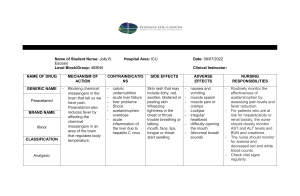
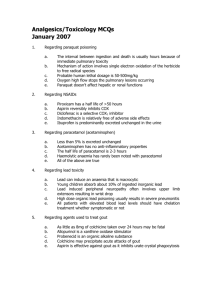
ANALGESICS Analgesics • Analgesics are drugs that relieve pains • They are capable of producing analgesia • Pain is subjective • Description of intensity of pain Mild Moderate Severe Types of pain Acute pain Chronic pain Nociceptive pain Neuropathic pain Psychogenic pain Physiology of pain 1. Transduction Mechanical, chemical or thermal stimulus is converted into a biological signal Inflammation causes nearby immune cells to release neurotransmitters such as serotonin, histamine, prostaglandins, bradykinin, and substance P that can trigger pain Nociceptors are activated to generate action potential 2. Transmission Action potential are transmitted from the site of injury to spinal cord and cerebral cortex of the brain for processing 3. Perception cerebral cortex processes the experience of pain and its characteristics such as location, intensity, and what makes the pain better or worse • Modulation descending neurons travel from brainstem and release neuromodulators such as endorphins and enkephalins which inhibit the transmission of pain signals and produce analgesic (painrelieving) effects Classification of analgesics 1. Opioids 2. Non-opioids 3. Adjuvants OPIOIDS • They work by binding to specific receptors in the central nervous system • e.g. morphine, codeine, oxycodone, hydrocodone, hydromorphone, oxymorphone, pethidine, tramadol and fentanyl Morphine Indications • Moderate to severe pain such as: Pain from surgery, trauma Advanced illnesses such as cancer Myocardial infarction Dyspnea (shortness of breath) Morphine Mechanism of action • Morphine binds to opioid receptors in the CNS • Alters the perception of pain by inhibiting the transmission of pain signals • Alters the response to painful stimuli by activation of receptors leading to feelings of euphoria, relaxation, and an altered sense of well-being Morphine Contraindications • Hypersensitivity or allergy to morphine • Respiratory depression • Paralytic ileus • Head injury or Increased Intracranial Pressure • Acute alcohol intoxication or drug abuse • Use of Monoamine Oxidase Inhibitors (MAOIs) Morphine Side effects Respiratory depression Confusion Hypotension Dizziness Sedation Constipation Nausea and vomiting Acute urinary retention Elevation of intracranial pressure, particularly in head injury Morphine Drug interactions • CNS depressants (e.g., barbiturates, benzodiazepines, alcohol) • Anticholinergic drugs (e.g., antihistamines, tricyclic antidepressants, atropine-like drugs) can exacerbate morphine-induced constipation and urinary retention • Antihypertensive drugs can exacerbate morphine induced hypotension • Naloxone (narcan) suppress the symptoms of opioid overdose Morphine Nursing considerations 1. Use supportive nursing measures as relaxation techniques to relieve pain before using narcotics 2. Explore the source of pain, use non-narcotic analgesia if possible 3. Administer the medication when needed 4. Monitor mental status 5. Monitor Respiratory rate (drug may lead to respiratory depression) 6. Monitor blood pressure (hypotension may occur) 7. Monitor pulse rate (if 60/m withhold the drug) 8. Watch for constricted pupils. Document it and notify the physician 9. Monitor bowel function, since drug may cause constipation 10.Encourage client to empty bladder every 3-4 hrs (since drug may cause urinary retention) 11.Inform the client/family that the drug may become habit forming and leading to addiction 12.Document any history of asthma or other contraindications 13.Have emergency equipment and narcotic antagonist available 14.Naloxone is used to reverse opioid such as morphine overdose Pethidine (Meperidine) • Pethidine is a synthetic opioid analgesic medication used primarily for the relief of moderate to severe pain. It shares most pharmacological properties with morphine NON-OPIOIDS • Mechanisms: Reducing inflammation Blocking pain signals Altering pain perception NON-OPIOIDS • Types of non-opioid analgesics: Acetaminophen (paracetamol) Non-steroidal Anti-Inflammatory Drugs (NSAIDs). E.g. ibuprofen and diclofenac Salicylates e.g. aspirin Paracetamol (Acetaminophen) Mechanism of action: • Works in the CNS to inhibit the synthesis of prostaglandins Paracetamol (Acetaminophen) Indications: Mild to moderate pains Fever Headache Toothache Osteoarthritis Colds and flu