SYMPHONY
Person-Centred Coordinated Care
Our Aim
“to dramatically improve the way in which
health and social care is delivered in South
Somerset”
The Symphony Project Board
We adopt the National Voices definition of person-centred coordinated care.
We will work to achieve person-centred coordinated care by:
• Supporting people to remain independent and healthy for as long as possible.
• When people do need advice or support, ensuring this is easy to obtain.
• Making it as easy as possible for people to access the services they need and
ensuring that we can provide individualised care to meet their needs.
• Ensuring that staff across our organisations work to do the right thing for the
people they care for at the right time, in the right place, regardless of who they
work for.
• Making it easier and more rewarding for staff to do their jobs.
We believe that if we do this, not only will local people receive better care but these
services will be more efficient and will make best use of our staff and our money.
Chard, Crewkerne and
Ilminster Federation
Other Partners (so far)
• Centre for Health Economics, York University
• South Somerset Together
• South Somerset Association for Voluntary and Community
Action
• Age UK Somerset
• South Somerset MIND
• Yarlington Housing Group
• Yeovil College
• Registered Care Providers Association
• South Somerset CAB
• Somerset Pharmaceutical Committee
• Devon & Somerset Fire & Rescue Service
Evidence-Based Approach
Establish the right environment to allow co-ordinated
care to flourish (culture, leadership, systems, processes,
incentives, information systems, governance)
Build on the approach of the Independent Living Teams
to develop integrated care model across primary,
community, acute, social care and wider
Key Symphony Components
1. Patient-focussed data set - evidence
2. Shared outcomes
3. A new way of contracting and a
shared budget
4. Care model
The Data-set
Overall Aims
• To identify which group(s) of patients should be the initial
focus of the Symphony Project (i.e. where there would be the
most benefit from an integrated approach)
• To inform the outline business case
• To develop a methodology to calculate a shared budget for
that group of patients
• To provide a baseline so the impact can be tracked
The Data-Set
• Fully pseudonymised
• South Somerset GP Federation (109,000 patients)
• Majority of activity and cost at patient level for:
–
–
–
–
–
–
Primary care
Community hospitals
Mental health (community and inpatient)
Acute
Social care
Continuing health care
• Age, sex, clinical conditions, ward of residence
• It’s evolving
What’s not included…yet
•
•
•
•
•
•
•
•
•
•
•
•
•
District nursing and health visiting
Ambulance service
Podiatry
Dietetics
Community diabetes service
Rehab
Community therapies
Tissue viability
Speech and language therapies
Continence
End of life
Voluntary sector
I’m sure there are others
Approach to Analysis
• Understand current patterns of utilisation and cost
• Understand what drives these patterns
• Develop an approach to decide which group to target
Approach to Analysis
• Develop method to calculate shared budget and
impact on each organisation
• Develop approach to tracking and evaluation
Basis
Frequency of
occurrence
Rationale
In developing a budget, need
enough people to form the “risk
pool”.
Analytical approach
Assess how many people
have particular conditions
(ETG) and combinations of
conditions.
People with multiple conditions
are more likely to require
collaborative care arrangements.
Costs of care
Potential savings greater the
higher are the costs of care.
Summarise total costs and
setting-specific costs by ETG.
Utilisation of
services across
settings
People who require services
Summarise the number and
across diverse settings most likely type of settings in which
to benefit from collaborative care patients receive care by ETG.
requirements
Morbidity (number of ETGs) by age band
100%
90%
80%
Number of
conditions
70%
0
Patients (%)
60%
1
2
50%
3
4
40%
5
6
30%
7+
20%
10%
0%
0-4
5-9
10-14
15-19
20-24
25-29
30-34
35-39
40-44
45-49
Age band (Years)
50-54
55-59
60-64
65-69
70-74
75-79
80-84
85+
Regression
variables
Age
Number of
conditions
Age, Number
of conditions
Variation
explained
3.36%
18.76%
19.30%
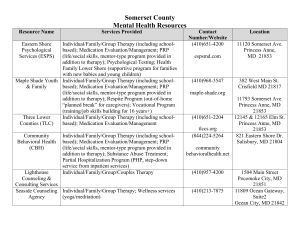
People with diabetes or dementia and any number of other
co-morbidities
Group
Number of
patients
Total cost
Diabetes
5625
£17M
% variation in
costs
predicted
36%
Dementia
1062
£13M
15%
Diabetes +
dementia
6521
£28M
38%
People with diabetes or dementia and any number of other
co-morbidities
Total cost by setting
Group
£
GP practice
1,163,285
Prescribing
2,778,463
Inpatient
7,456,346
Outpatient
1,543,905
AE
281,422
Mental health
2,288,199
Community health
1,504,421
Social care
6,651,990
Continuing care
4,401,048
Total
28,069,078
2. Outcomes
•
•
•
•
•
Central to care model and alliance contract
To be developed by patients, carers and staff
Facilitated process culminating in workshop
Care model designed to deliver them
Alliance contract tied to them
What does “good” look like?
• One-to-one interviews with patients
and carers
• Event for patients and staff
• What does “good” look like for:
–
–
–
–
Patients
Carers
Staff
“The system”
3. Alliance contract
4. Care model
• Design work starts in December
• Design team:
– Lead responsible for delivery: member of Project Board
– Design team oversees process and makes strategic design
decisions to recommend to project board
– Expert facilitation
– Project support
– To deliver the agreed outcomes
• Clinician and patient-led
• Learn from Independent Living Teams;
• Include known effective ingredients (e.g. care coordination, single assessment, shared protocols)
Timescale
Patient
group
decision
September
October
Patient &
carer
interviews
“What good
looks like”
agreed
Initial design process
November
December
January
March
2014 February
Alliance contract negotiation
Patient and staff involvement
April
Alliance
agreement