Unique Needs of the Elderly Hearing Impaired Patient
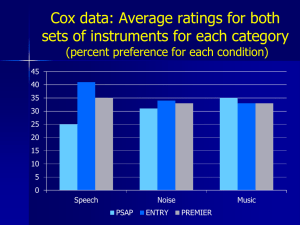
advertisement

Things We Can Do To Better Meet The Needs Of Our Hearing Impaired Patients Robert W. Sweetow, Ph.D. University of California, San Francisco The brain must…… • • • • • Detect Discriminate Localize Segregate auditory figure from ground Perceptually learn new as well as familiar auditory dimensions • Recognize and identify the source Phillips, 2002 Problems for older listeners • No problem in ideal listening conditions – – – – – Quiet One talker Familiar person Familiar topic, situation Simple task, focused activity • Difficulty in non-ideal listening conditions – – – – – – Noise Multiple talkers Strangers New topic, situation Complex task, many concurrent activities Fast pace Perceptual and cognitive declines (resource limitations) in elderly • Speed of processing • Working memory • Attentional difficulties (noise, distraction and executive control) Wingfield and Tun, 2001Seminars in Hearing Threshold elevation can account for nearly all of the changes in speech perception with age (in quiet or in less demanding listening environments.) Humes 1996 In complex perceptual tasks, older listeners are more likely to demonstrate suprathreshold deficits in addition to the effects of reduced audibility. It is less certain exactly what factors contribute to these deficits. Pichora-Fuller & Souza 2003 Impact of aging on speech perception • Even in the absence of hearing loss, older subjects require 3-5 dB higher SNR than young listeners (Schneider, Daneman and Murphy, 2005). • Older subjects with normal hearing perform approximately the same as young hearing impaired subjects (Wingfield and Tun, 2001) Disadvantage of elderly in SNR for difficult sentence material (PL = Predictability low; PH = Predictability high) Frisina and Frisina, 1997 Critical Bandwidth increases with Aging (lack of lateral inhibition) Sommers and Gehr, 1997 Brainstem changes • In noise, brainstem and midbrain blood flow increases to a greater degree in young listeners than in older listeners • Gamma aminobutyric (GABA) diminishes in older (animals) Binaural interference “Difficulty with bilateral amplification in some elderly patients might be attributable to “age-related progressive atrophy and/or demyelination of corpus callosal fibers, resulting in delay or other loss of the efficiency of interhemispheric transfer of auditory information.” Chmiel et al (1997) Age-related Hearing Loss It is likely that peripheral, age-related changes result in a partial deafferentation of the central auditory processor. This result in a series of plastic/pathologic compensatory changes including a down-regulation of inhibitory function (Caspary et al., 1990, 2008; Eggermont and Roberts, 2004; Sörös et al.,2009). The change in inhibitory function, at the level of A1, has a negative impact on the processing of simple and complex stimuli in the elderly. Cortical network effects in Aging “Consistent with the decline-compensation hypothesis, we found reduced activation in auditory regions in older compared to younger subjects, while increased activation in frontal and posterior parietal working memory and attention network was found. Increased activation in these frontal and posterior parietal regions were positively correlated with behavioral performance in older subjects, suggesting their compensatory role in aiding older subjects to achieve accurate spoken word processing in noise.” Wong et al. 2009; Neuropsychologica Young brain activity is more lateralized Old brain activity is more distributed Listening, Comprehending, Communicating • Stress during auditory processing draws mental resources away from higher levels of processing • Making listening easier by improving input will have secondary benefits to higher level processing Possible cognitive factors in aging Knowledge is preserved and context is helpful but there are problems with ….. • • • • • Slowing Working memory Attention (inhibition of distracters) Less automatic processing More trouble coordinating sources of information All are cognitive consequences if sensory (or motor) abilities are reduced. Hypothetical Interaction • Poor hearing but good memory = 25% loss • Poor memory but good hearing = 25% loss • Resultant loss could be only 50% but usually is more because the impaired memory needs full sensory input (hearing) in order to only create a 25% loss and the poor hearing creates a 25% loss only if the memory is good enough to help fill in the gaps Five Things We Can Do to Better Meet the Hearing