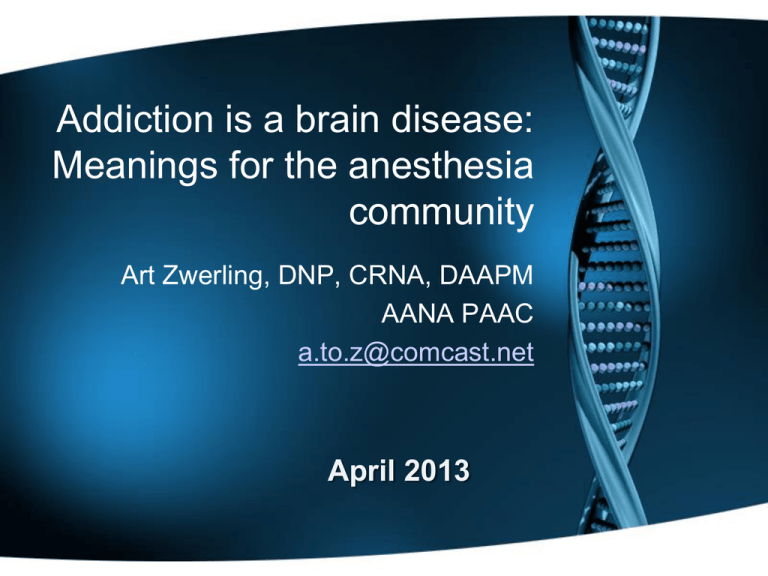
Addiction is a brain disease:
Meanings for the anesthesia
community
Art Zwerling, DNP, CRNA, DAAPM
AANA PAAC
a.to.z@comcast.net
April 2013
Grateful Acknowledgements
•
•
•
•
•
•
•
•
•
•
•
•
•
Diana Quinlan, CRNA, MA
Heather Hamza, CRNA, MS
Greg Ramplemann, CRNA
Linda Stone, CRNA, MSN
Tony Chipas, CRNA, PhD
Gary Clark, CRNA, EdD
Saundra Dockins, CRNA
Terry Wicks, CRNA, MSHS
Michael Lords, SRNA
Julie Rice, AANA
Don Bell, CRNA, DNSc
Steven D. LaRowe, Ph.D.
AANA BOD
Learning Objectives
– Inform communities of interest regarding the
antecedents, risks and consequences of
chemical dependency
– Promote awareness of the impact of CD on the
anesthesia community
– Review the basic neurobiology of chemical
dependency as a chronic brain disease.
– Reduce the incidence of chemical dependency
and the impact of CD on the nurse anesthesia
profession
History/Background
• Diana Morgan, Minnesota President
• 1983 Annual Business Meeting
Resolved: That the American Association of Nurse
Anesthetists form a task force to study the impact of
chemical dependency upon our profession and to
be a source of positive public relations concerning
chemical dependency information as it affects our
members.
Pioneers in the AANA’s Peer
Assistance and Recovering Community
Rusty Ratliff, Diana Quinlan
and many other worked to
support and find acceptance
for the recovering CRNA
community
A Rude Awakening…
• Death of Jan Stewart in 2002
• Jan Stewart Memorial Lecture
Series 2004
• Virginia Trotter Betts 2004
• AANA Blue Ribbon Wellness
Panel and establishment of the
Wellness Program 2005
• Presidential Wellness TF 2010
AANA President
1999-2000
Chemical Dependency
• Substance related disorders characterized by
chronicity and progression that threaten wellness..
• Propensity for relapse
• Transition to a chronic disease, chronic care model
• Subversion of primitive reward and anti-reward
systems
• Neuroplasticity
CRNA Statistics
• Approximately 1 in 10 CRNAs becomes addicted
during their career (Clark & Stone, 1999)
• 15.8% of CRNAs found to be dependent on
alcohol, drugs or both (Berry, 2000)
• Male CRNAs with 6 to 10 years of clinical
experience are most at risk for addiction (Bell,
1999)
• 66.7% of SRNAs with substance abuse problems
were ranked in the upper third of their graduating
class (Clark & Stone, 1999)
Drugs of Choice
• Opioids such as fentanyl and
sufentanil are the most commonly
cited abused substances by
anesthesia providers (Booth, 2002)
• CRNA studies have shown
midazolam is the most misused
controlled drug among providers
(Bell, 1999)
Drug Misuse
by Preference
Inside the OR
1.
