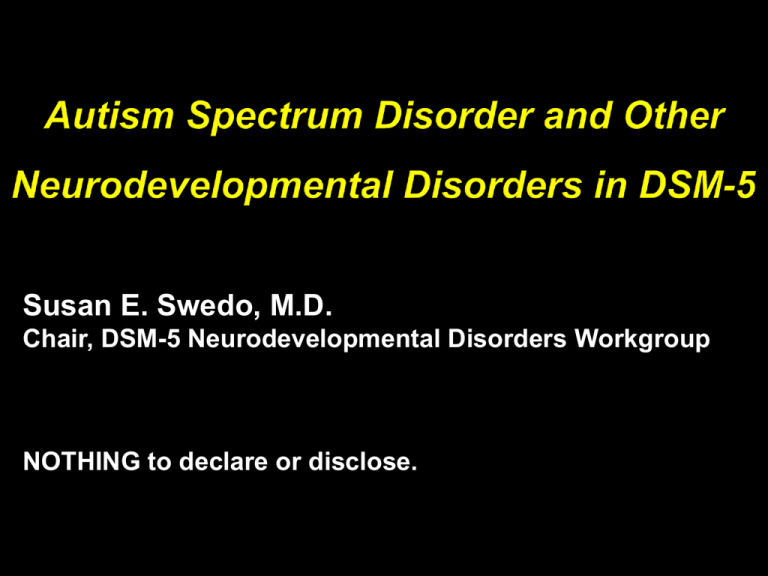
Susan E. Swedo, M.D.
Chair, DSM-5 Neurodevelopmental Disorders Workgroup
NOTHING to declare or disclose.
MEMBERS
ADVISORS
Gillian Baird
Ed Cook
Francesca Happe
James Harris
Walter Kaufmann
Bryan King
Catherine Lord
Joseph Piven
Rosemary Tannock
Sally Rogers
Sarah Spence
Susan Swedo
(Fred Volkmar)
Amy Wetherby
Harry Wright
Jim Bodfish
Martha Denckla
Maureen Lefton-Grief
Nickola Nelson
Sally Ozonoff
Diane Paul
Eva Petkova
Daniel Pine
Alya Reeve
Mabel Rice
Joseph Sergeant
Bennett & Sally Shaywitz
Audrey Thurm
Keith Widaman
Warren Zigman
Brief review of changes to
Intellectual disability (intellectual developmental
disorder)
Specific learning disorders
In-depth consideration of DSM-5 criteria for autism
spectrum disorder
Introducing severity ratings and specifiers
Relationship of ASD to Social (Pragmatic)
Communication Disorder
Performance of ASD criteria in field trials
Why should you care about DSM-5? Or, what is the
relationship of DSM-5 to ICD-10 and ICD-11?
A. Deficits in intellectual functions, such as reasoning, problem
solving, planning, abstract thinking, judgment, and academic
learning and learning from experience, confirmed by both clinical
assessment and individualized, standardized intelligence testing.
B. Deficits in adaptive functioning that result in failure to meet
developmental and sociocultural standards for personal
independence and social responsibility. Without ongoing support,
the adaptive deficits limit functioning in one or more activities of
daily life, such as communication, social participation, and
independent living, and across multiple environments, such as
home, school, work, and recreation.
C. Onset of intellectual and adaptive deficits during the
developmental period.
Reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorders,
Fifth Edition, (Copyright © 2013). American Psychiatric Association. All rights reserved.
DSM-IV
DSM-5
Reading Disorder
Specific Learning
Mathematics Disorder Disorder (Single
Disorder of Written
Category)
Expression
Learning Disorder
NOS
Use of specifiers
to define deficits
Rationale
Lack of evidence
for separation
(symptoms
overlap); need for
single “umbrella”
diagnosis.
Improved utility for
individual cases;
better represents
known
neuroscience
A. Difficulties learning and using academic skills, as indicated by the presence
of at least one of the following symptoms that have persisted for at least
6 mos, despite provision of interventions that target the difficulties:
Inaccurate or slow and effortful word reading (e.g., reads single words aloud incorrectly or
slowly and hesitantly, frequently guesses words, has difficulty sounding out words).
Difficulty understanding the meaning of what is read (e.g., may read text accurately but not
understand the sequence, relationships, inferences, or deeper meanings of what is
read).
Difficulties with spelling (e.g., may add, omit, or substitute vowels or consonants).
Difficulties with written expression (e.g., makes multiple grammatical or punctuation errors
within sentences; employs poor paragraph organization; written expression of ideas lacks
clarity).
