Metropolitan Health Plan - Long Term Quality Alliance
advertisement

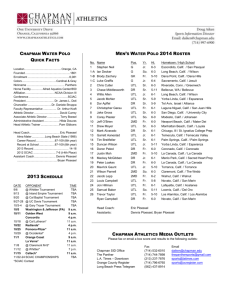
About the Association for Community Affiliated Plans September 2014 ACAP’s Mission To represent and strengthen not-for-profit safety net health plans as they work with providers and caregivers in their communities to improve the health and well-being of vulnerable populations in a cost-effective manner. 2 ACAP Represents 58 Safety Net Health Plans Arizona University of Arizona Health Plans California Alameda Alliance for Health CalOptima CenCal Health Central California Alliance for Health Community Health Group Contra Costa Health Plan Gold Coast Health Plan Health Plan of San Joaquin Health Plan of San Mateo Inland Empire Health Plan Kern Family Health Care L.A. Care Health Plan Partnership HealthPlan of California Santa Clara Family Health Plan San Francisco Health Plan Colorado Colorado Access Denver Health Connecticut Community Health Network of Connecticut District of Columbia Health Services for Children With Special Needs Florida Prestige Health Choice Hawaii AlohaCare Illinois Family Health Network Indiana MDwise Kentucky Passport Health Plan Maryland Maryland Community Health System Priority Partners Massachusetts Boston Medical Center HealthNet Plan Commonwealth Care Alliance Neighborhood Health Plan Network Health 3 ACAP Represents 58 Safety Net Health Plans Minnesota Metropolitan Health Plan New Hampshire Well Sense Health Plan New Jersey Horizon NJ Health New York Affinity Health Plan Amida Care Elderplan & Homefirst GuildNet Hudson Health Plan Monroe Plan for Medical Care, Inc. Univera Community Health VillageCareMAX VNSNY CHOICE Ohio CareSource Oregon CareOregon Pennsylvania AmeriHealth Caritas Pennsylvania UPMC for You Rhode Island Neighborhood Health Plan of Rhode Island Texas Children’s Medical Center Health Plan* Community Health Choice Cook Children’s Health Plan Driscoll Health Plan El Paso First Health Plans Sendero Health Plan Texas Children’s Health Plan Virginia Virginia Premier Washington Community Health Plan of Washington Wisconsin Children’s Community Health Plan *Incubator plan. 4 ACAP’s 58 Plans are in 24 States 5 23 ACAP Plans Operate SNPs • • • • • • • • • • Affinity Health Plan (N.Y.) Alameda Alliance for Health (Calif.)* AlohaCare (Hawaii) AmidaCare (N.Y.) CalOptima (Calif.) CareOregon (Ore.) CareSource (Ohio)* Colorado Access (Colo.) Commonwealth Care Alliance (Mass.) Community Care Alliance of Illinois/FHN (Illinois) • Community Health Group (Calif.) • Community Health Plan (Wash.) • Denver Health Medical Plan (Colo.) • Elderplan & Homefirst (N.Y.) • GuildNet (N.Y.) • Health Plan of San Mateo (Calif.) • Inland Empire Health Plan (Calif.) • L.A. Care Health Plan (Calif.) • Metropolitan Health Plan (Minn.)* • Partnership HealthPlan of California* • University of Arizona Health Plan** • UPMC for You (Pa.) • VNSNY CHOICE Health Plans (N.Y.) * Operating SNP through 2014. ** Entering SNP market in 2015. 6 17 ACAP MLTC Plans • • • • • • • • • Affinity Health Plan (N.Y.) Alameda Alliance for Health (Calif.) Amida Care (N.Y.) CalOptima (Calif.) Commonwealth Care Alliance (Mass.) Community Health Group (Calif.) Elderplan & Homefirst (N.Y.) Guildnet (N.Y.) Health Plan of San Mateo (Calif.) • • • • • • • • Horizon NJ Health Inland Empire Health Plan (Calif.) L.A. Care Health Plan (Calif.) Metropolitan Health Plan (Minn.) Neighborhood Health Plan of R.I. Santa Clara Family Health Plan (Calif.) VillageCareMAX (N.Y.) VNSNY CHOICE Health Plans (N.Y.) 7 17 ACAP Plans Planning or Participating in Duals Demos California: Alameda Alliance for Health*; CalOptima*; Community Health Group of San Diego; Health Plan of San Mateo; Inland Empire Health Plan; L.A. Care; Santa Clara Family Health Plan*. Massachusetts: Commonwealth Care Alliance; Network Health Minnesota (D-SNP Model): Metropolitan Health Plan*** New York: Elderplan/HomeFirst, GuildNet, VillageCareMAX, VNSNY Choice Health Plans Ohio: CareSource Rhode Island: Neighborhood Health Plan of R.I.** Virginia: Virginia Premier Health Plan Other ACAP plans are in non-demo duals initiatives * Delayed ** LTC services began Nov. 2013; Medicare services included in 2015 *** MHP leaving MSHO demo in 1/15 8 Contact Mary Kennedy | Vice President |Medicare and Managed Long Term Care Association for Community Affiliated Plans 1015 15th St. NW Suite 950 | Washington, DC 20005 Direct: (202) 701-4749 1015 15th St. NW, Suite 950 Washington, DC 20005 mkennedy@communityplans.net Web: www.communityplans.net 9 Minnesota Senior Health Options Sue Kvendru Minnesota Department of Human Services Minnesota Experience Medicaid Managed Care since 1985 Minnesota Senior Health Options since 1997 Initially Medicare Payment Demo D-SNP ( Initial MOU with CMS to transition) MOU with CMS for