Personality Disorders Dr C Murton 25th Oct 2013
advertisement
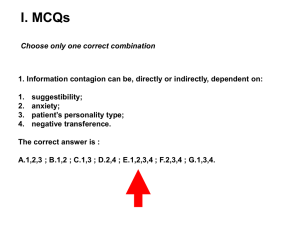
MRCPsych course CT2-3 General adult module Personality Disorders ‘You either love them or you hate them’ Dr Claudia Murton ST5 general adult and liaison psychiatry Learning objectives? Mine are: • Cover background information on aetiology, diagnostic criteria(ICD10 and DSM IV), treatments • Discuss case examples if time. • Exam practice; CASC role play and discussion Yours?: Definitions: ICD 10: Personality disorder represents extreme or significant deviations from the way in which the average individual in a given culture perceives, thinks, feels and particularly, relates to others. Behaviour patterns tend to be stable and to encompass multiple domains of behaviour and psychological functioning. They are frequently, but not always, associated with various degrees of subjective distress and problems of social performance Classification: ICD vs DSM DSM V: AXIS II disorders Cluster A: paranoid, schizoid, schizotypal Cluster B: antisocial, borderline, histrionic, narcissistic Cluster C: avoidant, dependent, obsessive-compulsive Personality Disorder NOS ICD 10 F60.0 Paranoid PD F60.1 Schizoid PD F60.2 Dissocial PD F60.3 Emotionally unstable PD F60.4 Histrionic PD F 60.5 Anankastic PD F60.6 Anxious (avoidant) PD F60.7 Dependent PD F60.8 Other specific PD F60.9 PD unspecified Differences between ICD and DSM? •Names •Inclusions and exclusions Prevalence (community sample by Coid) Personality disorder % of population Antisocial 0.6-3.0 Borderline 0.7-2.0 Narcissistic 0.4-0.8 Histrionic 2.1 Paranoid 0.7-2.4 Schizoid 0.4-1.7 Schizotypal 0.1-5.6 Avoidant 0.8-5.0 Dependent 1.0-1.7 Compulsive 1.7-2.2 Any 4.4-13.0 Aetiology: Nature or Nurture? •Attachment disorders? “I hate you…don’t leave me!” • Biologically based? Temperament Constitutionally based individual differences in emotion, motor, reactivity and self-regulation consistent across situations and over time Temperament is biologically based: Heredity, neural, and hormonal factors affect response to the environment. Temperament can be modulated by environmental factors e.g. parental response: Rutter M, Bjpsych 1987 150: 443-458 Thomas and Chess. Alexander Thomas, Stella Chess, Herbert G. Birch, Margaret Hertzig and Sam Korn began the classic New York Longitudinal study in the early 1950s regarding infant temperament (Thomas, Chess & Birch, 1968). •Activity •Regularity •Initial reaction •Adaptability •Intensity •Mood •Distractibility •Persistence •Attention span •Sensitivity Aetiology of PD Coid 1999 BJPsych • Population study to establish aetiological association between Axis II disorders and certain risk factors • Family Hx mental disorder (1st degree relative) • Neurobiological risk • Early environmental adversity Demographics and IQ Population sample survey indicated BPD associated with females and narcissistic, antisocial, histrionic were associated with males. Those with ASPD were of a lower socioeconomic class. Those with paranoid, antisocial, borderline and dependent were found to have slightly lowered full-scale IQ’s whilst narcissistic PD was associated with a higher IQ. Family History and early environmental adversity • Population survey found BPD associated with a family history of depression and parental dischord, other studies have disagreed Gunderson and Philips 1991. • ASPD associated with family history of PD and a range of factors including sexual abuse, poverty, cruelty and criminality in families • Schizoid PD was characterised by absence of early adversity Biological and neuropsychiatric risk factors • • • Schizoid PD associated with perinatal complications, motor and speech delay. It is associated with schizotypal PD. Suggested may fit better in neurodevelopmental classification Schizotypal PD is common in relatives of people with schizophrenia (Baron et al 1985) and is not included in ICD10 personality disorders Narcissistic and antisocial PD not associated with neuropsychiatric risk factors. There is correlation between the two (Coid 2003) and also psychopathy. Aetiological factors are varied. Biological susceptibility interacts with environmental adversity to varying degrees. BPD: the adult outcome of interactions between constitution and environment Genetic theory: Human serotonin transporter gene Some evidence found polymorphisms in the 5HT transporter gene to be associated with psychopathological phenotypes related to disturbed impulse control, anxiety, depression and violent behaviour Psychotherapeutic theories of PD Melanie Klein: The Paranoid-Schizoid position (1946) Part of normal development age 4-6 months. It can be normal to move in and out of this and more mature positions, however some operate in this much of the time. It is the more primitive position; a person will progress through it if environment and upbringing is satisfactory. Object Relations theory; Klein sees emotions as always related to other people or objects of emotions. Relations during these first months are not to whole objects but only to part objects (e.g. breast). Good Breast / Bad breast Paranoia: fear of invasive malevolence experienced as external. Derived from sense of destruction or death instinct. Paranoid-schizoid is before internalisation of a good object and the immature ego deals with paranoid anxiety by splitting off bad feelings and projecting them out. Schizoid: Defence of splitting. Separation of good from bad; means good can be identified with and introjected. This can protect good from being destroyed by bad. Depressive: Later when the ego has developed bad can be integrated and ambivalence and conflict tolerated. Leads to mourning of the idealised object. Formulation: splitting The Borderline Solution Sit on the fence Oscillation One foot in each camp Substance Misuse Opiates and Amphetamine ESCAPE ESCAPE ENTER • Fear of falling forever Case discussion if wanted? Video examples Narcissistic PD Borderline PD Antisocial PD Management: Biological, Psychological, Social? Caution- NICE guidance: • Pharmacotherapy should not be used routinely to specifically treat borderline PD or for individual symptoms or behaviour associated with it e.g repeated DSH, emotional lability, risk taking and transient psychotic symptoms • Pharmacological intervention should not be routinely used for treatment of ASPD or associated behaviour, aggression or impulsivity. NICE recommend integrated approach to BPD • • • • • • Person centred care: autonomy and choice Care planning (including endings) Psychological treatment (including close supervision) Specialist personality disorder services Risk assessment and crises management Managing self harm (separate guideline) ASPD • • • • Emphasis on treating comorbid disorders keeping in mind tendency to poor concordance, prescription and illicit drug and alcohol misuse and offending behaviour Group therapies based on cognitive and behavioural models: Aim at impulsivity, interpersonal problems, antisocial behaviour Reasoning and rehabilitation: focussed on reducing offending and other antisocial behaviour. Close supervision of those working with people with psychopathy CASC scenarios Summary and recap of learning objectives? Any other questions? Anything else needed to be covered?