Resource - Indiana Rural Health Association
advertisement

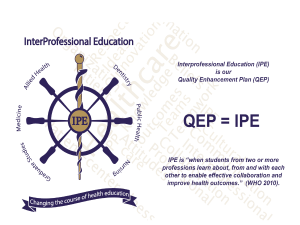
Interprofessional Education at a Federally Qualified Health Center Who Are We? Dr. Eric Beachy, MD Medical Director VPCHC Dr. Jim Buechler, MD Director Emeritus Richard G. Lugar Center for Rural Health Dana Edwardson Clinical Mental Health Counseling Graduate Student Indiana State University Learning in Silos Today’s Health Care Training What is Interprofessional Education “When students from two or more professions learn about, from and with each other to enable effective collaboration and improve health outcomes.” (WHO – 2010) The Goal of IPE “The Goal of this interprofessional learning is to prepare all health professions students for deliberately working together with the common goal of building a safer and better patient-centered and community/population oriented U.S. health care system.” Interprofessional Education Collaborative Expert Panel – 2011 Other Definitions Interprofessional Teamwork - “The levels of cooperation, coordination, collaboration characterizing the relationships between professions in delivering patient-centered care.” (IECEP – 2011) Interprofessional Team Based Care - “Care delivered by intentionally created, usually relatively small work groups in health care, who are recognized by others as well as by themselves as having a collective identity and shared responsibility for a patient or group of patients, e.g., rapid response team, palliative care team, primary care team, operating room team.” (IECEP – 2011) Interprofessional Collaborative Practice - “When multiple health workers from different professional backgrounds work together with patients, families, caregivers and communities to deliver the highest quality of care. (WHO – 2010) History of Interprofessional Education • First started to be looked at approximately 50 years ago • First scholarly articles regarding IPE appeared in the Journal of Medical Education in 1965 • Institute of Medicine Conference “Interrelationships of Educational Programs for Health Professionals” was held in 1972 Early Drivers of Interest in IPE IOM Committee Expressed the following reasons for IPE: – Desire to use existing health care workforce optimally and cost-effectively – Desire to ensure that health care workers are trained and enabled to practice to the full scope of their expertise – Recognition of need for effective multi-disciplinary teams and that the educational system at the time was not preparing health professionals for team work Interesting Early Articles “A Student-Run Course in Interprofessional Relations” – Journal of Medical Education March 1977 – A student-driven collaborative course for students in the disciplines of medicine, nursing, physical therapy and occupational therapy “The Mini-God Syndrome” Journal of Medical Education – February 1978 “Arrogance is a rather common failing among physicians…. outwardly, it is expressed in various behavioral patterns, such as belittlement of the patient or the nursing staff or in self-exaltation over colleagues.” “This phenomenon can be uprooted quite easily on condition that every one of us is conscious of it, is persistent in his self restraint, and remembers to treat every fellow human being with due honors.” Recent Explosion of Interest in IPE Average annual articles published by decade in Academic Medicine (formerly Journal of Medical Education) Annual average IPE articles 35 30 25 20 Annual average IPE articles 15 10 5 0 1965-1974 1975-1984 1985-1994 1995-2004 2005-2014 Why is IPE Important Today? The same issues as were present in the 1960s and 70s persist today We need to prepare tomorrow’s healthcare workers to collaborate effectively with all members of the healthcare team to improve patient care, outcomes, provider satisfaction (and thus retention), and cost-effective care delivery A Small, Experimental IPE Effort Initiated by the Lugar Center for Rural Health – participating organizations included the IUSOM, Indiana State University (Physician Assistant and Clinical Mental Health Counseling students), VPCHC The Project To provide clinical students from varying disciplines the opportunity to work in collaborative partnerships to more effectively treat patients of a rural Federally Qualified Health Center. Valley Professionals Community Health Center • Federally Qualified Health Center (FQHC) • Offers primary and behavioral health care services to citizens of Parke and Vermillion counties in west central Indiana • Serves residents below 200% of the Federal Poverty Level (FPL), uninsured, underinsured, Medicaid, Medicare, privately insured patients • VPCHC has three service delivery sites – Clinton, IN (Vermillion Co.) – Cayuga, IN (Vermillion Co.) – Bloomingdale (Parke Co.) Bloomingdale Clinic Valley Professionals Community Health Center • Opened in 2013 • See over 700 patients annually • Located in Parke County: – Health Professional Shortage Area (HPSA) – Partial-county Medically Underserved Area (MUA) – Population of 17,152 – 36.9% of residents living below 200% of the FPL Who was Involved? • Medical Preceptor • Behavioral Health Preceptor • Medicine IU School of Medicine • Clinical Mental Health Counseling Graduate Student Indiana State University • Physician Assistant Indiana State University *By chance, a practicing NP was also present for several sessions Perceived Possible Barriers (Prior to Start of Project) • Patient Receptiveness • Patient Volume – Too much or too little would not work well • How would students interact with each other • Preceptor Time How was it Structured? • 4 afternoons in fall 2013 – October 22, October 29, November 5, November 12 • Students, preceptors all present in exam room (if patient willing – most were) • Medical HPI initiated by Medical Preceptor with follow-up questions asked by learners • Behavioral Health history taken by counseling student and/or Behavioral Health preceptor • At the end of each afternoon, team sat down together and discussed patients, interactions, learning points Evaluation - Course Course Survey • Assessed whether course objectives were met: – Have an enhanced understanding of Federally Qualified Health Centers – Enhance skill sets such as history taking and physical examination – Become more comfortable communicating with students in other healthcare disciplines – Better understand the level of education, training, and skill sets required of other healthcare disciplines – Better understand the benefits of IPE and the collaboration of multiple disciplines toward the enhancement of patient care Evaluation - IPE Interdisciplinary Education Perception Scale (IEPS) Luecht et al, (1990, Journal of Allied Health, 181-191) • Valid, evidence-based tool • Measures attitudes deemed important in the interprofessional setting • Completed pre/post course Results - What was Learned? • Every student responded that each objective was met fully • Attitudes toward IPE improved • Knowledge of other health professions increased • Collaborative learning was enjoyable! • Multiple patients had Behavioral Health needs that would not have been uncovered without this collaborative exercise • Patients felt like the “center of attention” – most were very receptive Why Did it Work? • • • • Patient volume appropriate Preceptor buy-in Student receptiveness Patient engagement How Could it Be Improved? • Expanded scope of disciplines involved • Expanded number of sessions • Involving Students at various levels of training – e.g. including upper level medical and PA students, possibly residents Resources • Framework for Action on Interprofessional Education and Collaborative Practice - World Health Organization (2010) • Core Competencies for Interprofessional Collaborative Practice – Report of an Expert Panel (May 2011) - Sponsored by Interprofessional Education Collaborative - AACN, AACOM, AACP, ADEA, AAMC, ASPH THANK YOU!