Alternative Demo signed September, 2013 – Not a Financial Alignment Demo (FAD) Minnesota Senior Health Options (MSHO) Combines Medicare (including Part D) and Medicaid services Includes Elderly Waiver (MLTSS) Includes 180 days of nursing home care Enrollment is voluntary instead of mandatory enrollment in Medicaid Managed Care program (MSC+) 70% have chosen to enroll in MSHO Approximately 36,000 enrolled Operating statewide All eight MSC+ (Medicaid managed care) plans participate MSHO Features: Overview Integrated member materials, one enrollment form, aligned enrollment dates, one card for all services State MLTSS assessment tool integrates Health Risk Assessment (HRA into assessment process All members are assigned individual care coordinators. The State sets uniform standards, audit protocols and criteria for care plans, face to face assessment and care coordination Flexible care coordination delivery models High degree of collaboration among SNPs and State on member materials, PIPs, care coordination, benefit policy, demo decisions, etc. through multiple joint workgroups Health plans waive Medicaid co-pays for members State level Stakeholders group, each SNP also has local stakeholders group. Aligned capitated financing supports innovation and payment reform Minnesota Demonstration “Demonstration to Align Administrative Systems for Improvement in Beneficiary Experience” Charts a new demo option path for improving States’ ability to work with Medicare Advantage Dual-Eligible Special Needs Plans (D-SNPs) Builds on current D-SNPs Current SNP and Medicaid financing and rates • HEDIS: 98% of MSHO seniors have annual primary care visits • Dual database: MSHO risk adjusted hospital admits/episode rates lower than FFS Medicare Medicare Advantage (Source: JEN iMMRS-MN) • S&Ps and STARS: MSHO D-SNPs have been high performing on STARS and SNP S&P measures • CAHPS: MSHO is highest rated MN Medicaid program; includes care coordination questions • Disenrollment rates: < 2% • Encounter data analysis: Increased HCBS access through annual face to face assessment/individualized care coordination • AARP scorecard: MN has been #1 for HCBS Access. – Minnesota has rebalanced its MLTSS system from 63% NF and 9.5% community waivers in 1996 to 24% NF and 39% community waivers in 2012. – See Rebalancing Graph (Sources: 1996 Medicaid Forecast, July 2012 Medicaid enrollment by living arrangement). Contact Info Sue Kvendru, Managed Care ( Seniors) • • 651-431-2517 sue.kvendru@state.mn.us Deborah Maruska, Managed Care (People with Disabilities) • • 651-431-2516 deb.maruska@state.mn.us Key Attributes of Integrated Health Organizations and Person-Centered Innovations September 18, 2014 Sarah Barth, JD Director of Integrated Health and Long-Term Services www.chcs.org Integrated Care Projects at CHCS • Implementing New Systems of Integration for Dual Eligibles (INSIDE) ► ► Brings together 16 states for group learning, innovation sharing, and opportunities to work with federal partners Supported by The SCAN Foundation and The Commonwealth Fund • Promoting Integrated Care for Dual Eligibles (PRIDE) ► ► ► Brings together 7 integrated health organizations to identify and test innovative strategies that enhance and integrate care for Medicare-Medicaid enrollees PRIDE consortium membership: CareSource (OH); Commonwealth Care Alliance (MA); Health Plan of San Mateo (CA); iCare (WI); Together4Health (IL); UCare (MN); VNSNY CHOICE (NY) Supported by The Commonwealth Fund • Integrated Care Resource Center (ICRC) ► ► Established by CMS to help states advance integrated care delivery for Medicare-Medicaid enrollees Technical assistance and online resources provided by CHCS and Mathematica Policy Research 19 PRIDE Framework for High-Performing Integrated Health Plans Attributes in 5 Domains: 1. Leadership and Organizational Culture 2. Infrastructure to “Scale Up” and “Stretch Out” While Maintaining Quality and Value 3. Financial and Nonfinancial Incentives and Related Mechanisms that Align Plan, Provider, and Member Interests 4. Coordinated Care Provided through Comprehensive, Accessible Networks and Person/Family-Centered Care Planning and Coordination 5. Capacity to Attract and Retain Members, Expand Enrollment, and Increase Retention 20 Person-Centered PRIDE Projects CareSource 360 degree view of individuals’ care needs Commonwealth Care Alliance Improving documentation of care plans for fluidity and person-centeredness Health Plan of San Mateo Pilot project providing supplemental residential supports UCare Making assessments more person-centered and culturally sensitive iCare Building independence through person-centered planning for PCA services VNSNY CHOICE Making care planning more person-centered Together4Health Addressing social determinants of health from the beginning 21