OPIOIDS
2.
BENZODIAZEPINES
3.
4.
5.
6.
7.
Fentanyl & Sufenta (Nasal)
Midazolam (Nasal)
N2O
PROPOFOL
DISSOCIATIVE DRUGS
AGONIST/ANTAGONISTS
BARBITURATES
Bell 2007
Triad of Contributing Factors©
Drug Misuse by CRNAs
AVAILABILITY
Stress
Burnout
Fatigue
Invulnerability
Genetics
Prior
Experimentation
ACCESSIBILITY
ACCOUNTABILITY
Adapted from Bell 2007
Warning Signs
• At work during off
hours
• Isolation
• Frequent breaks
• Tardy or Absent
• Signing out more
drugs than peers
• Inappropriate
dosages, drug
choices
• Problematic alcohol
use at social
functions
Difficulty with authority
Forgetful, confused
Freq. Illness, physical
complaints
Dishonesty (trivial
matters)
Elaborate excuses
Tremors
Long sleeves, alcohol
on breath
Source: AANA Website
Causes of Addiction:
Disease Model
• Alcoholism and other addictions represent diseases
for which a certain proportion of the population is
genetically predisposed
– Developed by Dr. Benjamin Rush, late 1700’s
– Scientific credence in 1960
• Jellinek’s “Disease Concept of Alcoholism”
– Originally rejected by AMA, but now accepted
– Framework for AA and other 12 step groups
– Burgeoning support from bench research in the
neurobiology of addictions
Why Do People Take Drugs in The
First Place?
To feel
good
To have novel:
feelings
sensations
experiences
AND
to share them
To feel
better
To lessen:
anxiety
worries
fears
depression
hopelessness
Natural Rewards Elevate Dopamine Levels
% of Basal DA Output
NAc shell
150
100
Empty
50
Box Feeding
SEX
200
150
100
15
10
5
0
0
0
60
120
Time (min)
Di Chiara et al., Neuroscience, 1999.
180
Copulation Frequency
DA Concentration (% Baseline)
FOOD
200
Female Present
Sample
Number
1
2
3
4
5
6
7
8
Fiorino and Phillips, J. Neuroscience, 1997.
Mounts
Intromissions
Ejaculations
Accumbens
1100
1000
900
800
700
600
500
400
300
200
100
0
AMPHETAMINE
DA
DOPAC
HVA
200
Accumbens
Caudate
150
100
0
0
1
2
3 hr
Time After Nicotine
COCAINE
DA
DOPAC
HVA
200
100
0
5 hr
NICOTINE
Accumbens
300
% of Basal Release
250
1
2
3
4
Time After Amphetamine
% of Basal Release
400
0
% of Basal Release
% of Basal Release
Effects of Drugs on Dopamine Release
250
0
1
2
3
4
Time After Cocaine
Accumbens
5 hr
MORPHINE
Dose (mg/kg)
0.5
1.0
2.5
10
200
150
100
0
0
1
2
3
4
Time After Morphine
5hr
Di Chiara and Imperato, PNAS, 1988
Vulnerability
Why do some people become
addicted while others do not?
We Know There’s a
Big Genetic Contribution to
Drug Abuse and Addiction…
….Overlapping with Environmental
Influences that Help Make
Addiction a Complex Disease.
Biology/genes
Biology/
Environment
Interactions
Environment
Anesthesia
Biology/genes
Stress Accessibility
Accountability
Potency
Biology/
Environment
Interactions
Applicant genome
Environment
DA Receptors and the Response to
Methylphenidate (MP)
high
low
Low DA
receptor
Dopamine receptor level
High DA
receptor
As a group, subjects with low receptor levels found MP
pleasant while those with high levels found MP unpleasant
Adapted from Volkow et al., Am. J. Psychiatry, 1999.
