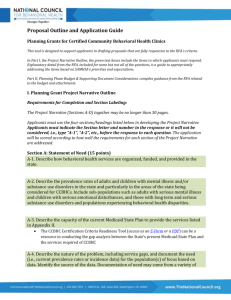
MACPAC Study of Medicaid Behavioral Health
advertisement
Washington Update November 11, 2014 Stuart Yael Gordon, J.D., NASMHPD Director, Policy and Health Care Reform 1 No Labor/HHS bill voted in House, Senate subcommittees. Mikulski did post Senate bill not voted. Continuing Resolution enacted September 17, expires December 11. GOP split. Some want full omnibus passed during lame duck, some want to extend CR until March, then enact full budget. House Appropriations will not release full budget until days before CR expires. 2 House GOP leaders announced in June that bill would move forward only with “noncontroversial” provisions (not specified), but new version still not released. Rep. Murphy continues to push for full passage. ◦ Cited Robin Williams’ August 12th suicide as evidence of need for comprehensive reform. Staff for House Energy and Commerce Chair Chairman Upton has told us “disease-specific” bill cannot move without bipartisan consensus. Original version now has 108 co-sponsors, 36 of whom are Democrats (4 Dems w/drew as sponsors). Bill likely will not move before end of post-election Lame Duck session (historic median length 33 days, shortest 3 days, longest 58 days). 3 Even if bill moves out of E&C Committee, unlikely there’s time to pass full House. Even if bill passes full House, Senate very unlikely to bring to floor, but bill would be positioned for support in 114th Congress. Budget C.R. will expire Dec. 11; either CR will be continued until March 2015 or full budget will be enacted during Lame Duck. With Republicans leading Senate, provisions of Murphy bill could pass in early 2015 as part of Budget Reconciliation Process requiring only simple majority vote of Senate (51 votes) rather than 60-vote super-majority. Byrd Rule requires provisions in reconciliation bills to be budgetary in nature (affecting revenue or spending.) Provision that doesn’t produce a change in outlays or revenue is subject to point of order that can be waived only with 60 votes. 4 H.R. 4574, “Strengthening Mental Health in Our Communities Act of 2014” Up to 63 co-sponsors, all Dems, many of whom are also co-sponsors of Murphy bill. Rep. Murphy adamantly opposes combining bills. H.R. 4574 unlikely to move this year (even out of committee), but is likely to return as Murphy alternative. 5 September 18, 2013, CMS finalizes methodology for allocating FY2014 and FY2015 DSH reductions and promises separate rulemaking for ensuing years. Implementation delayed with Congressional delays … ◦ The Middle Class Tax Relief and Job Creation Act of 2012 extended reductions to FY2022. ◦ Sec. 1204 of Bipartisan Budget Act of 2013 delayed implementation of the DSH payment cuts until FY2016 and extended reductions through FY2023. ◦ Protecting Access to Medicare Act of 2014 delayed reductions to FY2017 and extended reductions to FY2024. Result: in FY2017, aggregate DSH reductions will total $1.8B, rather than $500M originally scheduled for 1st year under ACA. 6 12 DSH bills, including one with sponsor (Baucus) gone, none moving, all already outdated by 2014 doc fix (H.R. 4302). Under H.R. 4302, Medicaid and CHIP Payment and Access Commission (MACPAC) must report to Congress annually, beginning February 1, 2016 on: ◦ Changes in the number of uninsured; ◦ Amount and sources of hospitals’ uncompensated care costs, including costs resulting from unreimbursed and underreimbursed services, charity care, or bad debt; ◦ Identity of hospitals with high levels of uncompensated care that provide access to essential community services for lowincome, uninsured, and vulnerable populations, including trauma care and public health services. ◦ State-specific analyses of the relationship between the most State DSH allotments and uncompensated care data. 7 Price Waterhouse Cooper released 9/3/14 report on admissions and uncompensated care in for-profit hospitals, comparing hospitals in 26 Medicaid expansion states (and D.C.) to those in 24 non-expansion states. ◦ 47% reduction in admissions of uninsured or self-paying patients at the hospitals in expansion states in the first half of 2014. Colorado Hospital Association (CHA) collects monthly financial and volume data for 465 hospitals in 30 states across the country in DATABANK. 15 states in database expanded Medicaid, 15 did not. June CHA Report found: ◦ When compared to the Q1 of FY 2013, there was a 30% drop in average charity care per hospital across expansion states, to $1.9M from $2.8M. 8 Proportion of charges by payer per group and average charity care per hospital. 9 17-member MACPAC has 6 vacancies opening up January 1. MACPAC, created in 2010, has never had representative from Behavioral Health provider/consumer community. NASMHPD forwarded PA Department of Public Welfare nomination of PA Medical Director Dale Adair by Sept. 5 deadline, with our support. ◦ Nomination seconded in letter from 30+ members of D.C.’s Mental Health Liaison Group and separate letter from APA. October 30, MACPAC began examining role of behavioral health in Medicaid, with eye toward two reports to Congress in April, June 2015. 