Cumbria and Lancashire End of
advertisement

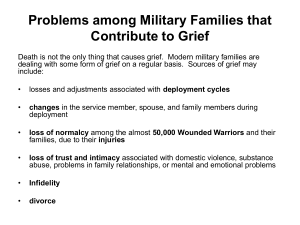
6 Steps to success in end of life care Residential homes Pam Williams Clinical Nurse Educator End of Life Care June 2011 Objectives • Identify good practice for the deceased resident • Give practical support and information to families, significant others, staff and other residents • Respect individual faiths & beliefs to address individual wishes • Have an action plan to implement a bereavement policy Listen to your wishes Help you think ahead Talk with you and the people who are important to you about your future needs. Endeavour to ensure clear written communication of your needs and wishes to those who offer you care and support Do our utmost to ensure that your remaining days and nights are as comfortable as possible Do all we can to help you preserve your independence, dignity and sense of personal control Support the people who are important to you, both as you approach the end of your life and during their bereavement. Royal College of Nursing patient charter 2011 Care of the deceased? • Last offices; • Death must be verified before last offices can commence • Is there a need for referral to the coroner? • Discuss any preferences with family i.e. religious or cultural requests • Collect all equipment necessary • Ensure privacy & dignity maintained Continued… • Remove anything invasive if appropriate • ( referral to coroner means all equipment must be left in situ) i.e. spigott off catheter & remove bag. • Remove jewellery unless instructed to leave on • Press gently on bladder if patient not catheterised to allow drainage and minimise leakage And… • Attend to hygiene needs particularly hair, nails & oral hygiene • If possible insert dentures , if not ensure they are clearly labelled and send with the body. • Attempt to close eyes using a small piece of clinical tape • Dress in shroud, gown or own clothes as required Documentation & legalities • • • • • • • • Check requirements for body bag Label patient as necessary Document everything & complete LCP Dispose of clinical waste appropriately Allow family time Arrange for transfer of the body Deal with property as per home policy Inform other agencies of the death as appropriate i.e. dn, gp, WHAT DO WE KNOW ABOUT GRIEF? • • • • • • • SOME EVIDENCE; The stages; Denial Anger Bargaining Depression Acceptance And… • High risk of increased morbidity and mortality Based on; • Experience of death • Supportive network NORMAL & ABNORMAL GRIEF Normal Grief • Found in the majority of survivors. • It describes grief that is eventually lessened as a person readjusts to their loss. • Grief is usually not something one “recovers” from because the loss is never regained or replaced. • A grieving individual doesn’t return to the person they were before the loss; rather they usually describe their lives after loss as “different”. • For some, it changes their entire identity and they will divide their lives into “before” the loss and “after” the loss. Abnormal Grief • Abnormal, often referred to as complicated grief, is found in only 3 to 25 percent of loss survivors. • Chronic grief – the grieving person has trouble finding closure and returning to normal activities over an extended amount of time. • Delayed grief – the intentional postponement of grief. • Disenfranchised grief – often occurs when a grieving person’s loss can’t be openly acknowledged or is one that society does not accept as a real. Examples include losses related to AIDS, miscarriage, or loss of a homosexual partner. • Exaggerated grief – intense reactions of grief • Sudden grief – when death takes place very suddenly without warning. Sudden grief can lead to posttraumatic stress disorder (PTSD). WHAT CAN WE DO? OFFER BEREAVEMENT SUPPORT AND INFORMATION TO THE FAMILY/SIGNIFICANT OTHERS What kind of information might they need? REMEMBRANCE • BOOK • GARDEN • REMEMBRANCE SERVICE • FOLLOW UP APPOINTMENT • ANY OTHER IDEAS? A BEREAVEMENT POLICY? • What the bereaved person is entitled to • The responsibilities of health professionals • How the home aims to meet these aspects The Role of the Funeral Director 6 STEPS END OF LIFE CARE POLICY • Systems are in place for providing good practice for the care and viewing of the deceased • Systems are in place to provide appropriate information and support to relatives and significant others, and staff post bereavement • Other residents are supported following a death in the care home • The quality of end of life care is sustained, audited and reviewed. SMALL CHANGE BIG DIFFERENCE • THOUGHTS FOR IMPLEMENTING CHANGE THE PORTFOLIO • Collecting evidence • Sorting evidence • CQC evidence • Ongoing resource THE CELEBRATION EVENT • WHAT DO YOU WANT TO HAPPEN? • DISPLAYING YOUR ACHIEVEMENTS ANY QUESTIONS