Everything to do with schiz - a2 Psychology Lesson updates 13-14
advertisement
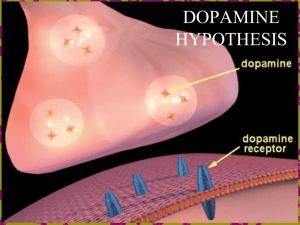
Schizophrenia Essential Revision In relation to their chosen disorder: schizophrenia Information to know characteristics of Sz WhatClinical do we need to know? Issues surrounding the classification and diagnosis of including relablitity and validity Biological explanations of Sz, for example, genetics, biochemistry Psychological explanations of Sz; behavioural, cognitive, psychodynamic and socio-cultural Biological therapies for their chosen disorder, including their evaluation in terms of appropriateness and effectiveness Psychological therapies for Sz, for example, behavioural, psychodynamic and cognitive-behavioural, including their evaluation in terms of appropriateness and effectiveness Schizophrenia Schizophrenia is one of the most chronic and disabling of the major mental illnesses affecting thought processes. 1% of the worldwide population suffers from schizophrenia. In order for a diagnosis to be made, two or more of the symptoms must be present for more than one month along with reduced social functioning The symptoms are separated into two categories; positive and negative. Positive symptoms are an excess or distortion of normal functions and negative symptoms are an diminution or loss of normal functions. The diagnostic criteria of the two systems (DSM and ICD) are very similar, but the DSM states that signs of disturbance should be apparent for at least 6 months, whereas the ICD requires the signs to be apparent for one month. Diagnosing mental disorders DSM (Diagnostic and statistical Manual of Mental Disorders) is produced by the American Psychiatric association. It contains a list of symptoms for each disorder and guidelines for clinicians who make diagnosis. ICD: International Classification of Diseases) is produced by the World Health Organisation for both physical and mental illnesses. Its aim is to follow the epidemiology of diseases worldwide. Clinical Characteristics Schizophrenia has been variously described as a disintegration of the personality A main feature is a split between thinking and emotion. It involves a range of psychotic symptoms (where there is a break from reality) Generally, schizophrenic patients lack insight into their condition, i.e. they do not realise that they are ill. They must follow the pattern of symptoms (see next slide) Positive and Negative Symptoms A distinction has been made between type 1 and type 2 schizophrenia. Type 1 is dominated by positive symptoms and type two by the negative. Positive Symptoms Negative symptoms Delusions – paranoia, grandiosity (i.e. Reduction in range and intensity of believe they are Jesus) emotional expression, including facial Experiences of control – thoughts and expression, tone of voice etc actions are believed to be under Avolition – reduction or inability to external control (i.e. of alien force). take part in goal directed behaviour. Auditory hallucinations – bizarre, Reactivity is not expected unreal perceptions, usually auditory. Thought blocking Thought disturbance and disordered Asocial behaviour thinking – thoughts have been inserted or withdrawn from the mind. Emotional blunting Psychomotor – catatonia – Language impairments immobility and frenetic activity Disorganised behaviour catatonia – immobility – echopraxia, echolalia Subtypes of Schizophrenia Paranoid Type – 35-40% (less severe) Preoccupation with one or more delusions or frequent auditory hallucinations. No disorganized speech, disorganized or catatonic behaviour, or flat or inappropriate affect. Catatonic Type – 10% immobility or stupor excessive motor activity that is apparently purposeless, extreme negativism, strange voluntary movement as evidenced by posturing, stereotyped movements, prominent mannerisms, or prominent grimacing. Disorganized Type – 10% Must have all; disorganized speech, disorganized behaviour, flat or inappropriate affect and not meet the criteria for Catatonic Type. Undifferentiated Type – 20% Variation between symptoms, not fitting into a particular type Residual Type – 20% Absence of prominent delusions, hallucinations, disorganized speech, and grossly disorganized or catatonic behaviour. Plus presence of negative symptoms or two or more symptoms listed in Criterion A for Schizophrenia Main points Reliability and validity of diagnosis Reliability • • • • • Both the DSM and the ICD are used and this causes difficulties as their criteria vary slightly. Despite the use of these system the reliability of diagnosis has been shown to be as low as 0.11 by Whalley. One symptom is “bizarre” delusion however what seems bizarre to 1 psychiatrist might not seem bizarre to another. Mojtabi and Nicholson found an inter-rater reliability of 0.4 which is low to base such a serious diagnosis Rosenhan’s study shows that reliability of diagnosis is questionable and is influenced by expectations and situational factors. Validity • Comorbidity Symptoms such as delusions and thought disorders are also found in other disorders such as bipolar disorders. • Predictive validity: it is impossible to predict the development of Sz in a particular individual therefore the Sz has low predictive validity. 