Birmingham_Ruth_11
advertisement
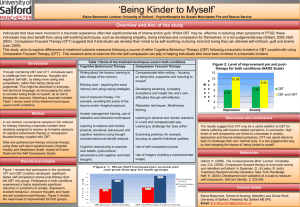
A novel CBT informed intervention for social anxiety in people recovering from psychosis. Ruth Turner, Richard White, Rebecca Lower, Lina Gega, David Fowler Acknowledgements • Everyone who has helped to make the Social Anxiety Research Clinic successful: Tony Reilly,Timothy Clarke, Felicity Waite, Evelina Medin, Kevin Lloyd, Rose Christopher, Emily Drake all of our participants,and the case managers within Central Norfolk Early Intervention Team Social Anxiety Research Clinic • • • • Describe participants Brief description of intervention Describe findings Discussion of use of virtual environments Background • Up to 70% of people recovering from psychosis experience social anxiety. • This is a significant barrier to social recovery. • Social anxiety appears to be independent of the experience of positive symptoms Screen referred cases for eligibility Enrollment and Consent Procedure Study outline Baseline Assessment (N = 48) Social anxiety Cognitive bias assessment Schema, low-level psychotic symptoms Qualitative interview Treatment Group (N=24) Allocated to immediate standard CBT (N = 12) Randomisation by randomly ordered sealed envelopes Allocated to immediate enhanced CBT (N = 12) Exclude non-consenters and cases not meeting inclusion criteria Waitlist control (N=24) Allocated to delayed standard CBT (N = 12) Allocated to delayed enhanced CBT (N = 12) Wait for 12 weeks Assess primary/secondary outcomes at the end of the intervention period (12 weeks) Assess primary/secondary outcomes at the end of the 12 week wait Assess primary outcome at 18 weeks Assess primary outcome 6 weeks following end of intervention (18 weeks) Assess primary outcome 12 weeks following end of intervention (24 weeks) Assess primary/secondary outcomes at 24 weeks Receive standard CBT for 8-12 sessions Receive enhanced CBT for 8-12 sessions Description of sample at baseline • Demographics: ; 17 male, 5 female; Average age = 26 (S.D. 6) • PANSS (data for 13 participants) average score on positive sub-scale = 10.9 (S.D. = 3.0). 46% (n = 6) of participants scored 4 or more on one or more items of the sub-scale. • BDI average score = 26.6 (S.D. 15.8) • SIAS: SIAS M (S.D.) SARC 55.6 (10.7) Social Phobia Comparison 34.6 (16.4) Non-Clinical Comparison 18.8 (11.8) Description of sample at baseline SSI SARC Psychosis Comparison Non-Clinical SSI SA M (S.D.) 17.4 (4.7) 8.6 (6.7) 4.4 (5.1) SSI P M (S.D.) 11.5 (7.6) 6.0 (6.4) 2.9 (3.6) SSI AE M (S.D.) 8.4 (5.5) 4.1 (5.7) 2.3 (3.4) SSI total M (S.D.) 37.2 (15.0) 18.7 (15.7) 9.5 (9.2) BCSS Positive Positive Self Negative Self Other M (S.D.) M (S.D.) M (S.D.) SARC 6.8 (6.4) 9.2 (7.0) 8.6 (6.5) Psychosis Comparison 10.3 (6.4) 7.2 (5.9) 10.3 (6.0) Non-clinical 10.2 (4.2) 3.5 (3.5) 10.4 (4.5) Negative Other M (S.D.) 9.0 (7.7) 9.1 (6.8) 4.0 (4) Formulation Based on Clarke and Wells model Trigger People talking Performance/ expectations on me Activates Beliefs and Assumptions I am inadequate I have to be on guard or I will be hurt Others are judgemental Perceived Social Danger Others might be talking about me I will be found out and punished Processing self as social object Focus on own anxiety Image – self sweating Safety Behaviour Avoid social and performance situations Listen in to others’ conversations Anxiety Sweating Heart racing Could not concentrate Intervention • The intervention is an assisted self-help intervention which follows four stages: – first stage included an assessment of social anxiety, goal setting and psycho-education about social anxiety. – Stage two helped patients develop an individualised CBT formulation. Patients identified their own idiosyncratic safety behaviours. – Stage three involved repeated exposure to anxiety provoking social situations in the format of behavioural experiments – The final stage focussed on maximising patients’ gains by planning further exposure-based behavioural experiments which were done either independently by the patient or with support from the care team. • Additional interventions were piloted using computerised cognitive bias modification and virtual environments. Outcomes - SIAS • Baseline SIAS scores were compared to those at the 12, 18 and 24 week follow up points. Baseline 12 weeks 18 weeks 24 weeks Therapy 60.2 (11.19) 49.7 (12.23) 42.9 (8.15) 40.4 (10.95) Waitlist 52.4 (9.19) 52.1 (13.69) 52.1 (12.76) 50.6 (13.09) Outcome - SIAS Therapy Waitlist 12 week 18 week 24 week N 10 7 8 Mean change score (SD) -10.50 (8.90) -17.29 (4.86) -16.75 (13.75) Reliable improvement (n) 6 7 6 Reliable deterioration (n) 0 0 0 Clinically significant reliable change (n) 2 1 4 N 11 9 8 Mean change score (SD) -.27 (11.34) -.56 (7.45) -1.0 (10.52) Reliable improvement (n) 3 1 3 Reliable deterioration (n) 3 1 3 Clinically significant reliable change (n) 2 1 1 Additional pilot interventions • Preliminary evidence that CBM-I sentence completion task can be used to train a more positive interpretation bias in this group. • Virtual environments are being used to provide additional situations in which behavioural experiments can be conducted. CAFÉ “sitting down waiting to order” Conclusions • Preliminary evidence that an assisted selfhelp intervention may help to reduce the level of social anxiety in people recovering from psychosis. • Psychoeducation about social anxiety and the active engagement in behavioural experiments seems to be key. Any questions? • Ruth.turner@nwmhp.nhs.uk