10 Issues touched on in the October 30 briefing and proposed for future consideration by MACPAC members included: ◦ the high cost of treating individuals with behavioral health conditions; ◦ the prevalence and treatment of behavioral health disorders; ◦ the fact that in some states there may be three delivery systems for behavioral health conditions; ◦ what is entailed in Medicaid coverage for mental illness and substance use disorders; ◦ the sometimes conflicting responsibilities and eligibility standards of federal and state agencies providing behavioral health treatment—including HRSA, SAMHSA, DoE, and the criminal justice system; 11 Issues proposed for consideration also included: ◦ Medicaid behavioral health carve-outs and the difficulties they create, particularly where carve-out policies change frequently; ◦ barriers to service—including the IMD exclusion and provider shortages—and state steps taken to address those barriers; ◦ how the IMD exclusion interacts with mental health parity and Early Periodic Screening, Diagnosis, and Treatment (EPSDT) coverage ◦ over-prescription of psychotropic drugs to some populations; ◦ abuse of opioids; and ◦ state approaches to integrating behavioral health and other medical services, and how integration affects costs, outcomes. 12 NASMHPD, National Association of Medicaid Directors commended MACPAC on initiative. ◦ NAMD urged study of IMD exclusion. ◦ NAMSHPD urged study of role of peer support services in maintaining access in mental health and substance use treatment. ◦ ASPE said it is currently studying impact of health homes, IMD exclusion demo, supported employment. ◦ PEW Research Center said it’s looking at interrelationship between behavioral health and corrections. 13 Regulations governing HCBS residential services published January 16. Guidance on non-residential services promised, still not published. “Association of Associations” (NAMD, NASUAD, NASDDDS, NASMHPD) asked by CMS to help define service terms, beginning with “prevocational services” and “adult day services,” for inclusion in guidance on non-residential HCBS services, with 8-week deadline. o o Workgroups formed with representatives from each association. Associations want to start with existing HCBS waiver taxonomy, then modify as appropriate to reflect appropriate sites, group-specific characteristics. 14 1. October 8: SAMHSA proposed to conduct a 61- question Peer Support Worker core competencies survey and telephone interviews to help SAMHSA prepare people in recovery for the role of peer worker and subsequently evaluate the job performance of peer workers. ◦ SAMHSA would survey 100 workers and interview 20. NASMHPD Feedback submitted by November 10 deadline: Sample far too small given that 33 states reimburse under Medicaid for peer support. 15 8 state, 2 year demo under which CBHCs will be paid under a prospective payment system (PPS) to provide behavioral health services, and states reimbursed at 90% FMAP. Short turnaround for awarding of $25M in state planning grants by January 1, 2016, so no formal regulations to be published. SAMHSA, CMS will issue only guidance to states. November 12: All-Day Listening Session at SAMHSA and via phone on draft guidance on implementation of Excellence in Mental Health (“Section 223”) two-year CBHC grant program. SAMHSA drafting guidance for states to set CBHC certification standards based on H.R. 4302 language. Two weeks for filing written comments following Listening Session; November 26 deadline. CMS drafting guidance on CBHC prospective payment system, due by September 2015. CMS Listening Session to be held November 20, virtually only. 16 24-hour crisis mental health services, including emergency crisis intervention and crisis stabilization Screening, assessment, and diagnosis, including risk assessment Patient-centered treatment planning Outpatient mental health and substance use services Outpatient clinic primary care screening and monitoring of key health indicators and health risk. Targeted case management Psychiatric rehabilitation service Peer support and counselor services, family supports Services for veterans, armed forces members, particularly in rural areas. 17 McConnell says he wants repeal of individual mandate, 30-hour workweek for coverage. Full repeal unlikely – Insurers would likely oppose ◦ Wellpoint enrollment up 1.68M, half are Medicaid enrollees. Stock up 50%. Retooled as “utility” ◦ United Healthcare, which sat out 2014, all in for 2015 ◦ 57 more issuers in federal exchange. Total issuer enrollment now 248. 18 Hearing still on in Federal Court of Appeals for DC, scheduled for December 17. Question: Can subsidies be provided to enrollees through federally facilitated exchanges? 18 states just filed Amici brief in D.C. court: ◦ If two interpretations, court must accept least nonsensical ◦ No notice to participating states of threat of loss of subsidy – Constitutional violation Challengers asking DC Court to dismiss. SCOTUS expected to hear in March 2015, decide in June. 19