Difficulties mastering number sense, number facts, or calculation (e.g., has poor
understanding of numbers, their magnitude, and relationships; counts on fingers to add
single-digit numbers instead of recalling the math fact as peers do; gets lost in the midst
of arithmetic computation and may switch procedures).
Difficulties with mathematical reasoning (e.g., has severe difficulty applying mathematical
concepts, facts, or procedures to solve quantitative problems).
B. The affected academic skills are substantially and quantifiably
below those expected for the individual’s chronological age, based
on appropriate standardized measures, and cause significant
interference with academic or occupational performance or with
activities of daily living.
C. The learning difficulties begin during school-age years but may not
become fully manifest until learning demands exceed the
individual’s limited capacities.
D. The learning difficulties are not better accounted for by intellectual
disabilities, global developmental delay, uncorrected visual or
auditory acuity, other mental or neurological disorders,
psychosocial adversity, lack of proficiency in the language of
academic instruction, or inadequate educational instruction.
Reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorders,
Fifth Edition, (Copyright © 2013). American Psychiatric Association. All rights reserved.
PDD will be replaced by Autism Spectrum
Disorder (ASD) with individual diagnoses
merged into a single, behaviorally defined
disorder
Three diagnostic domains will become
two (Social communication and
Restricted, repetitive behaviors)
Rett Disorder and other etiologic
subgroups will be described by use of a
Specifier: Associated with Known Medical
or Genetic Condition or Environmental
Factor
Delete the term “Pervasive Developmental
Disorders”
Symptoms are not pervasive – they are specific to social-
communication domain plus restricted, repetitive
behaviors/fixated interests
Overuse of PDD-NOS leads to diagnostic confusion (and
may have contributed to autism “epidemic”)
Overlap of PDD-NOS and Asperger disorder (and
autistic disorder)
New diagnostic category: “Autism Spectrum
Disorder” reflects current terminology in field.
DSM-IV (Pervasive developmental disorders)
Autistic Disorder
Asperger Disorder (relationship to “Aspies”)
Pervasive Developmental Disorder NOS
Childhood Disintegrative Disorder
Rett Disorder
DSM-5
Autism Spectrum Disorder
DSM-IV
Social
Communication (primarily verbal abilities)
Restricted and Repetitive behaviors
DSM-5
Social Interaction/Social Communication
Restricted and Repetitive behaviors
A. Persistent deficits in social communication and social interaction
across multiple contexts, as manifested by the following, currently
or by history (examples are illustrative, not exhaustive; see text):
1. Deficits in social-emotional reciprocity, ranging, for example, from
abnormal social approach and failure of normal back and forth
conversation; to reduced sharing of interests, emotions, or affect; to
failure to initiate or respond to social interactions.
2. Deficits in nonverbal communicative behaviors used for social
interaction, ranging, for example, from poorly integrated verbal and
nonverbal communication; to abnormalities in eye contact and bodylanguage or deficits in understanding and use of gestures; to a total
lack of facial expressions and nonverbal communication.
3. Deficits in developing, maintaining, and understanding relationships,
ranging, for example, from difficulties adjusting behavior to suit
various social contexts; to difficulties in sharing imaginative play or in
making friends; to absence of interest in peers.
Reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorders,
Fifth Edition, (Copyright © 2013). American Psychiatric Association. All rights reserved.
B. Restricted, repetitive patterns of behavior, interests, or activities, as
manifested by at least two of the following, currently or by history
(examples are illustrative not exhaustive; see text):
1. Stereotyped or repetitive motor movements, use of objects, or speech
(e.g., simple motor stereotypies, lining up toys or flipping plates,
echolalia, idiosyncratic phrases).
2. Insistence on sameness, inflexible adherence to routines, or ritualized
patterns of verbal or nonverbal behavior (e.g., extreme distress at
small changes, difficulties with transitions, rigid thinking patterns,
greeting rituals, need to take same route or eat same food every day).
3. Highly restricted, fixated interests that are abnormal in intensity or
focus (e.g., strong attachment to or preoccupation with unusual
objects, excessively circumscribed or perseverative interests).
4. Hyper-or hyporeactivity to sensory input or unusual interest in sensory
aspects of the environment (e.g., apparent indifference to
pain/temperature, adverse response to specific sounds or textures,
excessive smelling or touching of objects, visual fascination with lights
or movement).
Reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition,
(Copyright © 2013). American Psychiatric Association. All rights reserved.
C. Symptoms must be present in the early developmental
period (but may not become fully manifest until social
demands exceed limited capacities, or may be masked by
learned strategies in later life).