Needs of Older People - Overview • 1) Develop a better clinical testing protocol to define the elderly patient’s global communication needs • 2) Match technology to the needs (and abilities) of the patient • 3) Integrate the patient’s social support structure into rehabilitation • 4) Extend rehabilitation beyond hearing aids • 5) Employ effective methods to enhance compliance 1. Develop a better clinical testing protocol to define the elderly patient’s global communication needs What constitutes a “typical” hearing aid evaluation? • • • • Pure tone audio Monosyllabic speech testing in quiet Informational counseling Sometimes…LDLs, MCLs, and RECDs, sentence recognition in noise • Perhaps other diagnostic tests such as OAEs Elements of Communication (Kiessling, et al, 2003; Sweetow and Henderson-Sabes, 2004) Potential impediments to achieving mastery of these elements • Hearing loss • Neural plasticity and progressive neurodegeneration • Global cognitive decline • Maladaptive compensatory behaviors • Loss of confidence Are we really testing communication? Current speech perception tests…. • Don’t take the contextual nature of conversation into account • Don’t take the interactive nature of conversation into account • Don’t allow access to conversational repair strategies that occur in real life Flynn, 2003 The biggest mistake we currently make may be… • Making hearing aids the focus of our attention, when the focus should be… • Enhancing communication How to do it? • All patients should be told at the outset of the appointment (even during the scheduling) that they will be receiving: – a communication needs assessment (CNA) and – an overall individualized communication enhancement plan that will consist of… • • • • • Education and counseling communication strategies hearing aids and / or ALDs individualized auditory training group therapy Relevant domains for assessment • • • • • • • • • • • Communication expectations and needs Sentence recognition in noise Tolerance of noise Ability to handle rapid speech Binaural integration (interference) Cognitive skills (working memory, speed of processing, executive function) Auditory scene analysis Perceived handicap Confidence / self-efficacy Vision Dexterity Communication Needs Assessment Measures beyond the audiogram that can be used to define residual auditory function. Objective procedures • QuickSIN • BKB-SIN • Hearing in Noise Test (HINT) • Listening in Spatialized Noise Sentences (LiSN-S) • Acceptable Noise Levels (ANL) • Binaural interference • Dichotic testing • Listening span (Letter Number Sequencing) • TEN • Rapid (compressed) speech test • Speechreading • Dual-tasking • Need for screening measures Communication Needs Assessment Measures beyond the audiogram that can be used to define residual auditory function. Subjective measures • Hearing Handicap Inventory for the Elderly – Screening HHIE-S • Communication Scale for Older Adults (CSOA) • Communication Confidence Profile or Listening Self Efficacy Questionnaire • Communication partner subjective scales (SAC and SOAC) Combined (objective and subjective) methods • Performance Perceptual Test (PPT) Communication Confidence Profile Please circle the number that corresponds most closely with your response for each answer. If you wear hearing aids, please answer the way that you hear WITH your hearing aids. Sweetow, R and Sabes J. Hearing Journal: (2010); 63:12 ;17-18,20,22,24. 1. Are you confident you can understand conversations when you are talking with one or two people in your own home? 2. Are you confident in your ability to understand when you are conversing with friends in a noisy environment, like a restaurant? 3. In order to hear better, how likely are you to do things like moving closer to the person speaking to you, changing positions, moving to a quieter area, finding better lighting, etc? 4. If you are having trouble understanding, how likely are you to ask a person you are speaking with to alter his or her speech by slowing down, repeating, or rephrasing? 5. How sure are you that you are able to tell where sounds are coming from (for example, if more than one person is talking, can you identify the location of the person speaking?) 6. Are you confident that you are able to follow quickly-paced conversational material? 7. Are you confident that you can focus on a conversation when other distractions are present? 8. Are you confident that you can understand a person speaking in large rooms like an auditorium or house of worship? 9. In a quiet room, are you secure in your ability to understand people with whom you are not familiar? 