ON-FIELD PHYSIOTHERAPY
advertisement

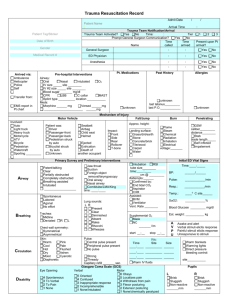
ON-FIELD PHYSIOTHERAPY CONTENTS Roles of on-field physiotherapist Basic assessment procedures Prevention and assessment of heat & cold injuries Management of acute soft tissue injuries Why we need on field physiotherapy? ON FIELD PHYSIOTHERAPIST Roles On-field services in Hong Kong Team Physiotherapist Domestic, National and International Level ON-FIELD PHYSIOTHERAPY SERVICES 1996 International Masters Hockey Tournament 1996 Seoul International Women’s Road relay Hong Kong Cricket team - Bangladesh Cricket Tournament Standard Chartered Shenzen - Hong Kong Marathon Swire Group Tsing Ma Bridge 10 km and Marathon Hong Kong - Beijing Relay Standard Chartered International Marathon (1997-2002) Sports Physiotherapy in Elite level SDB, 5 full time physiotherapists Hong Kong Team physiotherapists 1987 Asian Athletic Championship 1992 Barcelona Olympics, 1994 Commonwealth and Asian Games, 1996 Altanta Olympics (3) 2002 Busan Asian Games: 8 physiotherapists KNOW THE SPORT ON FIELD SERVICES KNOW THE VENUE PREPARATION Deployment Equipment of manpower Types of injury Cases Muscle soreness/strain 175 Ligamentous sprain 112 Tendonitis 44 Joint problems 41 Contusion 42 Laceration 7 Haematoma 3 Concussion 1 Others 6 Types of services Number IFT 44 US 158 TENS 34 HVG 7 ICE 98 Manual technique 210 Massage 211 Strapping and taping 70 Dressing 13 Education and advice 85 ON-FIELD MANAGEMENT ASSESSMENT VENUE PERSON PROCEDURES SYSTEMATIC APPROACH Scene Survey Is the scene safe? It is frequently better to remain uncertain about a diagnosis and feel mildly folish than to be constantly certain and confirm that you are an absolute fool. PRIMARY SURVEY OF THE PATIENT LOC Talk to the patient and assess his level of consciousness A Alert V Response to vocal stimuli P Response to pain U Unresponsive AIRWAY + C-SPINE CONTROL Is the victim able to maintain his airway If he can talk, the airway is OK Open airway by jaw thrust if necessary Do not use head tilt as this may affect the C-spine BREATHING Assess if victim is breathing adequately. Is it too fast? too slow? too shallow? Oxygen, if available, should be given if breathing is laboured. Feel for any tenderness BREATHING Auscultate the chest for unequal air entry Check if the trachea is central CIRCULATION Arrest any visible haemorrhage using direct pressure Check both carotid and radial pulse If radial pulse is weak or not palpable, the patient is probably in shock Capillary refill is less than 2 second normally CIRCULATION If the patient is unresponsive and with no carotid pulse==> this is cardiac arrest. you should start cardiopulmonary resuscitation immediately DECISION POINT : SEND FOR THE AMBULANCE IMMEDIATELY Impaired conscious state Airway obstruction Breathing difficulties Significant external bleeding especially when control by external pressure is ineffective DECISION POINT : SEND FOR THE AMBULANCE IMMEDIATELY feature of shock: thready pulse, cold clammy hands, delayed capillary refill unstable pelvis major fracture of limb bones CARDIOPULMONARY ARREST PROBABLE CAUSES: HEAD TRAUMA Cx INJURY MAXILOFACIAL OR THORACIC TRAUMA CVA MYOCARDIAL INFARCTION HAEMORRHAGE INTERNAL: COLD RAPID PULSE AND RESPIRATION PALPABLE PAIN AND TENDERNESS RESTLESSNESS EXCESSIVE THIRST BLOOD IN THE URINE OR STOOL OBSERVE FOR SHOCK OR ARREST HAEMORRHAGE External Direct Pressure Arterial Pressure