Cutting Too Deep? Assessing the Impact of a Shorter Surgery
advertisement

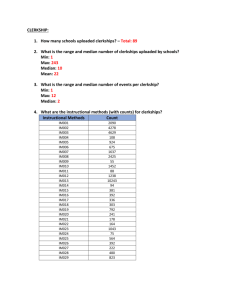
Cutting Too Deep? Assessing the Impact of a Shorter Surgery Clerkship on Students’ Clinical Skills and Knowledge Navin D. Bhatia, Colleen C. Gillespie, Alexandra J. Berger, Mark S. Hochberg, Jennifer B. Ogilvie New York University School of Medicine 04/23/2013 Background •In 2011, the New York University School of Medicine initiated implementation of a new Curriculum for the 21st Century •Changes to the core clinical year included shortening of the Surgery Clerkship from 8 weeks to 6 •Previous school-specific studies have found a decline in student performance following such a reduction in surgery clerkship length1 •We sought to evaluate the impact of this new clerkship duration on medical students’ performance in an Objective Structured Clinical Examination (OSCE) and the National Board of Medical Examiners (NBME) Clinical Science Surgery Examination 1 Lind et al, J Surg Res, 1999. Cutting Too Deep? Assessing the Impact of a Shorter Surgery Clerkship on Students’ Clinical Skills and Knowledge 2 Methods • 214 medical students from 2010-2011 were included in the study • 115 from the first four blocks of the 8-week clerkship • 99 from the first four blocks of the 6-week clerkship • Performance on an end-of-clerkship OSCE was calculated across 8 sub-domains, using a behaviorally-anchored checklist • Scores were calculated as the mean of relevant items • Response options: Not Done, Partly Done, Done • NBME exams were assessed by the NBME, using standard scaled scores • Results were compared using a 2-tailed, independent-sample, unequal variance t-test Cutting Too Deep? Assessing the Impact of a Shorter Surgery Clerkship on Students’ Clinical Skills and Knowledge 3 OSCE Grading Sheet Cutting Too Deep? Assessing the Impact of a Shorter Surgery Clerkship on Students’ Clinical Skills and Knowledge 4 OSCE Grading Sheet Cutting Too Deep? Assessing the Impact of a Shorter Surgery Clerkship on Students’ Clinical Skills and Knowledge 5 Results • Mean Overall OSCE scores did not statistically differ between the 6 week (92.92, SD 6.01) and 8 week (93.21, SD 5.64) clerkships (t =.37, p=.71) • Mean NBME exam results in the 6 and 8-week clerkships (75.26 vs. 76.13) were also not found to be statistically different (t=.81, p=.42) • Students in the 6-week clerkship performed better in four of the 8 OSCE sub-domains: • • • • Blood pressure measurement Orthostatic blood pressure measurement Rectal exam Fecal occult blood test Cutting Too Deep? Assessing the Impact of a Shorter Surgery Clerkship on Students’ Clinical Skills and Knowledge 6 Results Cutting Too Deep? Assessing the Impact of a Shorter Surgery Clerkship on Students’ Clinical Skills and Knowledge 7 Results Cutting Too Deep? Assessing the Impact of a Shorter Surgery Clerkship on Students’ Clinical Skills and Knowledge 8 Results Cutting Too Deep? Assessing the Impact of a Shorter Surgery Clerkship on Students’ Clinical Skills and Knowledge 9 Conclusions • Overall clinical performance in a summative OSCE and the NBME exam did not differ between students in an 8 week vs. 6 week surgery clerkship • Students in the 6-week clerkship performed better in specific procedural components of the OSCE, including BP measurement and rectal/fecal occult blood exams • Further research will explore whether this enhanced clinical performance in specific competencies was due to differences in clinical training prior to the clerkship, and/or differences in the composition of the student classes Cutting Too Deep? Assessing the Impact of a Shorter Surgery Clerkship on Students’ Clinical Skills and Knowledge 10