How Huddles Improved Hand Hygiene and Reduced VRE
advertisement
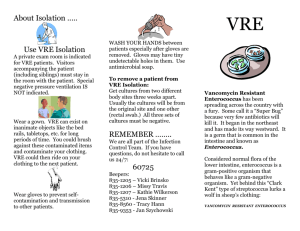
How Huddles Improved Hand Hygiene and Reduced VRE A reflection on our journey Overview • Identification of the problem: – Rising VRE rates • Use of high reliability concepts for change • End results Commercial Interest Disclosure: • Colleen Zidik • How Huddles Improved Hand Hygiene and Reduced VRE • The presenter today has no commercial interests to disclose. Objectives: • Importance of evaluating small tests of change • Importance of inter- and intra- professional involvement and team collaboration for sustainable results Unit's Nosocomial VRE Rates: Cases Per 1,000 Patient Days Curtains 15 13.8 Action Team 11.7 10 9 9 5 3 0 2.8 0 0 Sep-07 Oct-07 Nov-07 Dec-07 Jan-08 Feb-08 Mar-08 Apr-08 Unit's Hand Hygiene Compliance 100 Goal is 90%! 80 60 40 20 0 Dec-07 Jan-08 Feb-08 Mar-08 Apr-08 What Happened? • High Reliability Concepts (Roger Resar) – Process versus outcome – Standardization – Identification of defects – Daily Huddle (Mon - Fri) • What went wrong? • What went right? • What would you change? Action Team Brainstorming Ideas: What are the defects? • I can’t find the Purell • If I have to change gloves in the room, new ones aren’t available • I have to walk all around the unit to find a laundry basket • How is the BP cuff cleaned between patients? • I didn’t know the impact HCAI had on Patients • These yellow gowns do not provide enough protection Measures Implemented • Glove box holders in each room – Reduced # glove boxes stocked on cart, making Purell holders visible & accessible • Laundry Hampers in each room – Initial trial used trash cans designated for laundry • BP cuffs & Stethoscopes for each Patient Bed – Cleaned by UA after discharge • Infection Control In-services • New Precaution Gowns Yes No Why? Are Purell dispensers visible? Does each patient bed have BP cuff & Stethoscope in place? Are people removing protective equipment within the patient room? Are people using Purell at the door prior to entry & then after removing PPE? Are “laundry” trashcans overflowing with dirty laundry? Are 3 staff members able to identify when they need to wash hands? (Answer: At the doorway to the patient room before entering patient room, and after removing PPE ) Ask 3-5 staff members the following questions regarding the Pilot Project: What went wrong? What went right? What would you change? Huddles: May: Problem: MDs were not using Purell before entering room Solution: Reminder cards on outside of door to use Purell June: Problem: RNs were not using Purell upon exiting room Solution: Purell on the inside of the door in patient room July: Problem: Food trays brought from room to nurses’ desk Solution: Dirty tray holder on unit 6B Hand Hygiene Rates HCAI In-services began Identified need for Purell As you exit the room 100 80 60 40 20 0 Mar-08 Apr-08 May-08 Jun-08 Jul-08 6B VRE Rates per 1,000 Patient Days 10 HCAI In-Services began 9 Huddles occurred May-July 8 6 2.9 4 2 2.8 2.9 Jun-08 Jul-08 2.8 0 Mar-08 Apr-08 May-08 Was This Initiative Sustainable? Hand Hygiene • FY2008 84% • FY2009 88% • FYTD (Feb) 2010 94% VRE Rates/1,000 patient days • FY2008 4.7 • FY2009 2.2 • FYTD (as of Feb) 2010 1.9 Questions? • Impact on small tests of change? • Impact of inter- and intra- professional collaboration? Original Action Team Members • • • • • • • • • Rebecca Spitz, RN NIC Carolyn Clark, UC Stephanie Carroll, PA Rob Schlossman, MD Candy Hsieh, RN IC Susan O’Rourke, RN IC Rose Villarreal, PA IC Marsha Milone, RN ANM Jeanne Barton, Dir. Operations Management • Luis Soto, Asst. Dir. Environmental Services • Jeannie Keith, RN NM • Colleen Zidik, RN QPM • Tamara Devlin, Ops Sup • Andy Madden, Dir. Materials Management • Karen Purdy-Reilly, Food Services • Maggie Bikowski, IC • Miriam Perez, ESD Supervisor Objectives • Importance of evaluating small tests of change • Importance of inter- and intra- professional involvement and team collaboration for sustainable results