Adaptations to reward & anti-reward
systems lead to chronic disease
Dancing with the white rabbit: A
break from the neuroscience
EMERGING THREAT: PROPOFOL
Another must read
The Misuse and Abuse of
Propofol *
Todd Monroe, Heather Hamza, Greg Stocks,
Paula Davies Scimeca and Ronald Cowan
*Substance Use & Misuse, Early Online:1–7, 2011
ISSN: 1082-6084 print / 1532-2491 online
Seminal Review Article:
Concise, Clear &
Comprehensive*
• Critical review of the current state identification,
intervention and monitoring.
• There are areas with an incredible paucity of data
such as CRNA specific outcomes
• Must read for every anesthesia educator
*The Drug Seeking Anesthesia Care Provider
Ethan O. Bryson, MD, Heather Hamza, MS, CRNA
Int Anesthesiol Clin. 2011 Winter;49(1):157-71
Evolution of the concept of the highjacked cortex
• For millennia we have grappled with the perverse
polymorphic nature of addictive processes and
the behaviors exhibited.
• Addictive behavior appears to defy logical
analysis at many levels.
• By exposing how primitive (midbrain) reward &
anti-reward system dynamics supersede higher
cognitive processes (orbitofrontal) allows us a
different perspective on the powerful, cunning, &
baffling nature of addiction.
The high jacked cortex
• It certainly can look
like demonic
possession
• The behavior is
puzzling, baffling,
perplexing and
frightening.
• Once complete
abstinence is achieved
an effective
denialectomy is
possible.
Addictive Thinking Revisited
• Normal Logic: All trees have leaves, this has
leaves, this may be a tree.
• Neurotic Logic: All trees have leaves, this has
leaves, this may be a tree and when fall comes
I’m going to pick up each leaf.
• Psychotic Logic: All trees have leaves, this has
leaves therefore I am a tree.
• Addictive Logic: All trees have leaves, this has
leaves therefore I need a drink/drug.
The Neurobiology of
Addiction
Steven D. LaRowe, Ph.D.
Center for Drug and Alcohol Programs
Medical University of South Carolina
Substance Abuse Treatment Center
Ralph H. Johnson VAMC
Addictive Behavior = Survival
Behavior Gone Awry
• Over the course of evolution, we have
developed circuitry in our brains that have
promoted our survival
• Drugs of addiction activate this “survival
circuitry” and with chronic use, essentially
take it over
• In the late stages of addiction, an individual
is basically a “survivalist” doing whatever it
takes to acquire and use drugs regardless
of the costs
Addiction: Hijacking the Basic
Survival Circuitry
Basic Neurobiology
•
•
•
•
Acquisition
Progression
Neuroplasticity
Chronicity & relapse
ADDICTION IS A DISEASE OF THE BRAIN
as other diseases it affects the tissue function
Decreased Brain Metabolism in Drug Abuse Patient
High
Control
Cocaine Abuser
Decreased Heart Metabolism in Heart Disease Patient
Low
Healthy Heart
Diseased Heart
Sources: From the laboratories of Drs. N. Volkow and H. Schelbert
Addiction Changes Brain Circuits
Stop & Go Systems Awry
Non-Addicted Brain
Addicted Brain
Control
Control
Saliency
Drive NOT
GO
Memory
Saliency
Drive GO
Memory
Source: Adapted from Volkow et al., Neuropharmacology, 2004.
Dopamine and Glutamate Revisited
Addictive Thinking Revisited
• Normal Logic: All trees have leaves, this has
leaves, this may be a tree.
• Neurotic Logic: All trees have leaves, this has
leaves, this may be a tree and when fall comes I’m
going to pick up each leaf.
• Psychotic Logic: All trees have leaves, this has
leaves therefore I am a tree.
• Addictive Logic: All trees have leaves, this has
leaves therefore I need a drink/drug.
