SNV STRATEGY 2007 - 2015 - Performance Based Financing
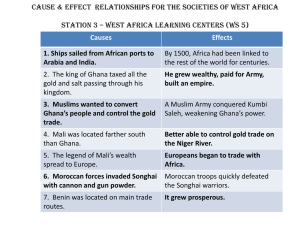
advertisement

RBF Approach Results Based Financing in Ghana: About getting started Rita Tetteh-Quarshie Rtetteh-quarshie@snvworld.org Presentation • Background of health situation (MCH) in Ghana • Planned pilot and implementation of PBF in Ghana by WB • The Wapuli case • Way forward Health spending did increase… • Recently, Ghana reached a middle income status • In Ghana health financing is close to reach Abuja Target for health spending (=15% of total government expenditure) • The per capita expenditure on health has grown from a level of $6.7 in 1996 to $13.5 in 2005 and $27 in 2008 • Around 93% of the government contribution is used to pay for salaries, limiting funding available for services and infrastructure • This is a result of the 2006 salary increase – about triplication - which was not performance based But performance is off track… Health indicators in Ghana appear off track and this affects particularly poor and rural households; i.e. • U-5 mortality is 80 deaths per 1,000 live births, with 90 in rural and 75 in urban areas. • Infant mortality rate is 49 per 1,000 live births in urban and 56 in rural areas. • The ’08 Ghana Maternal Health Survey estimates maternal death (MMR) at 451 per 100.000 live births. Deliveries attended by Skilled Provider – by Region Delivery by Skilled Provider by Region Upper East Upper West 46% 47% Northern 27% Ghana: 59% Brong Ahafo 66% Volta 54% Ashanti 73% Eastern 61% Western Central 62% 54% Greater Accra 84% Use of Modern FP Methods by Region Upper West 21% Upper East 14% Northern 6% Ghana: 17% Brong Ahafo 22% Volta 21% Ashanti 16% Eastern 17% Western Central 13% 17% Greater Accra 22% 35% unmet need among currently married women Maternal Health- Problems Accessing Health Care Reforming the Health System of Ghana? • Overall consensus: “no copy & pasting of the Rwanda model” Governance institutions and “rules of the game” do exist Governance structure is complex, preferably no new institutions Existing funding channels, etc • So, adapting to the existing Ghanaian context – but how? • Hesitation at Central level to kick-off: Agree on the principles – but how to implement them in Ghana? Sustainability: macro-economic implications? Again top-up of salaries health staff through RBF? We have already an ex-post provider payment mechanism, NHIS Again another reform? Assisted delivery is already free of charge Opportunities and threats to start-up RBF • Opportunity: existing, functioning governance structures Like NHIA: already a purchaser with a verification function (quantity and quality of services) Most facilities already accredited (Q/C) District Assembly is already (by law) in charge of health • Threat: the same existing governance structures Resistance to change the “enterprise culture” and power relations in institutions as well as in individuals Changing the “rules of the game” will not be easily Actually no clear-cut functional split of functions existing Deconcentrated system – complicating checks & balances National RBF program (MOH/ WB)) • Preparatory activities: Aide Memoire and Concept Note ready to be signed (March) • Pre-pilot (2011) to inform pilot (2012 - 2013) in Eastern and Northern Regions • Pre-pilot (500 K): regional program to prepare actors Supply-side and demand-side incentives Situational analysis, legal and financial-amin issues, Bottleneck studies household, facility, Local Govt Instrument development testing payments in 1 district (ER, E Akim), 1 in NR? • Pilot (11,5 Mio + 1 Mio for Impact Evaluation): All districts in NR and ER: 240 Facilities Institutional Framework in Ghana – hypothesis WB MOH/PPME Overvie Technical w Comm Cttee GHS NHIA World Bank MOFEP (other HIP donors) Regional Health Directorate DHMT DMHIS CSO/ NGO Providers (DH, HC, CHPS) CHAG GHS Private District Assenblee Pregnant Women POPULATION Funding Results Contracting Relation Verification results Regulation Operational research: How to introduce RBF in Ghana (SNV/KIT experiences) • Step 1: Regional workshops to identify need and common vision • Step 2: Situational analysis on baselines • Step 3: Workshops to identify and match priorities from medical and nonmedical actors to agree on institutional framework (to be tested) • Step 4: Assist health facilities to develop results-based action plans on identified priorities • Step 5: Negotiation on contract (and agree on incentives, which may come out of existing funds) • Step 6: Implementation (3 months cycle), evaluation and learning, payment of incentives, renegotiation of contract step 6 : Performance Based Financing step 5: contracting approach step 4 : develop results-based action plans at health centres & community level step 3: Identify matching priorities step 2 : situational analysis and training non-medical partners to anlyse data step 1: joint understanding of need to develop alternative institutional performance framework RBF-institutional framework, hypothesis SNV/KIT Donor s MoHealth policies, norms & standards, resource allocation MoFinanc e Funds NHIA Steering Cttee Regional