6. WLMHT Presentation - Mental Health & Learning Disability Nurse

Enhanced Engagement and Observation:
Gillian Kelly, Acting Deputy Director of Nursing
Francis Thompson, Head of Nursing Education & Standards
Paul Knowles, Patient Safety Lead
West London Mental Health NHS Trust
• Provide care and treatment for about 20,000 people a year and serve a population of 700,000 residents
• A large Trust employing some 4,300 staff and serve a local community of many races, religions and languages, across four London boroughs. This includes local mental health services for adults, older people and children in the boroughs of Ealing, Hammersmith & Fulham and
Hounslow.
• Our high secure services at Broadmoor Hospital in
Berkshire are internationally recognised. With our West
London Forensic Service, they make us a leading national provider of secure and specialist mental healthcare.
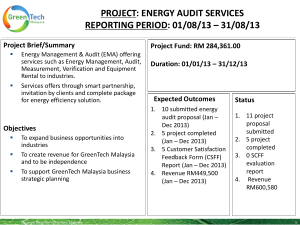
SUI’s 2013
40
35
30
25
20
15
10
5
0
34
16
7
Trust SUI's Inpatient SUI's EE and O link
Trustwide incidents
HSS Broadmoor Hospital
Paul Knowles
Patient Safety Lead/Practice Development Nurse
& Modern Matron
Recent Historical Issues
• 2 Recent SUI reviews into patient deaths (last 2 years) highlighted contributory factors regarding EE&O practice
(particularly during night shift).
• 5 staff have recently (last 2 years) been either dismissed or had local and or NMC sanctions against them for failing to adhere to policy re EE&O’s.
• Rooms and site poorly designed (particularly Victorian buildings) do not necessarily support EE&O’s.
Actions taken
• Routine review of CCTV by local nurse managers
• Routine audits of EE&O practice by Senior Clinical
Mangers
• Unannounced out of routine hours audit of EE&O practice by Practice Development Nurses
• Review of mandatory training to include simulation of practice
• All staff to be assessed as having necessary skills and understanding by their local manager before carrying out
EE&O’s
• Learning Lessons events with particular focus on EE&O practice
• SOP for nurses I/C of shifts with clear instructions for monitoring EE&O practice during the shift
Future developments
• Electronic Monitoring: a) Heart rate monitors b) CO2 monitors c) Movement recognition
• Recently announced rebuild a) Room design and observational windows reworked to take into account EE&O’s b) Line of site observation generally much improved part of design brief
Forensic Services
Clinical audit and the cycle of improvement
Gillian Kelly, Acting Deputy Director of Nursing
Aims
• Discuss experience and approach to EE&O audit with
Specialist & Forensic CSU
– What we found
– What we did
– What we still need to do
The Initial Audit Findings: What we found:
July/Aug’ 12
• Some good practice
• Areas of concern and significant risk
• Preventing suicide components particularly concerning
– risk assessment and management, engagement, care planning, activities and documentation
• Staff awareness of requirements below acceptable standards
• Patient involvement and information sharing below acceptable standards
– not feeling safe, respected and that privacy/dignity is not maintained
– Not receiving copy of care plan
The Formula: What we did
• Monthly spot-check audits
• Approach:
– Team working across operational/Practice
Development Roles -real strength in approach / pooled resources / fun / enhanced ownership / variety of experiences
– Spot-checking / clinical areas not notified in advance
– Initial auditors: Senior Nurses (8a>)
– Pre-audit meeting/planning (teams allocated)
– Team/Buddy system - allocated areas outside of normal workplace
– Audit Day nominated / combined with WM’s meetings
The Formula: What we did
• Immediate remedial actions are taken when auditors identify failures in EE&O practice
– systemic and individual errors addressed
• Post audit debriefs/discussions of findings held with ward managers and senior nurses to discuss issues and remedial actions shared; identifying actions requiring follow-up and priority areas for improvement (lessons learnt) whilst awaiting formal data analysis from audit
• WM’s later involved in auditing to enhance ownership and raise awareness – healthy competitiveness developed / real pride in achievements
• Audit report also discussed at WM’s Meetings
Actions Taken
GOVERNANCE
• EE&O included in CSU risk register
• EE&O included within Suicide Prevention Strategy
• Ongoing audit and reports discussed in Gov meetings
PRACTICE
• Remedial actions/debriefs as described
• Directive from the DDN regarding accountability and areas for immediate action
• Email from DDN - commending improvements and highlighting areas for ongoing development
TRAINING
• EE&O Tutorials
• Enhanced Engagement for HCAs and B5 workshops
Going Forward: What we still need to do
• Still room for improvements
• Serious Incidents / High Risk Areas
– where should we focus practice development initiatives? (high and low usage areas)
• Quarterly V’s Monthly audit?
• Who should undertake the audit? (MDT involvement /
Band 5 / preceptees / Senior Nurses Qrtly)
• Need for mandatory training in this area
• Next audit important for understanding if improvements have been sustained
• SU perspectives/involvement
Any questions / thoughts?