treatment for tinnitus ◦ ~50% of HI listeners with tinnitus had tinnitus relief Tinnitus causes psycho-social handicap in some cases (high THQ scores) Use of hearing aids can reduce psychosocial handicap and tinnitus-hearing handicap ◦ Counseling alone ineffective ◦ Counseling plus hearing aid use resulted in significant improvement Elderly individuals with hearing loss Assessed at baseline, 4, 8, and 12 months after hearing aid fitting. All quality-of-life areas improved significantly from baseline to 4-month post-hearing aid fittings. ◦ ◦ ◦ ◦ ◦ Social and emotional (HHIE) Communication (QDS) Depression (GDS) benefits All were sustained at 8 and 12 months Cognitive changes (SPMSQ) reverted to baseline at 12 months. Hearing aids provide sustained benefits for at least a year in these elderly individuals 431 articles Reported outcomes with hearing aids indicate they are an effective method for treating mildmoderate HL in cases where the patient is appropriately fitted and is willing, motivated, and able to use the device. Very positive QoL and speech perception outcomes have been documented in treating severe-profound presbycusis with CIs. In some studies, QoL outcomes have even exceeded expectations of elderly patients. Sprinzl & Riechelmann, 2010 Ensure maximal speech audibility Find a revenue stream in addition to hearing aids Spend as much time on… ◦ Realistic expectations ◦ Limitations of amplification ◦ Communication strategies ◦ …as on benefits of hearing aids, “new features”, “smaller size”, “cosmetically appealing” Ensure that hearing assistance technologies other than hearing aids are also provided Engage the patient in individual and/or group rehabilitation, or peer support group, or all to the extent that they are willing Our services are underutilized ◦ significant, negative, implications for communicative/QOL/cognitive outcomes ◦ Impacting a large and growing population We need to move the focus from “the device” to a program of ◦ Identification – encouraging individuals to seek services ◦ Accurate and thorough diagnosis ◦ Comprehensive rehabilitation Of which hearing aids are a necessary, but not sufficient, solution to the problem Challenges ◦ Hearing aid features are marketed prior to rigorous testing regarding efficacy ◦ Claims may be made that actually don’t stand up to study Lag between introduction of signalprocessing schemes and validation research Difficult to provide accurate information about the products offered Responsibility to acknowledge such Promote the concept that hearing aids work Provide hearing aid fittings based on best practices ◦ And that rehabilitation, including hearing aids, is in an individual’s and family’s best interests ◦ That means real-ear verification to validated targets Need to grow population of cultural/linguistic audiologists Need to educate public/physicians/mental health workers about relationship of untreated hearing loss to mental and physical health impairments Advocate for low-cost solutions for those who cannot afford hearing aids ◦ While advocating for third-party reimbursement for hearing aids Need to advocate for adequate and appropriate reimbursement for services ◦ (sales of hearing aids cannot be our sole revenue stream!)