Neurobiological Basis
• Addiction: a condition in which behavior that can function both to
produce pleasure and to reduce painful effects is employed in a
pattern that is characterized by two key features: (1) recurrent
failure to control behavior and (2) continuation of the behavior
despite significant harmful consequences (Goodman,2007).
• Dependence: Emergence of a negative emotional state produced
by negative reinforcement mechanisms (e.g. dysphoria, anxiety,
irritability) when access to the drug is prevented (Koob, 2009).
• Salience: Prioritization of a stimulus in the environment based on
its relative importance to the organism’s overall well being or
survival. Readily influenced by long-term memory stores or
anticipatory mechanisms. *important concept
• Hedonism: Intrinsic value of pleasure. The only value is how
much good is produced and how little pain is experienced
(Encyclopedia Britannica, 11th ed., 1911).
Allostasis
• A state of chronic deviation of the regulatory
system from its normal operating level (homeostasis)
(Koob et al. 2008).
• A continuous readjustment of all parameters toward
a new set point illustrates the construct of this
mechanism as “stability through change” (Koob et al.
2008).
• Repeated challenges, such as the case with drugs
of abuse, lead to attempts of the brain via molecular,
cellular and neurocirciutry changes to maintain
stability (Koob et al. 2008).
• The residual deviation from normal brain reward
systems threshold is termed the allostatic state (Koob
et al. 2008).
Opponent Processes
• Reward system (s) involved in the acquisition of
addictions
• Anti-reward system (s) involved in the
maintenance of addictions
• Neuroplasticity appears to underpin the chronicity
of addictions and propensity for relapse
Neurocircuitry of Addiction
George F. Koob,
& Nora D. Volkow
Neuropsychopharmacology REVIEWS (2010) 35,
217–238 & 2010 Nature Publishing Group
Neuroplasticity Progression
Green= Go Preoccupation Compulsivity
Blue= Binge Intoxication
Red= Withdrawal Stress Dysphoria
•Figure 5. Neurocircuitry schematic illustrating the combination of neuroadaptations in the brain circuitry for
•the three stages of the addiction cycle that promote drug-seeking behavior in the addicted state. Note the activation of the
•ventral striatum/dorsal striatum/extended amygdala driven by cues
•through the hippocampus and basolateral amygdala and stress through the insula. The frontal cortex system is compromised,
•producing deficits in executive function and contributing to the incentive salience of drugs compared to natural reinforcers.
•Dopamine systems are compromised, and brainstress systems such as CRF are activated to reset further the salience of drug
• drug-related stimuli in the context of an aversive dysphoric state
Dark Side of Addiction
• The transition to a progressive, chronic and
relapsing begins with the euphoric effects of
these potent intoxicants on primitive reward
systems that underpin basic biological survival
drives.
• Ultimately maintenance of the addiction cycle is
mediated by persistent Neuroplasticity in the
reward and anti-reward systems.
• Avoidance of dysphoric states/withdrawal
symptoms become the most powerful drivers of
persistent addictive behavior.
The Dark Side of Addiction
• Development of an aversive emotional state that
drives negative reinforcement of addiction (Koob et al.
2008).
• Consists of key motivational elements: chronic
irritability, emotional pain, difficulty identifying feelings
(alexithymia), malaise, dysphoria, loss of motivation for
natural rewards (Koob et al. 2008).
• Two processes involved:
–Loss of reward systems
–Recruitment of brain stress or anti-reward
systems
(Koob et al. 2008)
Neurobiological Basis
• There are two key areas of brain arousal and stress
mechanisms
in the development of dependence:
–Neuropharmacological actions of
corticotropin-releasing factor (CRF)
the
–Norepinephrine in the extrahypothalamic systems in
extended amygdala
• Central nucleus of the amygdala
• Bed nucleus of the stria terminalis
• Transition area in the shell of the nucleus accumbens
(Koob, 2009)
Common pathway
Addiction is Similar to Other
Chronic Illnesses Because:
•
Recovery from it--protracted abstinence
and restored functioning--is often a longterm process requiring repeated
treatments
•
Relapses to drug abuse can occur during
or after successful treatment episodes
•
Participation in self-help support
programs during and following treatment
can be helpful in sustaining long-term
recovery
50 to 70%
50 to 70%
80
70
60
50
40
30
20
10
0
30 to 50%
10
090
40 to 60%
Percent of Patients Who Relapse
Relapse Rates Are Similar for Drug
Addiction & Other Chronic Illnesses
Drug
Addiction
Type I
Diabetes
Hypertension
Asthma
McLellan et al., JAMA, 2000.