10. In a noisy environment, are you confident in your ability to understand people speaking with whom you are not familiar? 11. Are you confident that you can switch your attention back and forth between different talkers or sounds? 12. If you are having difficulty understanding a person talking, how likely are you to continue to stay engaged in the conversation? CCP interpretation • • • • 50+ = Confident 40-50 = Cautiously certain 30-39 = Tentative Below 29 = Insecure 2. Match technology to the needs (and strengths) of the patient • Measure state of readiness “How important is it for you to improve your hearing right now?” • Identify vital factors necessary to achieve success including dexterity • Don’t oversell; cost of hearing aids • Use appropriate features – Automatic (not manual telecoil) – Datalogging (allow for nap time) – Avoid multiple programs, including mute Hearing aid patients by age 70 60 50 40 % 30 20 10 0 65+ 45-65 30-44 18-29 <18 Age (years) From Strom, Hearing Review, 2001 Requirements for trying amplification • Problems need to be solved • Emotional needs to be addressed Assessing Motivation • Source : internal vs. external • Level: handicap perception • desire to rehabilitate • Don’t fit an unmotivated patient Tools to get there • • • • • • • Help patients tell their stories Clarify the problems Help patients challenge themselves Set goals Develop a plan Implement the plan Conduct ongoing evaluations Egan, 1998 Returns and exchanges average as high as 20% for hearing aids…….Blaming failure on a single factor is too simplistic Failure is a product of: • inaudibility • poor benefit/cost ratio • unrealistic expectations and inadequate counseling • neural plasticity • cognitive changes • poor listening habits What hearing aids don’t do • • • • • • • resolve impaired frequency resolution rectify impaired temporal processing undo maladaptive listening strategies Provide proper localization cues* “properly” reverse neural plastic effects correct for changes in cognitive function meet “unrealistic” expectations Probe Microphone Measures • Still relevant? • Issues with open fit hearing aids • Counseling implications Do prescriptive formulas work for older people? • Testing without aid of visual cues • Vision testing Client Oriented Scale of Improvement COSI • Self-report questionnaire requiring patient to list 5 listening situations in which help with hearing is required. Post-rehab, the reduction in disability and the resulting ability to communicate in these situations is quantified. • Takes less than 5 minutes of patient time, 2 minutes professional time for interpretation Expectations vs. Goals • Expectations has a product orientation – Patient assumes passive role – Whatever goes wrong is the professional’s fault • Goals has a rehabilitation orientation – Patient assumes active role – Patient shares in the process Characteristics of Amplification Tool COAT • 9-item measure of non-audiologic information to determine if technology is required. • Takes 3 minutes of patient time, 2 minutes professional time for interpretation Characteristics of Amplification Tool (COAT) Newman and Sandridge • Assesses – – – – – Motivation Expectations Preferences Cosmetics Cost considerations http://www.audiologyonline.com/management/uploads/articles/sandridge_COAT.doc Look at the pictures of the hearing aids. Please place an X on the picture or pictures of the style you would NOT be willing to use. Your audiologist will discuss with you if your choices are appropriate for you - – given your hearing loss and physical shape of your ear. Mini BTE How will your patient (and you) assess outcome? • • • • • • • • • Hearing soft sounds Louder perception Understanding speech in noise Listening effort (elevators don’t make travel from floor 1 to floor 20 more effective, but they do make it easier) !!!!! (Irv Hafter) End of day fatigue Use of new strategies Quality of life Benefit or satisfaction RFC 3. Integrate the patient’s social support structure into rehabilitation • Identify communication partners and insist on their collaboration (including discussion of communication strategies and home acoustics) • Senior outreach programs • Group therapy • Recognize need for outside referrals Perspective of an older adult who lives with hearing loss • “When you are hard of hearing you struggle to hear; • When you struggle to hear you get tired; • When you get tired you get frustrated; • When you get frustrated you get bored; • When you get bored you quit. 4. Extend rehabilitation beyond hearing