D. Symptoms cause clinically significant impairment in social,
occupational, or other important areas of current functioning.
E. These disturbances are not better explained by intellectual
disability or global developmental delays. Intellectual
disabilities and autism spectrum disorder frequently co-occur;
to make comorbid diagnoses of autism spectrum disorder and
intellectual disability, social communication should be below
that expected for general developmental level.
Reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorders,
Fifth Edition, (Copyright © 2013). American Psychiatric Association. All rights reserved.
Sensitivity has been “sacrificed” in order to
improve specificity
Social communication domain
Restrictive interests and repetitive behaviors domain
Merging Asperger disorder (and PDD-NOS)
into autism spectrum disorder results in loss of
identity and ignores uniqueness of Asperger dx
Pre-/post DSM-5 research studies won’t be
comparable
DSM-IV
DSM-5 Proposed
For subcriterion A.3,
DSM-IV checklist item is “failure to develop
peer relationships and abnormal social
play.”
DSM-5 recommendations include higherorder impairments of “difficulties adjusting
behavior to suit different social contexts.
For criterion C, DSM-IV requires that
symptoms begin prior to the age of 3 years.
The DSM-5 requires that symptoms begin in
early childhood, with the caveat that
“symptoms may not be fully manifest until
social demands exceed capacity” (during
middle-school years, later adolescence, or
young adulthood).
Scientific validity
Lack of specificity and sensitivity in
separating the diagnoses
Lack of accurate historical information
about very early language development
put emphasis on current speech
(trainable)
Overlap in samples when VIQ controlled
Consideration of access to services
2102 validated singletons with ASD;
8500 family members (two biological parents
and, in most cases, at least one unaffected
sibling) with DNA and intensive behavioral
and neuropsychological phenotyping
Recruited from 12 sites in the US and Canada
ADOS Social Affect
From: A Multisite Study of the Clinical Diagnosis of Different Autism Spectrum Disorders
Arch Gen Psychiatry. 2012;69(3):306-313. doi:10.1001/archgenpsychiatry.2011.148
Figure Legend:
Figure 1. Best-estimate clinical diagnoses across 12 university-based sites (ie, autism service providers) for 2102 probands
assigned to 3 autism spectrum disorder diagnostic categories (autistic disorder, Asperger syndrome, and pervasive developmental
disorder–not otherwise specified [PDD-NOS]).
Date of download: 11/26/2012
Copyright © 2012 American Medical
Association. All rights reserved.
From: A Multisite Study of the Clinical Diagnosis of Different Autism Spectrum Disorders
Arch Gen Psychiatry. 2012;69(3):306-313. doi:10.1001/archgenpsychiatry.2011.148
Figure Legend:
Figure 2. Classification and regression tree (CART.2 model) for best-estimate clinical diagnoses with diagnostic scales, site, and
diagnostician characteristics as predictors. The sets of numbers separated by slashes denote the numbers for each diagnostic
group: autistic disorder (AUT)/pervasive developmental disorder–not otherwise specified (PDD)/Asperger syndrome (ASP). ADIRRB indicates Autism Diagnostic Interview–Revised restricted and repetitive behaviors total score; ADI-social, ADI-R social total
score; ADI-VC, ADI-R verbal communication total
score; ADOS-CSS,
Autism
Diagnostic Observation Schedule calibrated severity
Copyright
© 2012 American
Medical
Date
ofADOS-RRB,
download: 11/26/2012
score;
ADOS restricted and repetitiveAssociation.
behaviors total
score;
ADOS-soc+com,
ADOS social and communication domain
All rights reserved.
total score; Yr Exp, senior diagnostician's number of years of experience.
Severity of ASD Symptoms
Pattern of Onset and Clinical Course
Etiologic factors
Associated conditions
Individual weaknesses and strengths
CLINICIANS WILL BE ENCOURAGED TO
DESCRIBE THESE DETAILS WITH
DIAGNOSTIC SPECIFIERS
Age and pattern of onset
With /without loss of established skills
With/without accompanying intellectual impairment
With/without accompanying structural language
impairment
Associated with a known medical or genetic
condition or environmental factor
Associated with another neurodevelopmental,
mental, or behavioral disorder
Severity of symptoms
No causal factors in ASD
i.e. presence of a risk factor will not predict ASD >
90% of the time
ID has “causal” loci but nothing else in DSM5
Due to some specific factors being so severe that
even with variability ID is present (e.g. maternal
deletion of 15q11-q13 – Angelman syndrome)
Examples – Rett disorder, Fragile X
syndrome, fetal alcohol syndrome
E.g., ADHD - had been specifically excluded as a
comorbid diagnosis in DSM-IV, yet 20-40% of
pts with ASD have ADHD.