20% of Sz recover their previous level of functioning, 10%show significant improvement, 30% show some improvement but 40% never recover. Because of the stigma attached to the diagnosis of Sz, psychiatrists might be reluctant to diagnose such a serious mental disorder therefore Sz might be underdiagnosed. Reliability; Reliability concerns consistency of measurements, in relation to the classification and diagnosis; inter-rater reliability – whether two or more clinicians make the same diagnosis when independently assessing a patient. Some of this error may be due to the fact that the same patient may give different information to different doctors. Test-retest reliability – whether the same clinician gives the same diagnosis when given the same information Obviously a diagnosis is useless if it fails to be consistent; BECK found 54% consistency when four experienced clinicians diagnosed 153 patients. More on Reliability There is both evidence for and against the reliability of a diagnosis of schizophrenia; PRO – the diagnosis of schizophrenia has relatively high reliability (+.81) ANTI – Read et al reported that test-retest reliability was as low as +.31 and also described a 1970 study where 194 British and 134 American psychiatrists were asked to provide a diagnosis on the basis of a case description. 69% American’s diagnosed schizophrenia and only 2% of British did. Despite low reliability, the classification schemes are still useful as they are better than nothing Classification systems are always being improved! (DSM II with Rosenhan, now DSM IV) Validity Reliability – an unreliable diagnosis cannot be valid (the diagnosis is not true; the person does not have schizophrenia). Predictive validity – if diagnosis results in successful treatment then the diagnosis must have been valid At one extreme, up to 20% of those diagnosed with schizophrenia never have a recurrence of the disorder after the first episode (Bichwood & Jackson, 2001). At the other extreme, about 10% of schizophrenics commit suicide (Birchwood & Jackson, 2001) Poor predictive validity! Cultural/Ethnic Bias – Keith et al. (1991) also found that 2.1% of African- Americans are diagnosed with schizophrenia, compared with 1.4% of white Americans. However, African-Americans on average are more likely than white Americans to live in poverty and to suffer marital separation. When these factors were controlled for, it turned out that there was no difference in the incidence of schizophrenia in the two groups. Social Class bias - . Keith et al. (1991) reported that 1.9% of lower-class people, 0.9% of middle-class people and only 0.4% of upper-class people were diagnosed with schizophrenia. Ethical issues around classification and Diagnosis Problems with type 1 and type 2 errors i.e. saying someone is schizophrenic when they are not, or saying someone does not have schizophrenia when they do. Labelling – diagnosis leads to labelling. While this can be helpful in terms of providing an appropriate treatment, it can be stigmatising and lead to a self-fulfilling prophecy. Genetics Neurochemical & hormones Structural brain abnormalities 1. 2. 3. Biological Explanation: Genetics Prevalence of schizophrenia is the same all over the world (about 1%) ◦ Supports a biological view as prevalence does not vary with environment Risk rises with degree of genetic relatedness ◦ Spouse – 1% (same as G.P.) ◦ Child – 13% ◦ DZ twin – 17% ◦ MZ twin – 48% Kendler et al (1985) found that 1st degree relatives of those with schizophrenia are 18 times more at risk than the general Population Children with both parents who suffer from schizophrenia have a CONCORDANCE RATE OF 46% Biological Explanation: Genetics The Copenhagen High-Risk Study (Kety et al. 1962) Kety identified 207 offspring of mothers diagnosed with schizophrenia (high risk) along with a matched control of 104 children with ‘healthy’ mothers (low risk) in 1962 Control group were matched on age, gender, parental socioeconomic status and urban/rural residence Children aged between 10-18 years at start