Mike Grady
advertisement
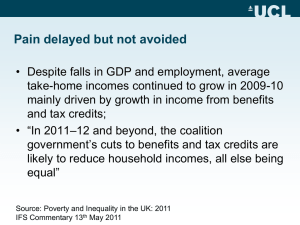
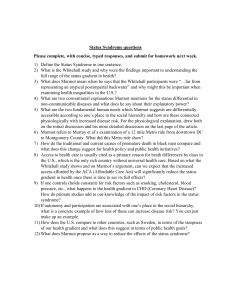
Dr Mike Grady Marmot Review Team. UCL. The Conceptual Framework Reduce health inequalities and improve health and well-being for all. Create an enabling society that maximises individual and community potential. Ensure social justice, health and sustainability are at heart of policies. Policy objectives Give every child the best start in life. Create fair employment and good work for all. Enable all children, young people and adults to maximise their capabilities and have control over their lives. Create and develop healthy and sustainable places and communities. Ensure healthy standard of living for all. Policy mechanisms Equality and health equity in all policies. Effective evidence-based delivery systems. Strengthen the role and impact of ill health prevention. Key themes Reducing health inequalities is a matter of fairness and social justice Action is needed to tackle the social gradient in health – Proportionate universalism Action on health inequalities requires action across all the social determinants of health Reducing health inequalities is vital for the economy – cost of inaction Beyond economic growth to well-being Cost of Inaction in lean times • In England, dying prematurely each year as a result of health inequalities between 1.3 and 2.5 million extra years of life lost – the human cost200000 deaths of 30+. • Economic benefits in reducing losses from illness associated with health inequalities. Each year in England these account for: – productivity losses of £31-33B – reduced tax revenue and higher welfare payments of £20-32B – increased treatment costs well in excess of £5B. Making it happen – A framework for delivery • Increased disability free life expectancy and reduction in inequalities across the gradient. • Empowering people : securing community solutions. • Intergovernmental action with dedicated leadership and executive team. • National Policies need effective local deliver focussed on health equity in all policies. • New model of civic and public sector leadership grounded in democracy and whole system thinking • Local Strategic Partnerships of Councils, NHS, 3rd Sector and Private Sector creating the conditions where individuals and communities take control. • Comprehensive, systematic, scaled up,coproduced action focussed on the social determinants of health. Partnerships with individuals and communities • Critical success factor in addressing health inequalities through empowerment – creating the conditions in which people can take control – Bespoke individual responses – Population focused approaches • Asset based partnership – half full not half empty – – – – Sharing power Community led and long term Shift in values and attitudes Leadership and knowledge transfer. • Shared aspirations in improving health and wellbeing – Perceptions of local schools, health and social care service, housing type,employment,safety and social cohesion. • Balancing long-term gains and short-term pressures. Evaluating partnerships • Process issues – Engagement of Senior managers in partnership – Reorganisation impact – Lack of financial and human resources – Information sharing and best practice – Coterminosity – Need for quick wins • Outcomes – Health outcomes – Monitoring and evaluation problems Perkins et al (2009) What counts is what works? New Labour and partnership in public health. Policy Press Public Health Workforce A Theory of Maturing Partnerships for Health Improvement Process factors No shared vision Confidence in partners Dominant partner Shared identity Top down Project focussed Quick wins Funding constraints Grant giving Immature Partnership Gaining collaborative advantage for health improvement Maturing partnership Little added value Shared vision Mature Partnership Showing Added value Increasingly acting on social determinants of health Joint ownership Alignment Joint posts Citizen engagement Internal focus Accountability Individual ownership Holistic Health an NHS issue Health everyones business. Medical Model External contextual factors Adapted from Seymour M (2009) Do LSPs provide collaborative advantage for Health Improvement. Addressing SDH Action • Olympic Host 5 Boroughs Strategic Regeneration Plan. Recommendations made to be incorporated into Stage 2 Plan to secure the Olympic legacy and convergence on health inequalities. • Bolton Local Strategic Partnership LSP developing action plan based on Marmot recommendations. To be submitted to marmot Team for comment. • Wakefield Council and PCT Working up a strategy for ratification by the LSP based on Marmot principles. • Yorkshire and the Humber NHS Action Plan to be agreed at next Board Meeting. Consideration being given to a 1 year dedicated post to oversee implementation of Marmot recommendations. • Coventry City Council and PCT Thematic Groups of the LSP to work up action plans on specific recommendations from the Marmot review. • North West Region Continuing development of regional strategy based on Marmot principles. • Greater London Authority. Marmot Team to facilitate and support implementation April 2010 • Health Lives/ Healthy Places 30 PCT sign up Social determinants approach to obesity Social Determinants approach Proximal Factors Areas of action Diet Early Years Skill Development Employment & work Communities & places Standard of living Prevention Equality/health equity Exercise Metabolism ‘Living Well’ Statements of intent to build vision of future For further information www.ucl.ac.uk/marmotreview