Aphasia Notes - A Guide to Treatment of Aphasia
advertisement

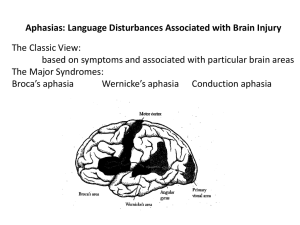
Aphasia Notes Test III Athena Hagerty • General Info about Treatment: • Working with Adults: you can tell them what they are doing and why. You can provide concrete feedback to your patient. Telling the person what they are doing a great job at. You can provide feedback for errors. “That wasn’t a good way to say that, tell me again”. Progress is its own reward. Instead of planning for kiddos, adults are happy for therapy, you don’t have to give them a sticker. • General Info about Treatment: • Planning for treatment- don’t take hours, do it easily and it’s cheap or free for therapy. Free newspapers from Dubois. Clinic has a laminator. Paper, pencil and you can do therapy Generalization: • Loose training- you should consider stimulus items that elicit a variety of acceptable responses. 1 cup for multiple things • Sequential modification- treat in different environments and diff. contexts. • Does Treatment Work? • Aphasia therapy work? YES. But It needs very good guidance from the clinician. Don’t do workbook stuff. If they don’t need you, they shouldn’t be in therapy. Computer programs are bad. Group therapy also WORKS. Evidence behind it. More support by other patients. Maintaining skills. Goals of Aphasia Therapy • Empowering the patient- you teach them skills that they can use. • Communicative Competence- the person can communicate in ANY context. If you can do this with patient you are a successful SLP. • Who receives treatment?- Initially everyone who has aphasia should receive treatment. • Prognosis- there are some people with really poor prognosis= severe Wernicke’s, severe global, after 3 months following injury. If nothing changes after 3 months that’s bad. • Group therapy- if its available, patient should participate. • Evaluation of cognition- you can evaluate cognition as the person improves IF the neruopsych is good at evaluation. – Neuropsych needs to be experienced. Treatment of Auditory Comp. • Bottom up model- patient is analyzing sounds to make sense of info. Repeating plate over and over again to make sense of it. • Top down model- begins with an expectation about the the speaker will say. Either confirm or change the action depending on the production. Ex- you’re walking and see a friend hows it going? They say not so good, you keep walking, see you later… then go back and ask them what up. Treatment of Auditory Comp. • Knowledge based/heuristic process– general knowledge and intuition to deduce meaning of spoken information. – what to expect when you are ordering at a restaurant. Treatment of Auditory Comp. • Point to/ show me • Y/N questions • Wh- questions/tell me (simple or complex) what is your name? where are you? Does it snow in July? Do you use an axe to cut the grass? • Following Directions (1-3) can increase up to three steps. (WM component) • Sentence verification- person has to listen to sentence and tell if its true or false. Can make it difficult my adding fake words. Treatment of Auditory Comp. • Task switching activities• Discourse comprehension – can they actually answer questions? – Familiar- if its familiar it will be easier. – Length & redundancy- Goal Writing • Long term goal- 3 components to a goal- every supervisor requires these 3 things. • Performance=measure • Condition- type of cues you are using • Criteria –percentage or trials Treatment of Auditory Comp. Aud comp long term goal- will vary from facility to facility. Determine goal by hierarchy. End point to whatever facility your in. where we want to get the patient eventually. • ST Goals- small steps to get to the long term goal. Baby step to get to long term goal. Point to show me/ y/n • Biggest LT goal- to comprehend conversation. Ask questions during conversation and keep track of answers. • Ex- patient. Moderate aud comp deficits. Are long term goal would be for academic year. ST- semester. Complex y/n questions. CUES • Cues- extra help • • • • • • • Verbal- explaining or repeating Phonemic- it’s a” K” for key. Visual Pointing Gestures Written Tactile (touch)- holding their hand. Giving them something to feel or touch. Percentages Maximum moderate minimum assistance. – Dr Isaki doesn’t like these terms. Doesn’t like 3 out of 4 trials. Likes percentages better. • Mild- 90% of time can do tasks. • Moderate-80% of time • Severe-70% of time • Try and shoot for 20% (increase) of