Motivating Patients to Make Change
Ann Landes, Ph.D.
alandes@zoho.com
Disclosure of Financial Relationships
This speaker has no significant financial relationships with
commercial entities to disclose.
This slide set has been peer-reviewed to ensure that there are
no conflicts of interest represented in the presentation.
Objectives
1.
Introduce the model of Motivational Interviewing (MI)
2.
Provide an overview of the concept of "Stages of
Change" and its application to patient self-management
3.
Explain how MI can be employed by medical providers to
encourage collaboration between the patient and the
medical provider, as they work toward positive behavior
change and improved quality-of-life
SUPPORT FOR
MOTIVATIONAL INTERVIEWING
Hettema, Steele, and Miller (2005)
• Found significant support for the efficacy of MI
across 75 randomized controlled trials (RCTs).
• Adding MI to the beginning of treatment led to
sustained outcome improvements.
• Outcomes were better when no manual was used.
*(e.g., focus more on the alliance/relationship between
provider and patient)
Applications
•
•
•
•
•
•
•
•
•
•
Alcohol abuse
HIV risk reduction
Illicit drug use
Smoking
Treatment adherence
Diet/exercise
Gambling
Intimate relationships
Eating disorders
Water purification to promote health
Beach, Keruly, & Moore, 2005;
Schneider, et al., 2004
Patient-Centered Communication from Provider
Effective Patient-Physician Relationship & Communications
=
Greater patient satisfaction in medical care
Greater improvements in general medical condition
Increased adherence to medical treatments
WHAT IS MI?
Motivational Interviewing is a…
• method that has been found to be successful
in increasing intrinsic motivation to change by
exploring and resolving ambivalence
• collaborative effort between the provider and
patient
(Miller & Rollnick, 2002)
Motivational Interviewing …
• helps patients identify and address roadblocks
to change (i.e., fears, lack of skills/information,
needed supports, etc.)
• focuses on the way we as providers can
inspire positive change in the lives of patients
(Miller & Rollnick, 2002)
The Spirit of MI
Autonomy
Collaboration
Focusing on patient choice
Coming along side;
nonjudgmental
Asking “permission” to
provide assistance , info.
Evocation
Exploring what motivates the
patient
Making no assumptions
Viewing the patient as the
“expert”
Appreciation
of
Ambivalence
Notes about Ambivalence
• When an individual feels two ways about
something
• Normal to the process of change
Trap
If we argue for change, the patient may argue
for the status quo, leading to decreased
likelihood for change.
Motivational Interviewing is a
method that …
1. works to create
collaboration between the
provider and the patient
2. focuses on patient
choice/autonomy
3. sees ambivalence as
pathological
4. Answers “1” and “2”
5. None of the above
The Individual and Change
Patients with HIV/AIDs and Change
• Adherence to current medication schedule
• Maintaining regular medical appointments
• Making healthy choices about use of alcohol, tobacco, illicit drugs
• Attending to self-care needs, such as diet and exercise
• Practice consistent precautionary behaviors to reduce
transmission (prevention)
• Enlisting social support(s)
Prochaska and DiClemente’s
Stages of Change Model
Precontemplation
Contemplation
Preparation
Action
Maintenance
Relapse
Pre-contemplation
• “I see no problem(s) to address at this time.”
• “I know there’s a need for change, but I don’t want to
right now.”
(… has not given much thought to change)
Provider Role
Bring awareness to the issue
Encourage engagement of the patient
Tell-Tale Signs – “I’m not ready”
Argues/disagrees with the provider’s
diagnosis or suggestions
Resists offers of assistance
Expresses denial of problems/concerns
Communicates a sense of hopelessness
about the situation
Contemplation
• “Yeah, I’ve thought about my health needs, but I’m
just not ready yet to change.” (ambivalence)
Provider Role
Increase awareness about the
options for and benefits of change
* Keep the patient thinking about positive change.
Preparation/Determination
• “OK, I’m prepared to make some changes, but, I’m
not really sure I can or know how to do it.”
Provider Role
Decrease barriers to change by
providing resources, information & offering assistance
Address issues of self-efficacy
Action/Will Power
• “I know I need to make some changes; I have had to
make changes before and did it.”
Provider Role
Encourage movement by
helping to develop realistic goals and a plan-of-action
Offer resources and support
Maintenance
• “Wow! I have made some impressive changes! How
can I continue on this path?”
