Intro. to FallProof Balance Tests - California State University, Fullerton
advertisement

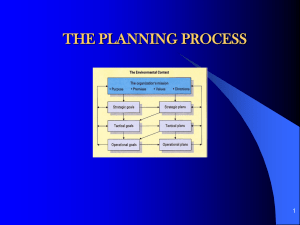
Introduction to TM FallProof Balance Tests Debbie Rose, Ph.D. Co-Director, Center for Successful Aging California State University, Fullerton FallProofTM Screening and Assessment Tools Fall Risk • 8 Foot Up and Go Functional Limitations • Fullerton Advanced Balance (FAB) Scale • Berg Balance Scale (BBS) • 50 Foot Walk at Preferred and Fast Speed • “Walkie-Talkie” Test FallProofTM Screening and Assessment Tools Sensory Impairments • Modified version of the Clinical Test of Sensory Interaction in Balance (M-CTSIB) Motor Impairments • Multidirectional Reach Test FallProofTM Screening and Assessment Tools Physical Impairments • Senior Fitness Test Items – Chair Stand; Arm Curl; Chair Sit-and-Reach; Scratch Test; 2Minute Step Fear-of-Falling • Health/Activity Questionnaire • Balance Efficacy Scale (Optional) Fullerton Advanced Balance Scale Developed by Rose & Lucchese (2003). Test demonstrates high test-retest reliability (.95) Inter-rater reliability is also high, ranging from .94 to .97 when administered by experienced clinicians. Scale is comprised of 10 items designed to measure multiple dimensions of balance. Recommended for use with higher functioning community-dwelling older adults only. Fullerton Advanced Balance Scale Test requires little equipment Can be administered within 8 to 10 minutes Has operational definitions by which to score each test item Assesses more dimensions of balance when compared to the Berg Balance Scale Expect to be less prone to ceiling effects Fullerton Advanced Balance Scale Test Items include: • Standing with feet together, eyes closed • Reaching forward to grasp object • Turn 360 degrees • Stepping over an obstacle • Walking with feet in tandem position • Standing on one foot Fullerton Advanced Balance Scale Test Items include: • Standing on foam, eyes closed. • Two-footed Jump for Distance • Walk with Head Turns • Backward Perturbation Total Score Possible: 40 Points Balance Dimensions Sensory reception and integration • Items 1; 3; 7; 9 Motor coordination • Items 2; 4; 5; 6; 8; 10 Musculoskeletal Integrity • Items 4; 5; 6; 7; 8 Interpretation of Item Scores Possible underlying Impairments? • Item 1- Standing with feet together and eyes closed. Weak hip abductor/adductor muscles Poor use of somatosensory Cues Poor Center of Gravity Control Interpretation of Item Scores Possible underlying Impairments? • Item 8 – Two-footed jump for distance. Lower body muscle weakness Poor Center of Gravity Control Poor upper and lower body coordination Interpretation of Item Scores Possible underlying Impairments? • Item 9- Walk with Head Turns Possible vestibular impairment? Poor use of vision Poor dynamic COG control Interpretation of Item Scores Possible underlying Impairments? • Item 10 – Unexpected Backward Release Absent or ineffective use of step strategy Lower body weakness (reduced power) Poor Center of Gravity Control Berg Balance Scale (BBS) Developed by Berg in 1989 Test comprised of 14 performance items High validity, test-retest and rater reliability Requires approximately 15 to 20 minutes to administer Prone to ceiling effects when used with community-dwelling older adults. Berg Balance Scale Test Items Include: • Rising from a chair • Standing independently for two minutes • Seated balance (if unable to stand independently) • Sitting down in a chair • Transfers between chairs • Standing with eyes closed Berg Balance Scale Test Items Include: • Standing with feet together • Leaning forward • Picking object up from floor • Turn to look over shoulders • 360 degree turn • Dynamic toe touching • Tandem Stance • Standing on one leg Modified Version of BBS In modified version of the test, the first 5 test items are deleted (Daschle et al., 1987) High reliability and validity retained with modified version. Total score reduced from 56 to 36 points Interpretation of Item Scores Possible impairments associated with low Scores: • Item 1 – lower and upper body weakness; poor dynamic COG control; Abnormal weight distribution. • Item 2 – Poor gaze stabilization; lower body weakness; abnormal weight distribution in standing. • Item 6 – Poor use of somatosensory inputs; Visual dependency and/or fear-of-falling; Lower body weakness.