of study Schizophrenia diagnosed in 16.2% of high risk group compared to 1.9% in low risk group Sherrington found that chromosome 5 has evidence of susceptible schizophrenia. Biological Explanation: Genetics To research more on the impact of genetics on schizophrenia, we can compare concordance rates for identical (MZ) and fraternal (DZ) twins Both share the same environment but only MZ twins have identical genetics – if schizophrenia is genetically related, the concordance rate of schizophrenia should be much higher in MZ twins. To prove this many studies have been conducted – ALL OF THEM show much higher concordance rate in MZ than DZ twins To prove the genetic influence further, you have to research the power of genetics in separate environments - researchers have sought out MZ twins reared apart where at least 1 has been diagnosed with schizophrenia Used the Maudsley twin register and found 58% (7/12 MZ twins reared apart) were concordant for schizophrenia Biological Explanation: Genetics Although twin, adoption and family studies continue to support that the degree of risk of developing schizophrenia increases with degree of genetic relatedness, there are two factors which stop us concluding biology as the source; No twin study has yet shown 100% concordance in MZ twins Studies conducted so far don’t tell us which genes might be important for the transmission of schizophrenia. Biochemical Explanation The dopamine hypothesis- Comer (2003) Dopamine is one of the many neurotransmitters operating in the brain. Dopamine neurons play a key role in guiding attention, so it is thought that disturbances in this process may lead to the problems of attention and thought found in people with schizophrenia. A group of drugs were developed in the 1950s called phenothiazines, which bind to the D2 receptors, effectively blocking the transmission of nerve impulses through these receptors and therefore reducing deficit found in schizophrenic. Evidence for Biochemical Explanation Dopamine substitutes such as L-Dopa increase the positive symptoms of schizophrenia L-Dopa is used to treat Parkinson’s Disease which is characterised by a lack of dopamine Too much L-Dopa produces psychotic symptoms in Parkinson’s patients Large doses of anti-schizophrenic drugs (in both ‘normal’ and schizophrenic patients) produce symptoms similar to Parkinson’s These drugs block the action of dopamine dopamine must be implicated in schizophrenia Evidence for Biochemical Explanation Drugs such as L-Dopa, cocaine, amphetamine, and methylphenidate (Ritalin) act as ‘dopamine agonists’ – mimicking the effects of dopamine because of their similar molecular shapes.. • Davis (1974) injected schizophrenics with methylphenidate and found a marked increase in symptoms • Griffith et al (1972) studied 7 participants with a history of amphetamine use: all were given large doses of dextroamphetamine every hour for 5 days although none had any previous history of mental illness, within 2-5 days all were showing psychotic symptoms General Evaluation of the Biochemical Approach There are ethical problems with this research. It might not just be about having too much dopamine. Schizophrenics are thought to have an abnormally high number of D2 receptors on their receiving neurons, resulting in more dopamine binding and therefore more neurons firing. Increases in dopamine leads to increases in positive symptoms, but not negative symptoms. Negative symptoms are better explained by structural brain abnormalities. Brain structure Using PET, MRI and Cat scans researchers have discovered that many schizophrenics have enlarged ventricles, cavities in the brain that supply nutrients and remove waste. The ventricles of a person with schizophrenia are on average about 15% bigger than normal (Torrey, 2002). Brown et al. (1986) found decreased brain weight and enlarged ventricles, which are the cavities in the brain that hold cerebrospinal fluid. Flaum et al. (1995) also found enlarged ventricles, along with smaller thalamic hippocampal and superior temporal volumes. Buchsbaum (1990) found abnormalities in the frontal and pre-frontal cortex, the basil ganglia, the hippocampus and the amygdale. As more MRI studies are being undertaken, more abnormalities are being identified. Structural abnormalities have been found more often in those with negative/chronic symptoms, rather than positive/acute symptoms, lending support to the belief that there are two types of schizophrenia: Type 1 (acute) and Type 2 (chronic). Evaluation research into enlarged ventricles and neurotransmitter levels have high reliability because the research is carried out in highly