Provider Role
Help maintain positive focus
and
reduce opportunities for relapse
Relapse
• “I was doing really well, I thought, but then I got tired of
having to focus so much energy on caring for my health.
So, I just quit.”
Provider Role
Normalize that relapse is “OK” (reduce shame)
Encourage honest discussion about what led to relapse
Assist in re-exploration of personal goals
Help develop strategies for re-engagement
Tips To Remember
It is not about us.
Responsibility lies with the individual patient and
what they feel they need in their life.
Our role is to be active, caring observers who are
present to help the patient.
Because individual behaviors can change over
time, we need to remain vigilant about checking-in at
each encounter (Metsch, et al., 2004).
The Health Care Provider
&
Motivational Interviewing
INSTRUMENTS
OF CHANGE
Provider Stance
Guiding or coaching (versus directing) and
supporting
Respecting individual autonomy & empowerment
Expressing belief in the patient’s ability to make
decisions
Resisting the reflex to make it “right” or to label
actions as “good versus bad”
Four Processes of MI
1. Engaging: listening to understand – “OARS”
2. Focusing: agenda setting, finding a common and
strategic focus, exploring ambivalence, offering
information and advice
3. Evoking: selective eliciting, responding,
summaries toward change talk
4. Planning: moving toward commitment and change
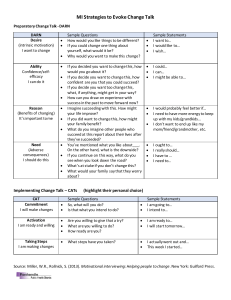
Change Speak – DARN-C
Desire:
I want to get healthier.
Ability:
I can do this if I set my mind to it.
Reasons:
Need:
My heavy drinking is causing me many health problems.
My family worries about me too much; it is not fair to them.
Commitment:
I will start getting more regular health check-ups.
Engaging: Building a therapeutic alliance
Step 1
OARS
Open ended questions
Affirmations
Reflective Listening
Summaries
http://motivationalinterview.org/clinical/interaction.html
www.mpaetc.org/downloads/motiv_interv_09.pdf
O-A-R-S
Open ended questions to elicit change talk:
• “What are some of your reasons for decreasing your
alcohol intake?” (desire)
• “How might you go about decreasing your drug usage?”
(ability)
• “What do you see as some benefits to lowering your
alcohol usage?” (reasons)
O-A-R-S
Open ended questions to elicit change talk:
• “How important is it for you to decrease your usage?”
(need)
• “What might you do to start reducing your alcohol
consumption?” (commitment)
O-A-R-S
Affirmations:
• Use to encourage people to see their “resources”
• Make them personal and genuine
• Explore partial successes and attempts and intentions
• Highlight patient attributes, effort
“I’m really glad you decided to come in to see me today.”
O-A-R-S
Reflective Listening (paraphrasing pt comments):
“It sounds as if you are a bit concerned about how to make
healthier choices in your life.”
Summaries (restating patient’s main points):
“Let me make sure I heard you correctly. You do want to
address your drug usage and you want information about
how to take more precautions in your sex life.”
O.A.R.S. is an acronym for the skills that can be
used to engage patients in treatment; it stands for
1. O-offer assistance; A-ask
questions; R-refer out;
S-summarize
2. O-operationalize; A-attend;
R-request tests; S-start goals
3. O-open ended questions;
A-affirmations; R-reflective
listening; S-summaries
4. O-open up discussion;
A-attend to; R-reflect;
S-shorten session
Focusing: Target one area
step 2
• Identify a strategic focus (agenda setting)
• Explore patient’s motivation, while listening
for change talk
• Offer and share information - ask
permission, Elicit-Provide-Elicit
Example
• Target behavior: use of condoms
• Agenda setting: “Hello, Sandy, it’s nice to see you. The
last time we met, we spoke about your goal to begin using
condoms more regularly. I’d like to start with that topic,
unless you have something more pressing to discuss.”
• Sandy: “I didn’t do too well - I do want to do better.”
• Possible Reflections:
• “You found it more difficult than you thought.”
• “You’re still committed to change and you found it
challenging.”
Example (cont.)
• Sandy: “My partner doesn’t like using condoms. He won’t
even talk to me about it.”
• Reflections:
• “It’s been difficult to make the change, especially since
your partner doesn’t agree with the change.”
• Sandy: “Yeah, I guess; I don’t really see the need either,
since I am monogamous.”
• Reflections:
• “You have questions about the importance of using
condoms, since you are having sex with just your
partner.