Relapse and Relapse Triggers
•
•
•
•
Cue based- People Places Things
Exposure- Iatrogenic Mediated
Stress- Alterations in CRF Responsiveness
Defining the dysphoric experience
Stress Susceptibility Model of Addictions
Certain people, due to a variety of biologically-based
factors:
•
genetics, neurocognitive functioning, stress response
•
may be predisposed to developing an addiction to
something, be it alcohol, heroin, gambling, sex or
other process addictions
•
if the right stressor, or combination of stressors,
affects the person at a critical time, the person may
be more inclined to develop an addiction.
The Stress Hormone Cycle
Hypothalamus
CRF
Pituitary
Gland
ACTH
CRF:
Corticotropin
Releasing
Factor
Adrenal
Glands
Kidneys
CORTISOL
Anxiety
DRUG USE
(Self-Medication)
CRF
CRF
STRESS
Anxiety
What Role Does Stress Play
In Relapse to Drug Use
What Happens When A Person
Stops Taking A Drug?
Anxiety
Prolonged
DRUG
CRF
USE
Abstinence
RELAPSE
Relapse Triggers: Distinctions
• Stress appears to mediate reinstatement of
drug seeking via CRF1 receptor activity in
the BNST.
• Contextual relapse appears to be mediated
via prefrontal and extended amygdala
Glutaminergic afferents to NAC shell.
• Priming (drug exposure) induced relapse
appears to be mediated via direct increases
in Dopaminergic tone via the VTA to the
NAC core.
Sinha R et al Psychological stress, drug-related cues, and cocaine craving.
Psychopharmacology 2000; 152:140-148
Relapse Triggers: Limbic Kindling
of Craving
• Glutaminergic prefrontal afferents from the
prefrontal cortex appear to mediate the
experience of craving induced by contextual
exposure as evidenced by fMRI.
• Susceptibility to exaggerated responsiveness on
exposure to drug related cues appears to persist.
Relapse Triggers: Stress
• Stress appears to mediate reinstatement of
drug seeking via CRF1 receptor activity in
the BNST
• The mediation of cue associated
reinstatement appears to be via
Glutaminergic prefrontal inputs into the NAC
• Drug (priming) induced reinstatement
appears to induce direct Dopaminergic
release between the VTA and NAC.
Sinha R et al Psychological stress, drug-related cues, and cocaine craving.
Psychopharmacology 2000; 152:140-148
Relapse Cycle and
Recommendations
Chronic Disease Models
• DM as a model
a. We know medication or diet non compliance
can lead to relapse.
b. We know that physiologic stressors such as a
infective process can lead to an exacerbation.
c. We know that compliance with treatment
regimen is the key to disease management!
Case Study: Martin
• Expert cardiothoracic CRNA
• Voted favorite preceptor
• Played viola in a string
quartet
• Adored husband and father
• Drug of choice: Fentanyl
Failed Re-entry
• Often it is a unfortunate confluence of
circumstances combining stress, failed
recognition of place preference and or exposure
to kindling cues that leads to relapse.
• Recognition of potential relapse triggers and
scenarios are critical to successful re-entry.
• Timing and assessing for readiness for reentry in
addition to relapse prevention strategies and
resources is also critical to success.
• Emphasis should be on getting it right the first
time!
People, Places, Things
Effectiveness of Treatment &
Relapse Prevention
Recovery
• According to the Betty Ford Institute,
recovery is defined as a voluntary
maintained lifestyle characterized by
sobriety, personal health, and living with
respect for yourself and those around you.