controlled environments, which specialist, high tech equipment such as MRI and PET scans. These machines take accurate readings of brain regions This suggests that if this research was tested and re-tested the same results would be achieved. Suddath et al. (1990)used MRI to obtain pictures of the brain structure of MZ twins in which one twin was schizophrenic. The schizophrenic twin generally had more enlarged ventricles and a reduced anterior hypothalamus. The differences were so large the schizophrenic twins could be easily identified from the brain images in 12 out of 15 pairs. This suggests that there is wider academic credibility for enlarged ventricles determining the likelihood of schizophrenia developing. The enlarged ventricles could be the effect rather than the cause of Sz. Beng-Choon Ho (2010) in a longitudinal correlational study of 211 schizophrenics found that antipsychotic drugs have measurable influence on brain tissue loss over time. This was supported by Lewis (2009) who administered antipsychotic drugs to primates and found a brain volume loss of 10% . However this was a correlational study so it does not show cause and effect and this study was carried out on animals so we cannot extrapolate to humans without caution. if the reduction in brain volume is the cause of the schizophrenic symptoms then it cannot explain why after 30 years of the initial onset, 35% of the schizophrenics are classified as "much improved". Evaluation of Biological Approach Humane approach; poses no blame on the individual or their families – states that the people who become ill are purely “unlucky” Tends to provoke little fear or stigma Effective treatments Well established scientific treatments Reductionist approach – Reference to Diathesis-Stress Model Animal studies Relies on self report Treats symptoms, not causes Behavioural Cognitive socio-cultural Psychological Explanations; Behavioural approach Behaviourists argue that learning plays a key role in the development of schizophrenia. One suggestion is that early experience of punishment may lead the child to retreat into a rewarding inner world. Others then label them as ‘odd’ or ‘strange’. Scheff’s (1966) labelling theory suggests that individuals labelled in this way may continue to act in ways that conform to this label. Bizarre behaviour is rewarded with attention, and becomes more and more exaggerated in a continuous cycle before being labelled as ‘schizophrenic’ Behaviourists have attempted to explain schizophrenia as the consequences of faulty learning. If a child receives little or no social reinforcement early on in life, the child will attend to inappropriate and irrelevant environmental cues, instead of focusing on social stimuli in the normal way. Behaviourists explain the fact that schizophrenia runs in families as a function of social learning. Bizarre behaviour by parents is copied by children. Parents then reinforce this behaviour and the behaviour becomes progressively more unusual, until eventually the child acquires the label of being ‘schizophrenic’. Evaluation The validity of the behavioural model is moderately supported by the success of behavioural therapies used with schizophrenic patients. Social skills training techniques have been used to help schizophrenics acquire useful social skills (Rodger et al.,2002). Allyon & Azrin (1968) have shown that schizophrenics have learned to make their own beds, comb their own hair etc. when given rewards for doing so. Finally Roder et al. (2002) has demonstrated that social skills training techniques have been used to help schizophrenics acquire social skills. The success of such programmes in teaching new skills and reintegrating schizophrenics back into the community suggests that these are skills that schizophrenics failed to learn in the first place. Overall this research can explain how schizophrenia symptoms are maintained but it does not adequately explain where they came from in the first place. Critics claim that labelling theory ignores strong genetic evidence and trivialises a serious disorder. In what ways could it be argued that the behaviourist approach to schizophrenia is reductionist? Further Evaluation of Behavioural Approach Experimentally tested Speaks on the present, as well as the past (validity) Effective treatments Accounts for cultural differences Simple model (reductionist) Animal studies Unethical? Need to refer to effectiveness and appropriateness (i.e. failure to take account of biological explanations is inappropriate, but success as developing social skills is effective). Psychological Explanation: Cognitive approach Frith (1992) attempted to