Laalasa Varanasi - School of Medicine
advertisement
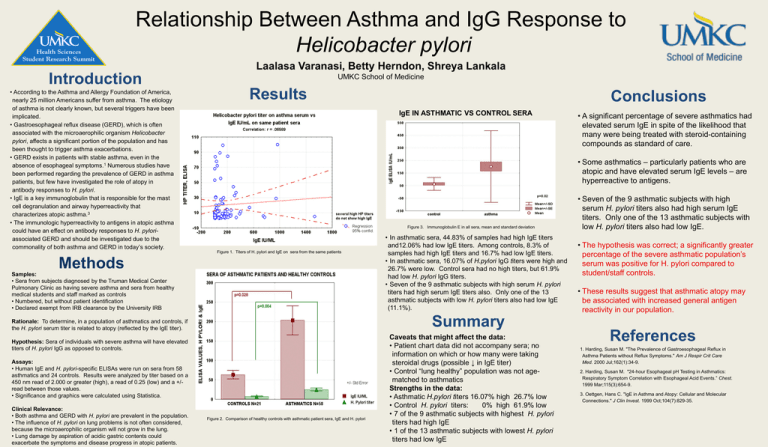
Relationship Between Asthma and IgG Response to Helicobacter pylori Laalasa Varanasi, Betty Herndon, Shreya Lankala Introduction • According to the Asthma and Allergy Foundation of America, nearly 25 million Americans suffer from asthma. The etiology of asthma is not clearly known, but several triggers have been implicated. • Gastroesophageal reflux disease (GERD), which is often associated with the microaerophilic organism Helicobacter pylori, affects a significant portion of the population and has been thought to trigger asthma exacerbations. • GERD exists in patients with stable asthma, even in the absence of esophageal symptoms.1 Numerous studies have been performed regarding the prevalence of GERD in asthma patients, but few have investigated the role of atopy in antibody responses to H. pylori. • IgE is a key immunoglobulin that is responsible for the mast cell degranulation and airway hyperreactivity that characterizes atopic asthma.3 • The immunologic hyperreactivity to antigens in atopic asthma could have an effect on antibody responses to H. pyloriassociated GERD and should be investigated due to the commonality of both asthma and GERD in today’s society. UMKC School of Medicine Results • A significant percentage of severe asthmatics had elevated serum IgE in spite of the likelihood that many were being treated with steroid-containing compounds as standard of care. • Some asthmatics – particularly patients who are atopic and have elevated serum IgE levels – are hyperreactive to antigens. Figure 3. Immunoglobulin E in all sera, mean and standard deviation Figure 1. Titers of H. pylori and IgE on sera from the same patients Methods Samples: • Sera from subjects diagnosed by the Truman Medical Center Pulmonary Clinic as having severe asthma and sera from healthy medical students and staff marked as controls • Numbered, but without patient identification • Declared exempt from IRB clearance by the University IRB • In asthmatic sera, 44.83% of samples had high IgE titers and12.06% had low IgE titers. Among controls, 8.3% of samples had high IgE titers and 16.7% had low IgE titers. • In asthmatic sera, 16.07% of H.pylori IgG titers were high and 26.7% were low. Control sera had no high titers, but 61.9% had low H. pylori IgG titers. • Seven of the 9 asthmatic subjects with high serum H. pylori titers had high serum IgE titers also. Only one of the 13 asthmatic subjects with low H. pylori titers also had low IgE (11.1%). Summary Rationale: To determine, in a population of asthmatics and controls, if the H. pylori serum titer is related to atopy (reflected by the IgE titer). Hypothesis: Sera of individuals with severe asthma will have elevated titers of H. pylori IgG as opposed to controls. Assays: • Human IgE and H. pylori-specific ELISAs were run on sera from 58 asthmatics and 24 controls. Results were analyzed by titer based on a 450 nm read of 2.000 or greater (high), a read of 0.25 (low) and a +/read between those values. • Significance and graphics were calculated using Statistica. Clinical Relevance: • Both asthma and GERD with H. pylori are prevalent in the population. • The influence of H. pylori on lung problems is not often considered, because the microaerophilic organism will not grow in the lung. • Lung damage by aspiration of acidic gastric contents could exacerbate the symptoms and disease progress in atopic patients. Conclusions Figure 2. Comparison of healthy controls with asthmatic patient sera, IgE and H. pylori Caveats that might affect the data: • Patient chart data did not accompany sera; no information on which or how many were taking steroidal drugs (possible ↓ in IgE titer) • Control “lung healthy” population was not agematched to asthmatics Strengths in the data: • Asthmatic H.pylori titers 16.07% high 26.7% low • Control H. pylori titers: 0% high 61.9% low • 7 of the 9 asthmatic subjects with highest H. pylori titers had high IgE • 1 of the 13 asthmatic subjects with lowest H. pylori titers had low IgE • Seven of the 9 asthmatic subjects with high serum H. pylori titers also had high serum IgE titers. Only one of the 13 asthmatic subjects with low H. pylori titers also had low IgE. • The hypothesis was correct; a significantly greater percentage of the severe asthmatic population’s serum was positive for H. pylori compared to student/staff controls. • These results suggest that asthmatic atopy may be associated with increased general antigen reactivity in our population. References 1. Harding, Susan M. "The Prevalence of Gastroesophageal Reflux in Asthma Patients without Reflux Symptoms." Am J Respir Crit Care Med. 2000 Jul;162(1):34-9. 2. Harding, Susan M. "24-hour Esophageal pH Testing in Asthmatics: Respiratory Symptom Correlation with Esophageal Acid Events.” Chest. 1999 Mar;115(3):654-9. 3. Oettgen, Hans C. "IgE in Asthma and Atopy: Cellular and Molecular Connections." J Clin Invest. 1999 Oct;104(7):829-35.