• Recovery is an ongoing process…
…NOT a
cure.
Over-riding principles
•
•
Our primary focus needs to be on prevention:
a. screening of applicants and identifying and
educating those at high risk
b. toxicology screening
c. increased accountability/decreasing ease of
access
Once we have identified the SRNA/CRNA with a
CD the focus is:
First we save lives and then downstream
when and where appropriate we may
cautiously help resurrect careers.
Take Homes
• CD is a chronic disease with similar compliance and
relapse issues to other chronic diseases such as DM
and HTN.
• Chronicity and relapse potential can be explained by
persistent neuroplastic alterations in the CNS.
• New pharmacotherapy strategies may assist as a
part of a multimodality approach to increase long
term recovery in some cases.
• We need to take the long view and focus on relapse
prevention!
References
• Auer JA: Learning mechanisms in addiction:
synaptic plasticity in the ventral tegmental
area as a result of exposure to drugs of
abuse. Annu Rev Physiol 2004, 66:447-475.
• Gardner E - What we have learned about
addiction from animal models of drug selfadministration Am J Addict 2000;9:285-313
References
• Faleiro LJ, Jones S, Kauer JA: Rapid synaptic
plasticity of glutamatergic synapses on dopamine
neurons in the ventral tegmental area in response
to acute amphetamine injection.
Neuropsychopharmacology, 2004, 29, 2115-2125
• Fattore,L., Spano, S., Deiana,S., Melis, V. Cossu,
G., Fadda,P. & Fratta, W. An endocannabinoid
mechanism in relapse to drug seeking: A review of
animal studies and clinical perspectives Brain
Research Reviews, In Press, Corrected Proof,
Available online 12 July 2006
References
• Kauer, J. A.: Learning Mechanisms in Addiction:
Synaptic Plasticity in the Ventral Tegmental
Area as a Result of Exposure to Drugs of Abuse
Annu. Rev. Physiol. 2004. 66:447–75
• Kim JA, Pollak KA, Hjelmstad GO, Fields HL: A
single cocaine exposure enhances both opioid
reward and aversion througha ventral tegmental
area-dependent mechanism. Proc Natl Acad Sci
USA 2004, 101:5664-5669.
References
• Nestler, E J: Molecular basis of long-term plasticity
underlying addiction. Nat Rev Neurosci 2001;
2:119–128;
• Nestler, E J: Molecular Biology of Addiction. Am J
of Addictions 10:201-217, 2001
• Nestler, E J, Malenka, R C: Biotechnology:
The Addicted Brain, Scientific American, April 2004,
retrieved online on the WWW at:
http://www.sciam.com/article.cfm?articleID=0001E632-978A-1019978A83414B7F0101&sc=I100322 on 7-20-06.
References
• Sinha R et al Psychological stress, drugrelated cues, and cocaine craving.
• Psychopharmacology 2000; 152:140-148
• Volkow ND, Wang G-J, Ma Y, Fowler JS,
Zhu W, Maynard L, Telang R, Vaska P, Ding
Y-S, Wong C, Swanson JM: Expectation
enhances the regional brain metabolic and
the reinforcing effects of stimulants in
cocaine abusers. J Neurosci 2003;
23:11461–11468
References
• Volkow ND, Fowler JS, Wang GJ, Swanson
JM: Dopamine in drug abuse and addiction:
results from imaging studies and treatment
implications. Mol Psychiatry, 2004, 9:557–
569.
• Volkow ND, Wang GJ, Telang F, Fowler JS,
Logan J, Childress AR, Jayne M, Ma Y,
Wong C: Cocaine cues and dopamine in
dorsal striatum: mechanism of craving in
cocaine addiction. The Journal of
Neuroscience, June 14, 2006, 26(24):65836588
Resources
• AANA PEER ASSISTANCE:
http://www.aana.com/peerassist.aspx
• AIR (Anesthetists in Recovery):
a.to.z@comcast.net or 215-635-0183
• AANA Wellness:
http://tinyurl.com/6du96lj