explain the onset and maintenance of some of the positive symptoms of schizophrenia. This is called the faulty filter model. His idea is that people with schizophrenia are unable to distinguish between actions that are brought about by external forces and those that are generated internally. The filter between conscious and preconscious processing breaks down. Most symptoms of schizophrenia can be explained in three cognitive processes Inability to generate willed action (that is, any action that is under the voluntary control of the individual) Inability to monitor willed action Inability to monitor the beliefs and intentions of others These three processes are all part of a general mechanism (called meta-representation) that allows us to be aware of our goals and our intentions and to understand the beliefs and intentions of others. Faulty operation of this mechanism is due to functional disconnection between frontal areas of the brain concerned with action and more posterior areas of the brain that control perception. He has produced some evidence for his ideas by detecting changes in cerebral blood flow in the brains of people with schizophrenia when engaged in specific cognitive tasks Evaluation It has provided a comprehensive framework for explaining many of the symptoms in schizophrenia. Research support is far from conclusive and the theory is still regarded as speculative. reductionist, fails to take into account the role of environmental and biological factors. Second cognitive theory: Helmsley’s Model (1993) This is based on the failure of schemas to activate as they usually would in everyday situations. The result is that schizophrenics become overloaded with sensory information and do not know which things to pay attention to. This could explain delusions. He claims that hallucinations are internal thoughts that are not recognised as coming from memory so they appear to be external. Helmsley claims that these are caused by abnormalities in the hippocampus. Evaluation So far there is no clear evidence to support Helmsley’s model. Cognitive theories simply explain symptoms in terms of cognitive deficits they do not explain where the deficits come from so there is not yet a complete theory. The diathesis-stress model (Zubin +Spring 1977) argue that stressful life events could trigger psychotic symptoms providing there is a genetic predisposition. Provides key support for the nature-nurture debate because it represents an interaction. Evaluation of Cognitive Approach Focuses on the current cognitions Plenty of research into the idea Influential and popular model Includes biological and the psychological Empowers the individual to change Ignores the environmental influences Unscientific Blaming the individual can make the disorder worse Is thinking irrational? Which is the cause? Which is the effect? Psychological Explanation; Sociocultural factors Family relationships & Double Bind Theory Bateson et al. suggest that children who frequently receive contradictory messages from their parents are more likely to develop Sz because this prevents them from developing a consistent construction of reality. Tienary et al. found that adopted who had Sz biological parents were more likely to develop Sz than normal children, but only if the when the adopted family was rated as disturbed. Double bind theory has mixed support, Berger found that Sz reported a high recall of double-bind statements by their mothers than did non-Sz (although their recall might have been influenced by their Sz). Liem found no difference in patterns of parental communication in families of Sz and non-Sz Psychological Explanation: Sociocultural factors Expressed Emotion This is a family style of communication that involves criticism and emotional over involvement. High levels of EE are likely to influence relapse rate. Labelling theory: if a person displays unusual behaviours associated with SZ they are considered deviant by society. Once this label is applied, it becomes self-fulfilling leading to further symptoms. Scheff evaluated 18 studies and found that 13 of those were consistent with self-fulfilling prophecy. Psychological Explanation; Sociocultural factors Life events – Links with Diathesis-Stress Model A major stress factor that has been associated with a higher risk of schizophrenic episodes is the occurrence of stressful life events, such as the death of a relative, job loss or the break up of an intimate relationship. It is not known how stress triggers schizophrenia, although high levels of physiological arousal associated with neurotransmitter changes are thought to be involved. Brown and Birley (1968) found that approximately 50% of people experienced a major life event in the 3 weeks prior to a schizophrenic episode, whereas only 12% reported one in the 9 weeks prior to that. Hirsch et al (1996) followed 71 schizophrenic patients over a 48 week period. Life events made a significant cumulative contribution in the 12 months preceding relapse rather than having a more concentrated effect in the period just prior to the schizophrenic episode. Although not all evidence supports the role of life events, in one study it was found that there was no link between life events and the onset of schizophrenia, patients being equally likely to have a major life event or not in the 3 months before the schizophrenic episode. Pharmacotherapy - Antipsychotic Drugs Electroconvulsive Therapy (ECT) Biological Treatment; ECT – electro compulsive therapy ECT is not considered a first line treatment but may be prescribed in cases where other treatments have failed. It is not recommended as a treatment for schizophrenia ECT works by using an electrical shock to cause a seizure (a short period of irregular brain activity). This seizure releases a ‘rush’ of chemical neurotransmitters and temporarily alters function (eg. perception/memory etc) ECT is given up to 3 or 4 times a week and usually for a maximum of 12 treatments. Before each treatment, the patient is given an anesthetic (to induce sleep) and a muscle relaxant. Then an electrical shock is applied to the patient’s head (via electrodes). The shock will last only 1 or 2 seconds (high voltage / low amperage) and will make the brain have a seizure. Biological Treatment: ECT Side effects may result from both the anesthesia and the ECT. Common side effects include temporary short-term memory loss, confusion, paranoia, nausea, muscle aches and headache. Some people may have longer-lasting/permanent problems with memory/paranoia. Can cause death. (Shiwach et al, 2001: 1 death in 1,630 treatments) Evaluation of ECT ECT can have an immediate beneficial effect Significant benefit of ECT over placebo Huge research shows no damage to brain after ECT Risk of cognitive impairment Unscientific Risk of becoming used for social control Biological Treatment; Antipsychotic Drugs Drugs used to treat schizophrenia are called ANTIPSYCHOTIC drugs, they work to suppress hallucinations and delusions Antipsychotic drugs are known as TYPICAL and ATYPICAL TYPICAL = well established ATYPICAL = newer and less widely used ATYPICAL ANTIPSYCHOTIC DRUGS tend to have fewer side effects and act in different ways to typical antipsychotic drugs A patient is only ever on ONE psychotic drug at a time (anti depressants can be taken at the same time) ONE DRUG DOES NOT TREAT EACH MENTAL ILLNESS – depends on the individual response to drug treatments and clinicians preference for some drugs Biological Treatment: Conventional Antipsychotic Drugs Reduce the effects of dopamine and therefore the symptoms of Sz. They bind to dopamine receptors without simulating them . They can eliminate hallucinations and delusions. Effectiveness: Most studies on the effectiveness of conventional antipsychotic drugs compare the relapse rates of those on medication with those on a placebo. Davis et al. reviewed 29 studies and found that the relapse occurred in 55% of the patients who were on placebo compared to 19% on those who remained on drugs. However Ross and Read argued that this is not a fair test as people whose drugs are replaced by placebo are in a withdrawal state . Biological Treatment: Atypical Antipsychotic Drugs Atypical antipsychotic drugs act on the dopamine pathway but they only occupy the dopamine receptors temporarily. Therefore they have lower side effects than the conventional antipsychotic drugs. Effectiveness: A meta-analysis (Leuch et al) found that the superiority of the atypical antipsychotic drugs in the treatment of negative symptoms is only moderate. Biological Treatment; Antipsychotic Drugs The atypical antipsychotics (also known as second generation antipsychotics) are a group of unrelated* antipsychotic drugs used to treat psychiatric conditions. Atypicals such as Clozapine work differently from typicals in that they only attach to the specific D2 dopamine receptors (with a transient blocking action on excessive perceptionisation). Atypicals are preferred to conventional antipsychotics because they produce less side affects (eg. tardive diskinesia*) Good for ‘positive’ symptoms, however comparative affects on ‘negative’ schizophrenia are marginal (Leucht et al, 1999). Evaluation of drug treatment Strengths Highly effective Proven to prevent the reoccurrence of the mental disorder