time. • Global aphasia- 30% of time correct- yes you can get them to 50% of the time. • Normal is not 80% of the time. You can write a goal for 100% of time if you think you can do it. Because they were capable before the CVA. • If client hits goal 3 times, you then need to review to goals and revise them. Goal for Auditory Comp. • GOAL for this client- client will answer complex yes/no question with 95% accuracy given verbal cues. In my methods verbal cues means repetition of questions. • Client will follow 3 step commands with 95% accuracy given visual cues. Visual cues may be pointing to item Expressive language Treatment • Content Words (nouns more important for Global) • Enhance with nonverbal communication (can live w/out articles & adverbs) • Increase length & complexity- Sub, Verb, Obj • Picture Description- take a picture from the newspaper (Norman Rockwell pics) • Storytelling & retelling • Conversation- most difficult • If you improve anomia, you will improve expressive language Reading Comprehension Tx. (deficits) • Reading glasses? Do they have glasses? • Surface Dyslexia? Lost direct lexical route and now dependent on phonological route. Exsound by sound or letter by letter. • Deep dyslexia- you have lost phonological route, now you’re dependent on whole word recognition. Reading Comprehension Tx. (deficits) • • • • • Letters- can they identify a letter? Words to pics- matching words to pics Phrase to pics Sentence- written questions or matching to pics Paragraph- written questions, 2 sentences, then 3, short stories • Survival Reading (6th grade level) menu, telephone book Anomic Tx. • Anomia looks like… • • • • Pauses Fillers “uh, um” I don’t know Ineffective gestures (waving during conversation) Anomic Tx. Suggestions for therapy • Naming (Rosenbek,Lapointe & Wertz) Choose at least 3 strategies • Semantic description- start describing its attributes, formulate descriptors to pull out. Cat= furry meow. • Embedding- (good for anomic aphasia) formulate your own sentence, embed the word within the sentence. Cup=”You use a _____ for drinking.” • Synonyms- works for high functioning • Antonyms- not every word has an antonym Anomic Tx. Suggestions for therapy • Rhyming- “cat” “bat”- looking at things that rhyme to get word. • Sentence completion- high functioning= anomic, conduction. “You drink from a _____.” • Phonemic cues- weird strategy. Everyone around patient uses the prompt “You drink from a c____.” • Writing- if you can’t think of a word, can’t write it. • Gestures- depends on person’s vocab, for high functioning patient • Drawing- depends on person’s vocab, for high functioning patient Anomic Tx. Suggestions for therapy • Once you DO get word: • practice for a couple of trials (recommend 3). • Also practice at the end of session. Format (Brookshire) • Hello- (only 5 minutes) where you catch up with your patient. How was your week? Etc. • Accommodation- we are going to work on easier tasks first. • Work- where you concentrate on more difficult tasks. • Cool down- more easier tasks so they can feel good about their performance. • Goodbye- reviewing entire session and progress they were able to show. Summarize abilities Resource Allocation • Central Pool- a way to think about how your therapy is affecting your client, analyze performance. Can pull out all sorts of language abilities and cognitive processes. • Depends on the demands of the task, you can pull out too many processes from the central pool. If this happens, the client will fail. • Reduce processes if client fails. • Environment can affect performance (noisy, busy, etc.) SIMPLIFY environment • Dr Isaki said to change rooms if the room you’re in is too noisy. Resource Allocation NAMING AUDITORY COMP CENTRAL POOL ORGANIZATION PROBLEM SOLVING Goals of Aphasia Therapy • 1) want patient to regain as much comm as possible as much as their injury allows and their needs drive them. • 2) teach them to compensate for the skills that they lack. • 3) teach them to be in harmony with their lives. Preparing someone for lifetime of Aphasia • 1) remember to give fair assessments of prognosis (don’t use word normal) • 2) stress the importance of what remains. (everyone has skills) • 3) Aphasia is a human disorder meaning it not only affects language, but a person’s life and relationship to others. Patients are unchanged at the core. Preparing someone for lifetime of Aphasia • 4. Never forget you are treating a PERSON w/ Aphasia. Try