Coord Council Fund Holder DMHIS/ payer Distr Ass Contractin g Regulation/ DHMT - quality ass/ accreditation - respect norms & standards - training and supervision Area Council verification facility negotiation Representatives Community patient s Perform: productivity & quality Provision of care - curative, - prevention, - promotion CSO, NGO, Universities verification household Distribution of Roles & Responsibilities Function Oversight at local level (decision-making to pay) Institutions Committee composed by: (i) District Assembly (Chair), DMHIS, DHMT, CHAG, CSO and CHAG Purchaser (contracting) District Assembly: District coordinating director to sign contracts with health facilities (HC & HP and District hospital) Verification Quantity of services in health facility: District Health Insurance Scheme (technical personnel for quality assessment will need to be determined) Verification Quality of Care in health facility: District Health Insurance Scheme and CSO Verification household level: CSO Patient tracing Consumer satisfaction Counter verification (quantity and quality) Technical Committee (central and regional); and/or external independent consulting firm Regions where PBF is being piloted by SNV Upper East Upper West Northern Brong Ahafo Volta Ashanti Eastern Western Central Greater Accra Intervention methodology • Lessons learning from experiences elsewhere • Define the building blocks for CA/ PBF in other contexts; • Site-visits to develop and adapt the working hypothesis with future local contracting partners at the operational level; • defining the institutional framework for the CA/PBF; • development of instruments – contextualizing those developed for elsewhere (Rwanda, Mali, ….) • Supporting Local Capacity Builders (NGOs) to support local actors to take up their future contracting roles; • Negotiation between contracting actors • Developing results-based action plans The case of Wapuli sub-district • Understanding performance and quality management, current theory and global practice • PBF Introductory workshop at Saboba District: DA,CSOs, NHIS,DHMT, Providers • Health baseline data was presented to stakeholders, put into result chain • Issues prioritized for the sub-district health team to work on were: -Skill delivery -ANC4+ attendance -Family planning. -Malnutrition • Issues were confirmed at a community durbar at a health sub-district. Some results (process) • Training SNV health advisors and LCB • Institutional framework for RBF developed: Who will purchase, verify, etc? • Measures taken by the clinic to increase outputs: Formation of steering committee by the community to help in educating other community A system for compensating TBAs for bringing referring pregnant women to the clinic for delivery (instant and annual) The clinic now opens everyday for ANC and FP activities and the staff work beyond their working hours. Though slow but the traditional leaders are taken measures to release pregnant women to the clinics. Results Months ANC Registration ANC Attendance Delivery 2008 2009 2010 2008 2009 2010 2008 2009 2010 September 59 83 87 269 194 279 15 13 13 October 86 62 56 253 118 222 9 13 20 November 75 66 86 260 207 246 14 7 14 December 33 89 90 181 203 284 5 7 14 January 11 77 239 15 Next steps…. • Further training of NGOs to support actors • Preparing non-medical actors: holding providers to account on results • Preparing medical actors: being creative and innovative to achieve results (enterprise culture) • Tools development (like verification: mHealth?) The approach leaves ‘room’ to address some known challenges during the process Potential challenge How these are mitigated, if RBF is applied as an approach Quality scoring on total package of activities Perverse effects – providers have a financial incentive to deliver excess on targeted services Keep contracting cycles short (so excesses can be identified soon) Equity/ inclusivenss – how to ensure access for the most vulnerable Women, PWD etc, should be included. Sustainability (financial) Understanding the national context. In Ghana using RBFincentives to top-up already high salaries would not be sustainable Carrot and stick Future policy making: make part of actual salary performance based. Integration of vertical programs Local priority setting Quantity indicators selective, quality indicators comprehensive Community involvement Decisive in local priority setting to make providers responsive to local needs and demand, in agreeing on payments Need to prepare the non-medical actors, Resilience of the system Flexibility If outputs truly answer to local needs and wants of the population So, not a model, but approach Technical sustainability…. Social sustainability… are health workers prepared for more demand Assisting clinics in developing ‘results-based action plans) Questions to the audience…. • How to finance scaling-up to national level ?!? • Assessing cost-benefit of increased transaction-costs? • Pay for results: to top-up of salaries – or to invest in conditions quality of care and « indirect costs »? • Ho to avoid the “vertical” and “centralistic” approach of RBF (focusing on MDG4,5)