Most people are tolerant to the side effects Weaknesses Are not effective in treating every patient Nasty side effects – muscle stiffness, slowing, shakiness, change in appetite, diabetes, cardiovascular Drugs do not CURE the disorder Delayed effects? Patient is a passive recipient as is not involved in the treatment other than taking the tablets so might reduce the motivation of the patients to look for other causes (life stressors) and tackle these possible causes Cognitive Behavioural Therapy (CBT) Psychological treatments, such as cognitive behavioural therapy (CBT), can help people with schizophrenia to cope better with the symptoms of hallucinations or delusions. Psychological treatments can also help to treat some of the negative symptoms of schizophrenia, such as apathy or a lack of volition/hedonism (motivation / enjoyment in life). Psychological Treatment; CBT Cognitive behavioural therapy (CBT) is based on the idea that most unwanted thinking patterns, and emotional and behavioural reactions are learnt over a long period of time. The CBT approach to treatment differs slightly from conventional CBT methods. The aims of this therapy are as follows: To challenge and modify delusory beliefs To help the patient to identify delusions To challenge those delusions by looking at evidence To help the patient to begin to test the reality of the evidence For example, you may be taught to recognize examples of delusional thinking in yourself. You may then receive help and advice about how you can avoid acting on these thoughts. Most people will require between eight to 20 sessions of CBT over the space of six to 12 months. CBT sessions usually last for about an hour. This type of treatment has been shown to be effective for reducing the positive symptoms of schizophrenia, for reducing relapse and for enhancing recovery when schizophrenia is diagnosed early. Psychological Treatment; CBT CBT strategies to challenge & help modify delusory beliefs Identify delusions Challenge evidence on which delusions are based Design ‘experiments’ to test reality of this evidence Chadwick & Lowe (1993) – significant reductions in delusions in 10 out of 12 patients Normalising strategies where patient is taught to understand the nature of schiz. symptoms Challenge ‘catastrophising’ beliefs about schizophrenia Help patient feel that symptoms are understandable and ‘normal’ Helps 70% of patients although other 30% may deteriorate (Kingdon & Turkington, 1996) Evaluation of CBT Gould et al. carried out a meta-analysis of seven studies and found a significant decrease in the positive symptoms of Sz. Kuipers et al. found that when combined with antipsychotic drugs there was a lower drop out rate and greater patient satisfaction. Doesn’t work for everybody i.e. not suitable when the patient are deluding as they cannot fully engage with the therapy CBT for Sz works by generating less distressing explanations for negative experiences rather than eliminate them completely. Psychological Treatment; Behavioural Implosion- Extinguishing anxiety by inducing the client to imagine intensely anxiety-provoking scenes that, because they produce no harmful consequences, lose their power to induce fear. Flooding- Extinguishing anxiety by exposing the clients to actual fear-producing situations that, because they produce no harmful consequences, lose their power to induce fear. Modeling- Exposing clients to desired behaviour that is modeled by an other person, and rewarding the client for imitating that behaviour. Evaluation of behavioural Approach Effective treatments Cognitive sense Patient responsible Unethical? Impractical methodology? Restricted application Other therapies Milieu therapy Token economy Potential Exam Questions Describe two psychological explanations of the Schizophrenia (8 marks) Evaluate these explanations of Schizophrenia (16 marks) “Psychologists believe that Schizophrenia can be explained solely by biological factors” Discuss this claim with reference to the above quotation. (8+16 marks) Describe and evaluate at least two issues in classifying or diagnosing schizophrenia (24 marks) a) Explain issues relating to classifying schizophrenia as a mental disorder (5) b) Discuss two explanations of schizophrenia from different perspectives in psychology (8 and 11 marks) Describe and evaluate two psychological treatments of Schizophrenia (24 marks) Describe the clinical characteristics of Schizophrenia (8 marks) Explain and evaluate issues relating to the diagnosis of Schizophrenia as a mental disorder (16 marks) Discuss the extent to which biological therapies can be used to treat Schizophrenia. (24 marks)