UK focus group issues presentation
advertisement

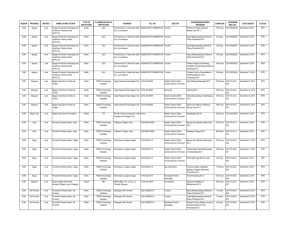
Focus Group: Hospitals and Residential Care DG EMPL – 12 July 2010 Study to support Impact Assessment regarding Directive 2003/88/EC and the evolution of working time organisation About the Study Aim: to provide evidence to enable the Commission to evaluate different options for action at Community level regarding Working Time, to inform decisions on what action should be taken, should any need for EU initiative be determined. CSES/ Deloitte’s work is being undertaken in parallel with DG EMPL’s public consultation exercise with the social partners. In order to measure the social and economic impacts of the WTD, the impact assessment will include four in-depth studies focusing on: Health and safety aspects of working time Economic impact on businesses Financial and organisational impact on public services Use of the 'opt-out'. 2 Study Objectives The specific aims of the study to support the Impact Assessment are to: Identify key social and economic changes in working patterns in the EU which affect the organisation of working time Analyse the main needs of workers, businesses, public services, consumers and other stakeholders in the EU regarding the organisation of working time Review the health and safety effects of various working time organisation patterns Analyse the economic costs and benefits to businesses in the EU arising from the Directive Data collection and analysis on the financial and organisational costs and benefits of the Directive for key public services in Member States 3 Impact of WTD on Hospitals A starting point for discussions - preliminary reading and discussions suggest that: Av. working hours in the NHS have fallen significantly in the past decade. From August 2004, junior doctors have been subject to EWTD with a 5 year phased transition period. A 48 hours max. av. weekly working limited has applied since August 2009. 44% of junior doctors were in Band 3 in March 2001, the earliest banding data available. 0.3% of junior doctors were in Band 3 in September 2009, the latest banding data available. Substantial investment by NHS in complying with WTD Temple report a "Time for Training" investigated how the quality and adequacy of training has been effected by a 48 hour week. While differences of opinion between stakeholders, report found that training could be accomplished within 48 hours Some concerns regarding amount of time available for training in particular medical disciplines (surgeons, anaesthetists, obstetricians?) Individual hospitals keep data on the working hours of junior doctors since this is linked to compensation and compliance with New Deal requirements. NHS Employers regularly collects compliance data on behalf of the Department of Health. However, there is no regional or national data on the extent of use of the opt-out by doctors (this is sometimes monitored by individual hospitals/ NHS trusts but no systematic data collection across all hospitals) 4 Impact of WTD on Hospitals (2) EWTD has had a considerable impact on resource planning. In some cases, complying with WTR has led to the reconfiguration and adaptation of service provision in hospitals To comply with WTR, there have been changes to working patterns and shifts. Given that doctors are working fewer hours than was previously the case, to what extent are they under increased pressure and work intensity? Finding adequate manpower to comply with EWTD while at the same time ensuring 24/7 service provision, covering staff shortages in particular specialties and covering sick leave etc. has been challenging for some hospitals While complying with WTR is not seen as that significant a problem by some NHS Trusts, it can pose challenges for others. Resourcing issues vary between regions, with particular problems identified in parts of Wales and Northern Ireland . There are also resourcing differences between urban and rural areas. Resourcing issues are also influenced by the changing composition of UK medical staff. While not linked to WTR, it is worth noting the wider context: changing gender composition of junior doctors, changes in immigration laws have made it more difficult for UK hospitals to recruit doctors from countries that have been important recruitment sources, including Australia, New Zealand, South Africa, the Indian sub-continent 5 Impact of WTD on Residential and Social Care Biggest issue – fact that many care workers may be on-call for considerable periods per week and also sleep-in at the social and residential care premises Sleep-ins have previously been seen as cost-effective by employers that run residential establishments such as care homes in covering 24-hour service operations using shift systems. Workers are commonly paid a nominal shift allowance rather than a higher, hourly rate. In light of the SIMAP-JAEGER ruling, however, time spent on an employer’s premises for a standard sleep-in shift counts as working time. Organisations providing essential 24-hour care are exempt from daily rest requirements, although they still have to provide workers with “compensatory rest”, which should be taken as soon as possible after a shift’s end. There are issues around whether sleep-ins result in residential and social care workers exceeding the 48 hr av. working. There are also pay and conditions issues - whether sleep-ins should be paid at the national minimum wage 6 Impact of WTD on Public Services – Key Questions What are the financial and resourcing implications of WTR? How has this changed since i) the original WTR were introduced ii) the adoption of the New Deal for Junior Doctors iii) Working Time Amendment Regulations? What are the main implications of WTR in respect of: medical training, patient satety and service delivery? What are the main regional variations in resourcing availability and how does this affect compliance with WTD? Likewise, what are differences between rural and urban areas? How far has WTD led to more flexible working practices? How do rest periods work in practice and how is compensatory rest managed? How does WTR affect different types of doctors within the NHS e.g. Junior doctors, doctors, consultants, senior consultants? What are the impacts of WTR and the opt-out respectively for safe patient care? How does this differ between hospitals and residential care? In the context of the financial constraints facing the UK health sector, what, if any changes are likely in terms of i) resource implications for hospitals in ensuring compliance with WTR requirements ii) the extent of usage of the opt-out? 7 Impact of WTD on Public Services – Key Questions How is on-call time managed? What are the implications of SIMAP-JAEGER in this regard? What are the potential problems faced by hospitals and residential care specifically with regard to the SIMAP-Jaeger rulings in terms of: • • • • Costs Practical organisation of work to provide 24 hour services Job quality Negative impacts on the health of employees What are the potential benefits arising from the SIMAP-Jaeger rulings • Avoiding negative implications for workers of long-hours (health and safety impact, risk of burn-out, negative implications for training, problems in reconciling work and family). • Avoiding negative affects of long-hours work for the employers and government (added difficulties in recruiting and retaining staff, higher risks of mistakes or accidents) • Advantages for the obligations of public authorities to ensure quality and continuity in provision of core services to citizens • Benefits for service users in terms of service quality, reducing risks of errors. 8 Impact of WTD on Public Services – Key Questions Potential benefits of strategies that have been implemented to cope with any issues arising from the Directive Experiences of reducing reliance on long-hours working by alternative work organisations Legal constraints to implement such strategies Time needed and acceptance/negotiation process with employees (organisation) Costs, effectiveness and efficiency of the strategies 9 Impact of the Opt–Out - Key Questions What are the benefits of the opt-out from WTD in respect of ensuring continuous resourcing of hospitals and residential care? How prevalent is the use of the individual opt-out in hospitals and residential/ social care? How effectively is monitoring carried out in respect of working hours by doctors/ care workers? What are the disadvantages of the opt-out? We would like help with factual information about the opt-out, specifically: Approximate proportion of workers that have signed an agreement to opt-out? Any limits to the weekly working time of a worker who agrees to opt-out Specifically for workers who agree to opt-out – proportion of on-call time in their total working time; level of activity required during on-call time Measures (and their effects) to ensure and protect health and safety of employees who agree to work more than 48 hours a week on average Extent of recording of working time patterns of individual employees (who have chosen to opt-out)? How practical would you find it to measure on call-time according to the level of activity required? Pay rates for workers who agree to opt-out and perform over-time? 10