to resist being everything to the patient. • 5. Learn to be a good listener. We’ll hear all types of info. We have boundaries in our profession, refer out as needed. • 6. Have to trust our patients that they are going to survive and cope and life Preparing someone for lifetime of Aphasia • 7. We are going to be counseling for comm disorders (not depression). Teach them about Aphasia and words we use. National Aphasia Assoc. has great paperwork. • LISTENING IS IMPORTANT. Silence is OK. Wait for them to say something. Shouldn’t be weird. Listen to their family and friends and ask what concerns they have. Preparing someone for lifetime of Aphasia • Rosenbeck states “that clinicians that are adequate, treat all people more or less equally. A superior clinicians finds out what each patient wants and needs and determines what is possible. ADULTS • • • • • • Easiest population. Easiest prep time No stickers & crafts Don’t need to applaud Comm is its own reward If you have superior clinician, will see amazing things in therapy. • Patient will try harder and they continue treatment. • Difficult for them to let you go. ADULTS cont. • You can point out errors and how to change those errors. • You have built this relationship on trust, support and respect. • It is acceptable to exploit a person’s strengths. • Prepare for generalization- client needs to be on their own. Take client out of therapy and let client do their own thing. Then go back in clinic and talk about it. A good clinician…. • Can adjust to changes- client will have good days and bad. We should be constantly thinking of hierarchy. • Recognizes when therapy isn’t doing very much • Laughter & crying is OK-sympathizing is OK. • Therapy has an ending. If patient plateaus, maybe it’s time to discharge them. You can say “ you can always come see me”. • Speech = motor- damage to PMC causes apraxia • Language= syntax semantics etc. Speech Deficits • Apraxia- the disturbed ability to reproduce purposeful learned movement, despite intact mobility. NO weakness of the musculature. • Ideational Apraxia- the disruption of ideas needed to understand the use of objects. Exwhen we see key, we know how to use it. – Show them object and say “show me how to use it”. Speech Deficits • Ideomotor Apraxia- requires motor movement. Types of ideomotor: – 1) Buccofacial/nonverbal/oral apraxia- the inability to demonstrate volitional oral movements on command. Exercises on oral mech exam. If you have this apraxia, you’ll see struggle and searching behaviors. Speech Deficitstype of ideomotor apraxia • 2) Limb Apraxia- inability to demonstrate volitional movements of arm wrist and hand on command. Exwave goodbye (they have problems with that). Look for whether they can do movements closer to the body or further away. Assess: if you give them an object they can do movement, take away object, they can’t. Kind of like they can’t pretend. Speech Deficitstype of ideomotor apraxia • 3) Apraxia of speech- where patient has problems programming the position and sequence of speech musculature, for the production of volitional speech (Darley Def.) • Characteristics: – No weakness or paralysis or sensory loss – Automatic speech is easier than planned speech – Artic consistancies in/of errors. When they make errors it WILL be consistent. – Struggle and searching behavior. Dysarthrias • Dysarthrias- weakness, paralysis, incoordination of the muscles, required for speech. • Descriptors: speech sounds slurred, unclear, imprecise. • Tx- make sure you have unfamiliar listeners come is to check client’s production because eventually you will understand them after a while. Indirect and direct approach General Suggestions: different approaches 1. Indirect approach-SLP is not working on any system specifically 1. Assisting the motor function (e.g. palatal lift, abdominal binders, surgery) Palatal Lift are done by dentist, teach person how to use Direct Approach Direct approach (SLP will work on the area affected; phonation, intensity, breathe support) Goal for the SLP: SLP will listen, determine what area needs to be remediated • See below General Strategies The clinician and the client will: a. Speak in a quiet environment implies that there is no competing noise. b. Speak face to face implies visual cues c. Teach client when to repeat, when to simplify and when to paraphrase. Severe Apraxia or Aphasia Severe Dysarthria/or Apraxia-consider an AAC if can’t understand the person