EAPS-poster4
advertisement

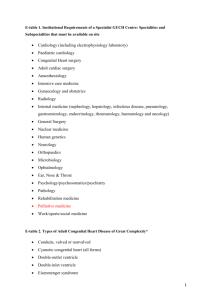
189 1st AND 2nd TRIMESTER HEAD SIZE IN FETUSES WITH CONGENITAL HEART DISEASE: A COHORT STUDY M.H. Lauridsen1, O.B. Petersen2, E.M. Vestergaard3, N. Uldbjerg2, T.B. Henriksen1, J.R. Østergaard1, N.B. Matthiesen1, V.E. Hjortdal4 1 Department of Paediatrics, Aarhus University Hospital, Denmark 2 Department of Obstetrics and Gynaecology, Aarhus University Hospital, Denmark 3 Department of Clinical Genetics, Aarhus University Hospital, Denmark 4 Department of Cardio-Thoracic Surgery, Aarhus University Hospital, Denmark Background: Congenital heart disease (CHD) is associated with neuro-developmental disorders. The influence of CHD on the brain may be present in the fetus. We hypothesize that fetal cerebral growth is impaired as early as 2nd trimester. Aim: To investigate if fetal cerebral growth is associated with major and minor CHD. Q-diagnoses CHD* Method: Pregnant women in Denmark (more than 95%) attend two publicly funded ultrasound scans; around 12 and 20 weeks gestational age (GA). During the first scan fetal bi-parietal-diameter (BPD) is routinely obtained. During the second scan fetal headcircumference (HC) is obtained and screening for fetal malformations is carried out. Our cohort includes all fetuses in Western Denmark (2.9 million inhabitants) screened in between January 1st 2012 and December 31st 2013, diagnosed with any structural, nonsyndromic congenital heart disease either during pregnancy or up to 6 months after birth. Results****: 276 fetuses with CHD were identified. 114 (41%) were genetically screened primarily by chromosomal microarray analysis (n=82). Fetuses with identified chromosomal abnormalities were excluded (flow chart) as were multiple gestation fetuses and fetuses with major extra cardiac malformations. Data from 208 fetuses (75%) with presumed non-syndromic CHD were included, 85 (41%) with minor and 123 (59%) with major CHD. Zscores for head size were analysed (table). Astraia-search CHD Invasive test results CHD Fetuses with CHD identified n=276** Chromosomal abnormalities n=29 (11%) (Common aneuploidies n=14) Multiple gestation n=26 (9%)*** Extra cardiac malformations n=15 (5%) Fetuses with presumed non-syndromic CHD n=208 (75%) Minor CHD n=85 Ventricular septal defect n= 46 Atrial septal defect n=30 Persistent arterial duct n=4 Double aortic arch n=3 Mild coarctation of the aorta n=2 Minor CHD Major CHD BPD Z-score GA week 12 0.10 (95% CI -0.1;0.3) 0.18 (95% CI -0.1;0,4) HC Z-score GA week 20 0.11 (95% CI -0.2;0.4) -0,37 (95% CI -0.6;-0.2) BPD Z-scores in week 12 and HC Z-scores in week 20 were analysed using students t-test (Stata 13). Major CHD n=123 Hypoplastic left heart syndrome n=23 Transposition of the great arteries n=16 Coarctation of the aorta n=14 Tetralogy of Fallot n=13 Pulmonary atresia or stenosis n=13 Atrioventricular septal defect n=8 Hypoplastic aortic arch n=8 Double outlet right ventricle n=7 Totally anomalous pulmonary venous drainage n=5 Hypoplastic right heart syndrome n=3 Other n=13 Conclusions: Our preliminary results suggest that Bi-parietal-diameter in children with CHD is within the normal range in the 1st trimester, but fetal cerebral growth may be disrupted as early as during 2nd trimester in major CHD. * CHD=structural congenital heart disease ** Right aortic arch, persistent arterial duct when born before gestational week 37 and dextrocardia or situs inversus are considered normal variations *** Two multiple gestation fetuses also fulfilled other exclusion criteria **** Data-collection and analysis are on-going Mette Høj Lauridsen, MD. Ph.D.-student. Departments of paediatrics and thoracic surgery research, Aarhus University Hospital. Denmark. Mail: mettelur@rm.dk