(cont.)
• Sandy: “Yeah, it’s such a big change; I’m not sure it’s worth it.”
• Reflection:
• “You feel a bit unprepared for making this change and
uncertain about whether using condoms is what you want to
do.”
• Sandy: “Yeah. I do and I don’t’ want to make the change.”
• Reflection:
• “You have some motivation to change. We can work on this
together. I have some ideas and information. Can I share
them with you?”
• Sandy: “Okay.”
Conversation continues
• Transitional Summary: “Alright, if I can summarize
what we have spoken about: You are confused about
the reasons for using a condom, it’s been difficult to
make the change since your partner does not agree
with it, and you feel unprepared. So, you would like
more information and some ideas that may work for
you.”
• Key Question: “Where do you want to begin – with
information about condom use, ways to make the
change, or how to approach your partner?”
(autonomy)
“Elicit, Provide, Elicit”
(information sharing process)
• ELICIT readiness and interest
• “What do you know about the effects of …”
• “What concerns do you have about…?”
• PROVIDE clear information or feedback
• “What happens to some people is that…”
• “The results of your tests suggest that…”
• “As your doctor/counselor/nurse, I strongly urge you to…”
• ELICIT the interpretation or reaction
• “What do you think?”
• “How do you think you might…?”
Evoking – pulling for change talk
step 3
• Encouraging, nurturing, reinforcing change
talk
• Guiding towards change – finding
alignment (and discrepancy) between
current behavior and goals and values
• Rolling with resistance
• Summarizing where you are
Approaches for Evoking Change Talk
Ruler for importance
Querying extremes
Goals and Values
Typical day
Looking forward
Coming alongside
Importance Ruler
“On a scale of 0 to 10, how important is it to you to
_________?”
“What is the reason it’s (x) and not (a lower number)?”
(If number is less than 8), “What would it take to move it
up in importance just one number?”
{Listen, reflect}
…“What do you think you might do next?”
Querying Extremes
“What are the worst things that could happen if
you don’t make this change?”
“What’s the best thing that could happen if
you make this change?”
Goals and Values
“Let’s, for a moment, move away from this ____ issue
and focus on the things that are most important to
you, your life dreams, goals, and values. Tell me the
most important areas for you.”
Listen, then say: “So being here, healthy, is important.
How does your (behavior) fit in with that?”
• Relate to values, bigger issues. May be useful to
prompt or have visual aides that reflect common
values and goals (family, work, country, spirituality,
community)
(Miller and C’deBaca, 2001)
Rolling with Resistance
o
Affirm and accept patient’s fears, concerns:
“I can understand your worries about the side effects of all you
medications. Let’s spend some time discussing this.”
o
Reflect other’s concerns:
“I hear you saying that you don’t care about maintaining a healthy
diet; but, how does this impact your partner?”
o
Reframing patient concerns to positive movement
“So what you’re saying is that you desire to quit smoking and
(instead of BUT) you realize this may be hard to do.”
o
Offer assistance
“How can I help you move towards making positive change? What
is needed?”
Assessment and Planning
step 4
• Summarizing where the patient is with regard to
making change
• Developing a goal and action plan
• Exploring, building patient’s confidence/self-efficacy
(affirmations)
• Addressing real and perceived barriers, challenges
• Scheduling follow-up
Assess Stage of Change
“How confident/ready are you in making changes to your
lifestyle?”
“How do you feel about the requirements of maintaining your
health?”
“ What do you hope with regard to your health diagnosis for
the future?”
“What concerns do you have about your risk-reduction
practices?”
Pre-contemplation
Listen and help address any patient concerns
“It sounds as if you want to reduce your alcohol intake, but your partner
does not want to change his/her lifestyle. Maybe we can brainstorm
ways that you can address this with your partner.”
Encourage information sharing from patient
“What is your opinion or belief about using condoms?”
“Tell me how you have been able to manage your medication
requirements.”
Express interest and empathy
“The decisions you have to make are very difficult. I know you can make
the decision on your own, but I would like to assist you in learning
more about your options.”
Planning for Change
(Contemplation Stage)
Attend to ambivalence
“I hear that part of you wants to make some positive changes, but a
part of you is also hesitant.” – reflect intention
Foster Self-efficacy and Autonomy
•
Elicit current knowledge: “What do you know about __?”
•
Provide information: “If I may, let me provide some information.”
•
Elicit Pt reaction: “What are your reactions to this information?”
•
“Ultimately, it is your decision to make about ___.”