a. communication board-picture board: picture of things that they need/feel/want b. communication book (e.g. C-book has section/or tabs like a food section, activity section and the patient turns to that page to express their needs/wants). The client will use his communication book to express his wants and needs. The client will point to a picutre c. electronic device (6 pictures to laptop to). The goal is for the client to produce S-V/S-V-0 sentences using his electronic device with 60%-100% with no cues. 5 factors for AAC List of AAC objects-Patient needs plus: 1. Cost of system-low functional-high functional ($1-$8000) a. not everyone has good insurance 2. Amount of training to use device (e.g. client and clinician training) a. SLP may needs hours of training before using the device, implement techniques 3. How does the system interfere with other activities? (e.g. person can not bring AAC to beach 4. Intelligibility of output (e.g. electronic voice on telephone) a. women voice, hanging up on electronic devices 5. Acceptability of system (everyone needs to accept the fact there is a device and give the client time to use the AAC device General Guidelines for Dysarthria Treatment of Severely Impaired Apraxia of speech-motor programing 1. Poor prognosis for apraxia of speech – a. one month with no volitional speech only stereo typical utterances (e.g. stereotypical utterances- patient says wiki wiki wiki wiki and can not get anything out.) b. after treatment for 1 month, the patient has not improved and every area for communication is severely impaired. 2. Poor prognosis-if patient has severe aphasia as well as severe apraxiacomorbidity..the type of aphasia associated with severe apraxia is global aphasia • Other Indication see below Treatment for Severe Apraxia 1. AAC device 2. multi- modalities communication 3. Single functional words 4. The SLP will educated family about what is speech apraxia and aphasia See notes below Characteristic of Moderate Apraxia Prognosis Indicators: 1. Poor prognosis-if patient has some volitional speech within one month Characterized by: 1. Moderate apraxia will have mild forms of other types of apraxia like limb 2. Moderate apraxia will have hemiplegia and hemipareis 3. Moderate apraxia will have a mild to moderate degrees of aphasia Treatment for Moderate Apraxia 1. SLP will use drill format to produce sounds Goal: the client will say functional words given from a functional word list with 80% accuracy given verbal and visual cues. the client will say a functional phrase given a verbal model from the clinician with 80% accuracy. the client will say a functional sentence without a verbal model.) 2. clinician will direct client to use words, phrase, to sentences 3. work-entry is possible with AAC. Some moderate aphasiacs will return to work and the SLP may suggest the use of an AAC device. Goal: the client will access his device, the client will produce a 2-3 word phrase using his AAC device with 80% given a clinician verbal prompt. Characteristic of Mild Aphasia Prognosis Indicators: 1. Mild apraxia have volitional speech, Dr. Isaki calls them functional speakers Characterized by: 1. Mild apraxia will have only mild aphasia 2. Mild apraxia will struggle with words and make errors, but they are cognitively aware of their problems with speech. If they are aware of the speech errors, they will correct it. Goal: the client will self-repair speech by repeating the word/phrase/sentence to the listener. Treatment Suggestions Treatment suggestions 1.SLP will target multi-syllabic word, phrases and sentences. 2. SLP wants the client to overcome speech apraxia The goal is work reentry.work-entry is a goal, clinician sets up therapy. (e.g. articulation therapy with children, you must model the sound. You don’t need to describe where the articulation need to go. The clinician will need a verbal model for them and they will repair the speech using their own skills. The clinician will give a verbal and visual model to show the client. 3. SLP should use Melodic Intonation Therapy (e.g. modeling) General Suggestion for Apraxia 1. SLP will make movements visible, short and simple. (e.g. substitute dad for father) 2. SLP will begin with functional items, instead of made-up words. SLP need to have functional and meaningful for adults. SLP should use functional 3.SLP will use Melodic Intonation Therapy: watch and listen. Goal: The client will watch and listen to the clinician use melodic intonation techniques and then the client will use melodic techniques to use produce/say a functional phrase, functional sentence with 100%. Functional Outcome Measures Functional Outcome measures 1. implement outcome measures (e.g. rating scales by the end of therapy and we will fill out the same measure.) 