Pt. Compression Area should be elevated SECONDARY ASSESSMENT Chief Complaints Behaviour of symptoms Location & radiation of the symptoms Mode of onset Mechanism of injury Functional alterations Related symptoms Past injuries LOOK AND PALPATION Location of Pain Degree & type of swelling Temperature & texture of the area Muscle spasm Tissue continuity & deformity Neuromuscular function Abnormal Motion or sensation MOVEMENT Active & Functional Motions Resistive Motion Specific Stress Test Sport Specific Function Return to activity HEAT INJURY Metabolic Heat Stress Metabolic heat production Exercise Shivering Thryoxine Sympathetic stimulation Exercise 20-25x 25% efficiency Heat Production Heat Balance Radiation Conduction Convection Evaporation Heat loss WBGT 0.1: 0.7: 0.2 CONVECTION Responsible for transferring heat from working muscles and the skin surface Temp differential between skin and environment Heat transfer coefficient, body surface area and wind velocity Minimal body fat and loose-fitting clothing CONDUCTION Minimal effect on body heat transfer Direct contact between skin and an object RADIATION Solar radiation and radiation from tracks, roads, and surrounding structures Can be a major contributor to heat load EVAPORATION Most important heat dissipation mechanism in warm environments Sweating – a fit athlete can produce up to 30 ml of sweat per min Evaporation depends evaporative heat transfer coefficient – air velocity and water vapor pressure gradient (relative humidity) WBGT Wet Bulb Globe Temperature Three monitors: Dry bulb (Tdb) air temperature Wet bulb (Twb) relative humidity Black globe (Tg) solar radiation WBGT = 0.1Tdb + 0.7Twb + 0.2Tg Without adaptive mechanisms, moderate exercise could elevate temp by 1C every 5-6’ Fluid/electrolyte Loss of solutions Sodium andadded Prevention: Potassium salt to food, high K+ diet HEAT INJURY Heat Cramp Warm, humid conditions, inadequate Cool fluids fluid pre-hydrate replacement Dehydration Red, Hot and Dry skin Heat exhaustion Strong & Rapid pulse LackMedical of sweating, CNS symptoms unsteady Emergency !! gait Heat Stroke confusion, combative behaviour, coma Profuse Sweating Clammy & Cool Shading Skin remove excess Headache &cloth cooling with ice, Weakness sponges Nausea & hydration Weakness monitor Rapid vital Pulsesign & hospital Disorientation PREVENTION Conditioning sweat rate Acclimatization 3-4 Thirst: hrs/day, poor indicator 60-70% load core temperature Intake: 400-600 ml 15-20’ 5-10 days volume Fluid replacement 2-3%; plasma 200-300 ml every 15-20’ exercise heat storage Venue and schedule intense 3L/hr Every L loss, 0.3 C Q 1L/min HR 8 CHILDREN AND HEAT INJURY Sweat less effectively; produce metabolic heat for given workload; acclimatize more slowly than adults; larger M/A; renal tubular filtration rate; self perceive; BUT HOW ABOUT COLD INJURY? Heat loss also depends on air movement, humidity, evaporation (sweating) and ambient temperature Wind velocity exacerbates heat losses Adequate clothing High energy bar Avoid wind exposure Medical Emergency !! Mild Hypothermina Moderate Hypothermia Severe Hypothermia Shivering, cold, hunger Confusion muscle spasm Slow pace Semi-conscious confused actions Extremely tired Poor coordination Muscle stiffness Slurred speech Disorientation Loss of consciousness Faint heartbeat Acute Sports Injuries Treatment that comes with PRICE! MANAGEMENT OF ACUTE SOFT TISSUE INJURIES PRICE HARM