No exclusionary comorbidities
Specifiers role is to indicate additional disorder
present and help clinician consider the impact
of that dx on presentation of ASD
Co-occurring disorder should be separately
coded and recorded
NO overall rating of ASD severity
Social Communication Impairment (level 1,2,3)
Restricted interests/Repetitive Behaviors (level 1,2,3)
Level 1 – requiring support
Level 2 – requiring substantial support
Level 3 – requiring very substantial support
Severity Level
Social Communication
Severe deficits in verbal and nonverbal social
Level 3
communication skills cause severe impairments
‘Requiring very substantial in functioning; very limited initiation of social
interactions and minimal response to social
support’
overtures from others.
Level 2
‘Requiring substantial
support’
Level 1
‘Requiring support’
Restricted, repetitive behaviors
Inflexibility of behavior, extreme difficulty
coping with change, or other
restricted/repetitive behaviors markedly
interfere with functioning in all spheres.
Great distress/difficulty changing focus or
action.
Marked deficits in verbal and nonverbal social
communication skills; social impairments
apparent even with supports in place; limited
initiation of social interactions and reduced or
abnormal response to social overtures from
others.
Inflexibility of behavior, difficulty coping with
change, or other restricted/repetitive
behaviors appear frequently enough to be
obvious to the casual observer and interfere
with functioning in a variety of contexts.
Distress and/or difficulty changing focus or
action.
Without supports in place, deficits in social
communication cause noticeable impairments.
Has difficulty initiating social interactions and
demonstrates clear examples of atypical or
unsuccessful responses to social overtures of
others. May appear to have decreased interest in
social interactions.
Inflexibility of behavior causes significant
interference with functioning in one or more
contexts. Difficulty switching between
activities. Problems of organization and
planning hamper independence.
1) Persistent difficulties in the social use of verbal and nonverbal
communication as manifest by deficits in all of the following:
Deficits in using communication for social purposes, such as greeting and
sharing information, in a manner that is appropriate for the social context
Impairment in the ability to change communication to match context or
the needs of the listener, such as speaking differently in a classroom than
on a playground, talking differently to a child than to an adult, and
avoiding use of overly formal language
Difficulties following rules for conversation and storytelling, such as
taking turns in conversation, rephrasing when misunderstood, and
knowing how to use verbal and nonverbal signals to regulate interaction
Difficulties understanding what is not explicitly stated (e.g., making
inferences) and nonliteral or ambiguous meanings of language, for
example, idioms, humor, metaphors and multiple meanings that depend
on the context for interpretation
2) Deficits result in functional limitations in effective
communication, social participation, social relationships,
academic achievement, or occupational performance.
3) Deficits must be present in the early developmental
period, but may not become fully manifest until social
communication demands exceed limited capacities.
4) Deficits are not better explained by autism spectrum
disorder, intellectual disability (intellectual development
disorder), global developmental delay, or another
mental disorder or medical condition.
Diagnosis is needed for:
Children with current dx of PDD-NOS made solely on the
basis of social communication deficits
Individuals with significant social skills deficits (e.g.
children with ADHD)
Individuals with “subthreshold” symptoms
Should NOT be included in ASD section because it
defines a group of individuals with related, but
separate symptoms
Criteria appeared to function well in field trials
DSM-5 criteria represent consensus of clinicians
and investigators on best description of autistic
spectrum disorder (and other ND’s)
Efforts to “harmonize” DSM-5 and ICD criteria
began in 2010 and are ongoing.
ICD-11 will likely retain separation of autistic
disorder from other autism “spectrum” disorders
but criteria are quite comparable
Research publications will be required to use
DSM-5 criteria for “Expert Clinician’s Judgment”.
ASD is already
preferred term for
research (over PDD
or individual dx’s)
ADI-R and ADOS
are diagnostic
standards for
research
NUI Galway
Dr. Geraldine Leader
Dr. Louise Gallagher
Ms. Patricia Walsh
Autism Speaks
Dr. Amy Daniels
Dr. Andy Shih
American Psychiatric
Association, and the
DSM-5 Task Force
Dr. David Kupfer
Dr. Darrel Regier
MEMBERS of DSM-5 Workgroup
Gillian Baird
Ed Cook
Francesca Happe
James Harris
Walter Kaufmann
Bryan King
Catherine Lord
Joseph Piven
Rosemary Tannock
Sally Rogers
Sarah Spence
Amy Wetherby
Harry Wright