Movement Towards Change
(Preparation and Action)
“What do you think would be a ‘do-able’ first step towards your
goal that you can do today?”
“What do you plan to do between now and next week?”
“ When do you think you will be able to start?”
“What strategies have you employed in the past to achieve
goals?”
“What will we be looking for that indicates success?”
Addressing Barriers to Change &
Enlisting Support
“What can I do to assist you?”
“Can I provide you some resources?”
“Who can you ask to be a support for you
during this time?”
Maintaining Positive Change
Normalize any possible set-backs (reduce shame)
“It’s OK if you don’t always meet your goals of ___”.
Help patient develop a plan to ensure success
“What other things can you do to encourage your progress
towards ____.”
“What might be some barriers or temptations that hinder you?”
Provide Continued Support
“I would you like to meet again to check-in and see how you are
doing. How does that sound?”
When Relapse Happens
Normalize relapse
“Relapsing is a normal part of any change process.”
Assist patient in remaining engaged
“I believe you are quite capable of continuing on toward your
goals – you did it before and you can do it again!”
“What lessons can be learned from this relapse to help you
remain focused on ___. What might you do differently?”
“Where do you think we should go from here?”
Case Study
H.A., a 42-year-old, Caucasian, divorced male is
referred to your care after he was found to be
HIV-seropositive. H.A. is currently unemployed
and homeless and though he has a long history
of abusing drugs and alcohol he states that he is
trying to “get clean”. H.A. states that he is really
concerned about his deteriorating physical and
mental health. When asked about social
supports, HA replies that he has a brother and a
sister who live close by. He adds that he also
receives great support from his case manager, a
social worker at the community-based recovery
program for homeless persons with addictions.
What is the patient’s stage of change and
how would you nurture his change talk?
1.
2.
3.
4.
Precontemplation Stage;
provider would express
empathy and encourage info.
sharing
Contemplation Stage;
provider would attend to
patient’s ambivalence and
foster his self-efficacy and
autonomy
Preparation Stage; provider
would help patient set goals
and develop action plan
Maintenance Stage; provider
would normalize relapse
Remind yourself that even if the patient
does not choose to change, the
intervention is not a failure.
Any discussion or talk about change is
planting a seed.
References
Beach, M., Keruly, J., & Moore, R. D. (2005). Is the quality of the
patient-provider relationship associated with better adherence and
health outcomes for patients with HIV? Journal of General Internal
Medicine, 21, 661.
Metsch, L. R, Pereyra, M., del Rio, C., Gardner, L., Duffus, W. A.,
Dickinson, G., et al. (2004). Delivery of HIV prevention counseling
by physicians at HIV medical care settings in 4 US cities.
American Journal of Public Health, 94(7), 1186.
Miller, W.R. & Rollnick, S. (2002). Motivational Interviewing: Preparing
People for Change (2nd ed.). New York: Guilford.
References
Miller, W. R., & C’deBaca, J. (2001). Quantum Change: When
Epiphanies and Sudden Insights Transform Ordinary Lives. New
York: Guilford Press.
Schneider, J., Kaplan, S. H., Greenfield, S., Li, W., & Wilson, I. B.
(2004). Better physician-patient relationships are associated with
higher reported adherence to antiretroviral therapy in patients
with HIV infection. Journal of General Internal Medicine, 19, 1096.
References
Cook, P. F., Bradley-Springer, L., & Corwin, M. A. (2009, August).
Motivational interviewing and HIV: Reducing risk, inspiring
change. Retrieved July 2, 2010, from
www.mpaetc.org/downloads/motiv_interv_09.pdf
Motivational interviewing [resources for clinicians, researchers, and
trainers.](n.d.) Retrieved July 2, 2010, from
http://motivationalinterview.org/clinical/interaction.html
Family Health International. (2007). Nursing care of patients with
HIV/AIDS. Retrieved August 19, 2010, from
http://www.fhi.org/NR/rdonlyres/erwyyfde6xm6oxea3vg46q5fpg7lo
ttczgkru5ymvykflcipkasb3jkqkfomo3ybedwpeis5z6sxlp/NursesCar
ePatientsParticipantsGuideHV.pdf
Questions?
• Contac
• Office: 352-376-1611 (x-4745)
Disclosure of Financial Relationships
This speaker has no significant financial relationships with
commercial entities to disclose.
This slide set has been peer-reviewed to ensure that there are
no conflicts of interest represented in the presentation.