2. Measuring the gains of the client by rating a. rating scale is subjective b. areas of concerns are broad-(e.g. communication-will not show gains)functional independence measure (FIM score) c. interreliability rating with family, client and clinician What Do We Need to DO? Step 1. Determine what type of aphasia the client has from the data below? 1. Expressive Non-fluent (global, brocas, transcortical) vs. Expressive Fluent (Wernickes/Transcortical Sensory, Conduction/Anomic). Step 1a. Name the characteristic of the Aphasia. (e.g. Broca’s aphasia has telegraphic speech, use of content words like nouns and verbs.) Step 2 Step 2: Determine what to target for the patient? Determine the target that will make the most gains from the data). Determine the area that will make the most changes in the area of communication? 0. SLP will need to teach the client a specific skill in a short amount of time. (by targeting drawing, writing, and gestures, you are teaching strategies). The client will use sentence completion for anomia. The client will complete 5 fill in the blanks sentences about a semantic description of a functional targeted word , about procedural task with 60%-100% accuracy given a read passage. 1. If we work on word finding difficulties (anomia), we will improve communication. 2. How would sentence completion generalize to outside environments. A mild Brocas will need to come up strategies to repair the anomia. A strategy might be a phrase to remember that word, but it is all internal. Why do we use cues for the severely impaired aphasiacs? Not for mildly impaired, we can teach the strategies and the mild Broca’s can generalize to other environments. a. the 10+ strategies are not tasks. The client will use the strategy to complete a task. b. Mild/Moderate/Severe Aphasia, the clinician will use cues. What type of cues is the clinician using. Why do we use cues in STG? Because we are teaching them a new skill. What skills does the SLP teach to mild/moderate/severe Brocas? The clinician will explain/show the client by modeling, by explaining how. Problem: if the client can not say the word “key” and over 5 trials, the client still can’t say the word “key”. The clinician will need to find strategies to say the word “key”. A bad goal is simple to name the object over and over. A good goal will name a strategy to help say the word ‘key’. Goal; the client will use semantic descriptors/synomyms. The client will give 5 semantic descriptors for the functional targeted word with 60%100% accuracy given verbal/visual cues. The strategies are specific, you must be able to count the strategies..5 synomyms, antonyms, hypernyms, hyponyms, meronyms. Strategies are incorporated in the tasks to help the person name! During a conversation, you may use the 10+ strategies to find a word if you are mildly impaired. However, during a conversation with moderate or severe, the conversation will be impaired. Strategies will help the listener move onto the next steps of the conversations. In a completing a fill in a blank, you can use any of the strategies. The strategy will help the listener continue the conversation Step 3 Step 3: Write a goal for the client. Determine what type of cuing that will be used in therapy (target strengths) Goals should generalize to environments outside the clinic…at the store. Must write out Verbal, Visual, The client will decrease neolgism by substituting a real word in 70% accuracy with visual cue by drawing, verbal cue by repeating, tactile cue by tapping. confrontational naming: 70%-bad-compared to 100% before repetition of words: 60 %-bad-grade Auditory comprehension: Focus on 80% to 100%. Hospital setting, we only work on short term goals. We don’t know the affect of one-part onto two-part. Focusing on one-part and take baseline data. What is the hierarchy? targeting the goal is important. Generalization, how do we approach therapy through goals. Your therapy goals are on or off. one part: 80%-fair two part: 40%-bad..if the patient has master 2 part directions, you can move onto wh-questions, answer questions, or answer two questions. THINK of