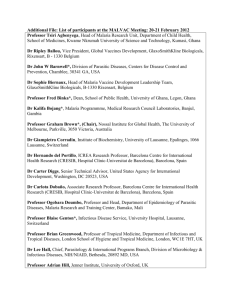
Research The Malaria..

Research: Malaria Vaccine and
Development
Baraka Amuri
Ifakara Health Institute (IHI)
Presentation Outline
•
Research and Development
•
Clinical phases
•
Target sites for malaria vaccines
•
Challenges
Research & Development
Identify
Antigen s
Produce
Antigens
Test in
Animal
Proof of
Concept
Phase I II III File Registration
/Post marktng
Preclinical Development (Inc. Formulation
Science)
Clinical Development (Inc Post
Marketing Surveillance up to 10-
20M$
2-4 yrs
Transfer Process to
Manufacturing x x up to 50-100M$ up to 500-1B$
1-10 yrs x x
Build
Facility x
2-3yrs
1 yr
Vaccine/Drug Development Model
Stage of Development:
A. Discovery and Pre-clinical Stages
Stage 1a
Discovery per se
Stage 1b
Transitional research
Stage 1c
Non-regulated
Non-clinical research
B. Clinical Phases/stages i. Phase I ii. Phase II iii. Phase II iv. Phase IV
Stage 1a: Discovery per se
• Researcher/scientist identifies a possible new vaccine/drug candidate
• Identifying signs that a compound may have a therapeutic potential
• Idea come from:
• Direct observation
• Scientific literature
• Knowledge of traditional practices
• Systematic screening
• Unlikely the research progress smoothly; researcher meet many dead ends and may collect inconclusive results
Stage 1b: Transitional research
• Researcher tries to characterize the active pharmaceutical ingredient (API)
• Investigate on how to produce and analyze the API
• Biological experimentation to investigate its actions in cells, tissues or the whole body
Stage 1c:
Non-regulated, non-clinical research
• Biological tests on subcellular systems, tissues and/or animals provide evidence for efficacy – i.e. ‘proof of principle’ (POP)
• Rigorously controlled studies with biological models
• Indicates whether the compound is biologically active
• Whether it is likely to be efficacious in man
• A sufficient supply of well-characterized test compound has to be ensured
Example
Stage 1a
Discovery per se
Stage 1b
Transitional research
Stage 1c
Non-regulated
Non-clinical research
A researcher knows that a population traditionally uses a local herb to alleviate an affective disorder.
But the herb contains dozens of interesting compounds of which several might be the active principle
Isolation of the most promising API, further exploration of the biological activity in cell, tissues and/or animal model.
Methods of producing and analyzing the compound
Receptor binding studies and animal behavioral models are most useful for establishing potential for efficacy
Clinical trial of Malaria vaccine
Animal models
PHASE 0
Preclinical
Safety, immunogenicity, tolerability, efficacy
Non-immune human volunteers in non-malarious areas.
Clinical setting
Human volunteers.
Experimental challenge with infected mosquitos.
Clinical setting
Semi-immune residents of malarious areas (all endemicities). Small target population, special groups.
Natural challenge
Semi-immune residents of malarious areas.Large target population, whole communities
Natural Challenge
PHASE 1
Clinical
PHASE II
Clinical
PHASE III
PHASE IV
Safety, immunogenicity, tolerability
Phase IIa: non-immune volunteers
Phase IIb: Immune volunteers
Vaccine efficacy, safety, tolerability, acceptance
Vaccine efficacy, safety, tolerability, acceptance
Vaccine efficacy, safety, tolerability, acceptance, vaccination strategy, effectiveness
Developing any vaccine is hard
Laboratory
Pre-clinical
Phase 1a
Phase 2
Phase 3
Can take 10-20 years to develop a product.
Cost hundreds of millions of dollars
Phase 1b
Malaria: Plasmodium Life Cycle
Gametocyte s
Sporozoites
Liver Stage
Blood Stage
Merozoites
Malaria: Plasmodium Life Cycle
Pre-erythrocytic stage, that is the stage that takes place shortly after being bitten by an infected mosquito up to and
including the liver stage.
Pre-erythrocytic
Stage
Sporozoites
Liver Stage
Pre-erythrocytic Stage Vaccines
• How they work:
• Generates Ab response against sporozoites and prevents them from invading the liver
• Prevents intra-hepatic multiplication by killing parasite-infected hepatocytes
• Intended Use:
• Ideal for travelers - protects against malaria infection
Malaria: Plasmodium Life Cycle
Asexual
Erythrocytic
Stage
Blood Stage
Merozoites
Asexual Erythrocytic Stage Vaccines
• How they work:
• Elicit antibodies that will inactivate merozoites and/or target malarial Ag expressed on RBC surface
• Inhibit development of parasite in RBCs
• Intended Use:
• Morbidity reduction in endemic countries
Malaria: Plasmodium Life Cycle
Sexual
Stage
Gametocytes
Sexual Stage Vaccines
• How they work:
• Induces Ab against sexual stage Ag
• Prevents development of infectious sporozoites in salivary glands of mosquitoes
• Prevent or decrease transmission of parasite to new hosts
• Intended Use:
• Decreased malaria transmission
Development
Manufacture
Ad5 CSP/
LSA/TRAP
Ad5 MSP-
AMA 1
MSP-4
MSP-5
Pfs-16
Vaccine Portfolio
Pre-Clinical
Evaluation
PvR II
in ASO2
PvR II
in AlOH
MSP-2 in ISCOM
MSP-2
in ISA 720
AMA-1C in ISA 720
AMA-1 in ASO2
AMA-1 in ASO1
Phase 1
+/- Challenge
LSA-1
in ASO1
CP2.9
in ISA 720
MSP-1C
in Alum-CPG
LSA-1
in ASO 2
Phase 1b endemic
RTS,S
in ASO1
Phase 2b endemic
RTS,S
in ASO2
Phase 3
RTS,S
in ASO2
RTS,S vaccine - Pre erythrocytic vaccine
• Hybrid containing the central repeats and most of the C-terminal of the CSP fused with hepatitis B surface antigen
• Complex adjuvant mixture AS02
• Completely protected six out of seven volunteers
• Field study in The Gambia showed good short-term protection
• A clinical trial in Mozambique and Tanzania showed delay of infection and reduction in incidence of severe malaria in young children
• The vaccine advanced to Phase III trial.
Efficacy in Double Blind Phase
Control
RTS,S/AS02
29.9%
95% CI
11-45 p = 0.004
0.7
0.6
Cohort 1
0.5
0.4
0.3
0.2
0.1
0.0
Clinical Malaria
4
3
2
1
7
6
5
0
Cohort 2
44.9%
95% CI
31-56 p < 0.001
Infection
ATP analyses
0.08
0.07
0.06
0.05
0.04
0.03
0.02
0.01
0.00
Exploratory cohort 1
57.7%
95% CI
15-79 p = 0.019
32.3%
95% CI 1-
54 p = 0.053
Severe malaria
Hospitalized malaria
Challenges for Malaria Vaccine
• Four antigenetically distinct malaria species
• Each has ~6,000 genes
• First gene only identified in 1983
• Immunity in malaria is complex and immunological responses and correlates of protection are incompletely understood.
• Identifying and assessing vaccine candidates takes time and is expensive
• There is no clear ‘best approach’ for designing a malaria vaccine