aids • Group therapy • Individual therapy Definition of an auditory processing disorder Jerger and Musiek, 2000 • An auditory processing disorder is a deficit in the processing of information in the auditory modality. It may be related to difficulty in listening, speech understanding, language development, and learning. These problems can be exacerbated in unfavorable acoustic environments. • What does a peripheral disorder do????? Does peripheral hearing loss lead to central auditory dysfunction If so, can anything be done to compensate? So why should AT be expected to produce benefit? • Acuity and sensitivity are lower level functions • Higher level functions (i.e. speech in noise) require more complex (hierarchical) processing (such as hemifields and temporal analysis) that may utilize multiple channels of perceptual processing not governed by critical bands What happened to Aural Rehabilitation? • declined because outcome measures concentrated on auditory training and speechreading and didn’t consider emotional and psychological by-products • boring? • too speech pathology like? • too time consuming? • lack of reimbursement Aural (auditory, audiologic) rehab…… Should NOT be considered an add-on! Incorporate it at the very beginning Repair Strategies (synthetic) • • • • • • • • • Repeat all or part of message Rephrase message Elaborate message Simplify the message Indicate the topic of conversation Confirm the message Write the message Fingerspell the message Nonspecific repairs: – What? Huh? Pardon? » Tye-Murray 1998 Group AR • Active communication education program (Hickson, 2007) • Learning to Hear Again (Wayner and Abrahamson, 1996). • Mayo Clinic program (Hawkins, 2004) LACE (Listening and Communication Enhancement) • Cognitive – Auditory Working Memory – Speed of Processing • Degraded and competing speech – Background noise – Compressed speech – Competing speaker • Context / Linguistics • Interactive communication All of the above are designed to enhance listening and communication skills and improve confidence levels Difference in Average CS Score 1st to 4th Quarter Difference in Average S/B Score 1st to 4th Quarter (dB SNR) (dB SNR) 0 -5 -10 10 10 5 5 0 0 (dB SNR) 5 Difference in Average TC Score 1st to 4th Quarter -5 -10 -15 10 20 30 40 50 60 -30 0 70 10 20 30 40 50 60 70 Subject Subject Difference in Average TW Score 1st to 4th Quarter Difference DifferenceininAverage Average TW MW MWScore Score 1st – 1sttoto4th 4th Quarter quarter 3 1 2 0 (dB SNR) (dB SNR) -25 -25 0 1 0 -1 -2 -4 -2 0 10 20 30 40 Subject 50 60 70 0 10 20 30 40 Subject 0 10 20 30 40 Subject -3 -1 -15 -20 -20 -15 -5 -10 50 60 70 50 60 70 Why do individuals with similar losses differ so much? • Subtle reorganization could produce diverse presentations by scattering the deficit in neural space • Individuals’ brains differ (i.e. variations in fissural patterns and propensities for adaptation and recovery) Why audiologists don’t recommend comprehensive aural rehabilitation • Belief that hearing aids alone are adequate • Lack of belief in outcome measures • Belief that additional resources (time, money) are required • Lack of reimbursement • Reluctance to ask patients to spend more time or money • Inertia • Laziness The biggest unresolved questions • Will audiologists recommend it? – Impact on return for credit rate? • Will patients do it? – Cost of effort – They do for physical therapy • Why? – MD recommendation – Immediate modeling of therapy after surgery 5. Employ effective methods to enhance compliance Reasons patients don’t comply • Denial of the problem • The cost (money, time, risk of failure) of the treatment • The difficulty of the regimen • The unpleasant outcomes or side-effects of the treatment • Lack of trust in the professional • Apathy • Previous negative experience More reasons • Symptoms improve before treatment is finished • Life-style changes are too hard to make • Work and family demands interfere with following the therapy correctly • Patients come to identify the treatment with their illness Suggestions • Compliance generally increases if patients are given clear and understandable information about their condition and progress in a sincere and responsive way • Simplify instructions and treatment regimen as much as possible. • Have systems in place to generate treatment and appointment reminders LACE CE and Compliance Percent of patients uploading at least 10 sessions (%) 50 40 * Patients training at home may choose not to upload data 30 20 10 0 In Clinic At Home Where Patient Completed Session 1 Thanks for Listening