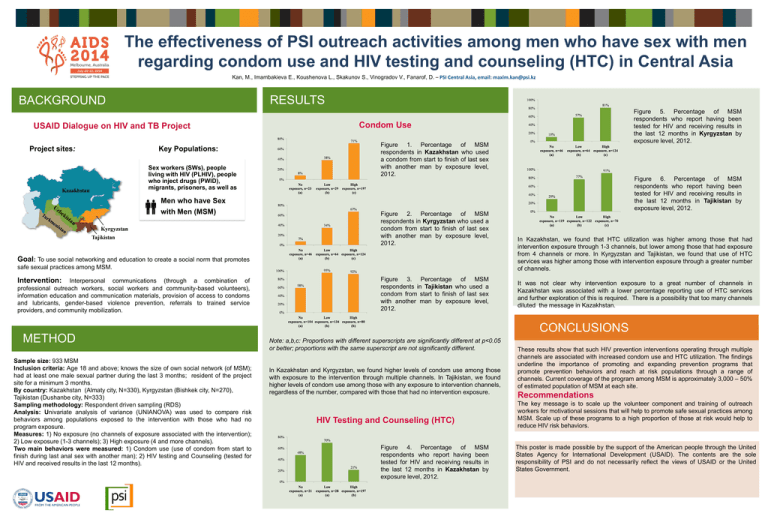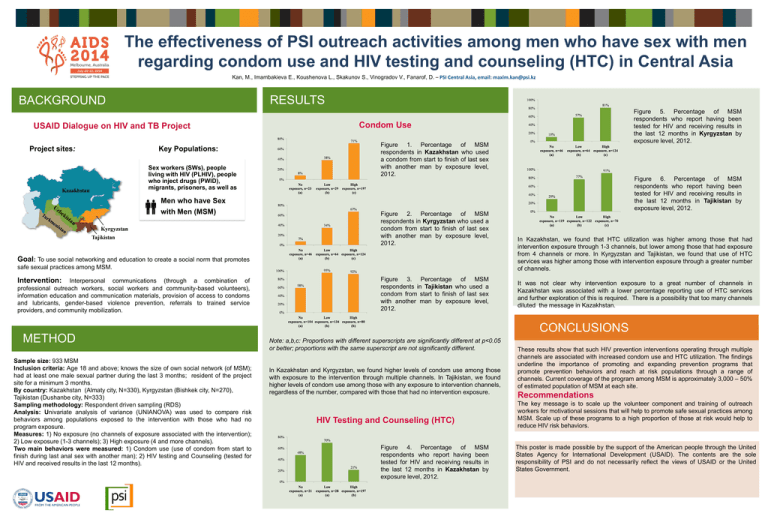
The effectiveness of PSI outreach activities among men who have sex with men
regarding condom use and HIV testing and counseling (HTC) in Central Asia
Kan, M., Imambakieva E., Koushenova L., Skakunov S., Vinogradov V., Fanarof, D. – PSI Central Asia, email: maxim.kan@psi.kz
RESULTS
BACKGROUND
USAID Dialogue on HIV and TB Project
Project sites:
Key Populations:
Sex workers (SWs), people
living with HIV (PLHIV), people
who inject drugs (PWID),
migrants, prisoners, as well as
Men who have Sex
with Men (MSM)
Condom Use
Figure 1. Percentage of MSM
respondents in Kazakhstan who used
a condom from start to finish of last sex
with another man by exposure level,
2012.
Figure 2. Percentage of MSM
respondents in Kyrgyzstan who used a
condom from start to finish of last sex
with another man by exposure level,
2012.
Goal: To use social networking and education to create a social norm that promotes
safe sexual practices among MSM.
Intervention:
Interpersonal communications (through a combination of
professional outreach workers, social workers and community-based volunteers),
information education and communication materials, provision of access to condoms
and lubricants, gender-based violence prevention, referrals to trained service
providers, and community mobilization.
METHOD
Sample size: 933 MSM
Inclusion criteria: Age 18 and above; knows the size of own social network (of MSM);
had at least one male sexual partner during the last 3 months; resident of the project
site for a minimum 3 months.
By country: Kazakhstan (Almaty city, N=330), Kyrgyzstan (Bishkek city, N=270),
Tajikistan (Dushanbe city, N=333)
Sampling methodology: Respondent driven sampling (RDS)
Analysis: Univariate analysis of variance (UNIANOVA) was used to compare risk
behaviors among populations exposed to the intervention with those who had no
program exposure.
Measures: 1) No exposure (no channels of exposure associated with the intervention);
2) Low exposure (1-3 channels); 3) High exposure (4 and more channels).
Two main behaviors were measured: 1) Condom use (use of condom from start to
finish during last anal sex with another man); 2) HIV testing and Counseling (tested for
HIV and received results in the last 12 months).
Figure 5. Percentage of MSM
respondents who report having been
tested for HIV and receiving results in
the last 12 months in Kyrgyzstan by
exposure level, 2012.
Figure 3. Percentage of MSM
respondents in Tajikistan who used a
condom from start to finish of last sex
with another man by exposure level,
2012.
Figure 6. Percentage of MSM
respondents who report having been
tested for HIV and receiving results in
the last 12 months in Tajikistan by
exposure level, 2012.
In Kazakhstan, we found that HTC utilization was higher among those that had
intervention exposure through 1-3 channels, but lower among those that had exposure
from 4 channels or more. In Kyrgyzstan and Tajikistan, we found that use of HTC
services was higher among those with intervention exposure through a greater number
of channels.
It was not clear why intervention exposure to a great number of channels in
Kazakhstan was associated with a lower percentage reporting use of HTC services
and further exploration of this is required. There is a possibility that too many channels
diluted the message in Kazakhstan.
CONCLUSIONS
Note: a,b,c: Proportions with different superscripts are significantly different at p<0.05
or better; proportions with the same superscript are not significantly different.
In Kazakhstan and Kyrgyzstan, we found higher levels of condom use among those
with exposure to the intervention through multiple channels. In Tajikistan, we found
higher levels of condom use among those with any exposure to intervention channels,
regardless of the number, compared with those that had no intervention exposure.
HIV Testing and Counseling (HTC)
Figure 4. Percentage of MSM
respondents who report having been
tested for HIV and receiving results in
the last 12 months in Kazakhstan by
exposure level, 2012.
These results show that such HIV prevention interventions operating through multiple
channels are associated with increased condom use and HTC utilization. The findings
underline the importance of promoting and expanding prevention programs that
promote prevention behaviors and reach at risk populations through a range of
channels. Current coverage of the program among MSM is approximately 3,000 – 50%
of estimated population of MSM at each site.
Recommendations
The key message is to scale up the volunteer component and training of outreach
workers for motivational sessions that will help to promote safe sexual practices among
MSM. Scale up of these programs to a high proportion of those at risk would help to
reduce HIV risk behaviors.
This poster is made possible by the support of the American people through the United
States Agency for International Development (USAID). The contents are the sole
responsibility of PSI and do not necessarily reflect the views of USAID or the United
States Government.