symptoms Sore throat Paracetamol (Acetaminophen) Side effects / adverse effects Rashes Blood disorders (e.g. thrombocytopenia, leucopenia, neutropenia) Hypotension Flushing Tachycardia also reported on infusion Liver damage Nursing considerations for paracetamol 1. Inform patients about the risk of liver injury 2. Assess pain prior to and after administration 3. Administer with a full glass of water 4. Advise patients to consume no more than 4000 mg of acetaminophen a day Nursing considerations for paracetamol 5. Advise patients not to drink alcohol while taking acetaminophen 6. Reduce dose of chronic alcoholics to take not more than 2000 mg of acetaminophen a day Nursing considerations for paracetamol 7. Advise patients with liver disease to ask their prescribers whether acetaminophen is safe 8. Monitor liver function tests, especially in patients with preexisting liver disease or those taking other medications that may affect liver function. 9. Educate the patient about the signs of liver toxicity, such as jaundice, dark urine, pale stools, and abdominal pain Salicylates • They are a class of compounds that contain the chemical salicylic acid • Aspirin (Acetylsalicylic acid) is one of the most well-known and widely used salicylate Aspirin Mechanism of action • inhibits the activity of an enzyme; cyclooxygenase (COX) • COX is of two types; COX-1 and COX-2 • Cox produces prostaglandin (mediators in the process of inflammation) and thromboxane (for blood clotting and constriction of blood vessels) • Aspirin therefore reduces the production of prostaglandins and thromboxane Aspirin Indications • Headache • Toothache • Neuralgias • Rheumatoid arthritis • Fever • To prevent coronary thrombosis and stroke in those at risk Aspirin Contraindications • Hypersensitivity or allergy • Peptic Ulcer Disease • Bleeding disorders such as hemophilia • Asthma • Pregnancy • Children under the age of 16 years (NB: because of Reye’s Syndrome) Aspirin Side effects / adverse effects • Gastrointestinal upset such as heartburn, indigestion, and stomach pain • Gastrointestinal bleeding • Bruising and easy bleeding • Allergic reactions such as skin rash, hives, swelling, difficulty breathing, or anaphylaxis • Asthma exacerbation • Tinnitus (ringing in the ears) Aspirin Nursing considerations 1. Take drug with or after food or with milk to decrease GI irritation 2. Assess for history of asthma and history of hypersensitivity 3. Do not use with other anticoagulants 4. Note any history of peptic ulcer 5. Report signs of side effect e.g. gastric irritation if occurs Aspirin Nursing considerations 6. Monitor the patient for signs of gastrointestinal bleeding 7. Assess for any signs of allergic reactions, such as rash, hives, swelling, or difficulty breathing 8. Aspirin is not given 1 week before & after surgery to prevent bleeding 9. Teaches patient about the toxic symptoms (ringing in the ears, dizziness, mental confusion) and ask him/her to report it to physician NON-STEROIDAL ANTI-INFLAMMATORY DRUGS (NSAIDs) Aspirin Diclofenac Ibuprofen Naproxen Celecoxib Mefenamic acid Piroxicam Meloxicam Indomethacin Diflunisal Etodolac Fenamates Meclofenamate sodium Fenoprofen Ketoprofen Methylsalicylate Nabumetone Oxaprazin Sulindac Tolmetin NSAIDs Indications • Mild to moderate pain, such as headache, dental pain, menstrual cramps, and musculoskeletal pain • Inflammation associated with conditions like arthritis, tendinitis • Fever NSAIDs Contraindications • Allergy or hypersensitivity • Peptic ulcer disease • History of gastrointestinal bleeding • Bleeding disorders like hemophilia • Severe kidney disease • Severe Liver Disease NSAIDs Side effects / adverse effects • Epigastric distress • Nausea • Vomiting • Gastrointestinal bleeding • Prolonged bleeding time • Respiratory depression • Tinnitus (ringing in the ears) • Hypersensitivity reactions such as urticaria, bronchoconstriction NSAIDs Nursing consideration 1. Perform a thorough assessment of the patient's medical history 2. Evaluate the patient's pain and inflammation levels 3. Monitor vital signs 4. Assess for gastrointestinal symptoms NSAIDs Nursing consideration 5. Educate the patient about the proper use of NSAIDs 6. Instruct the patient to take NSAIDs with food, milk, or a full glass of water to reduce the risk of gastrointestinal irritation 7. Advise patients to avoid alcohol while taking NSAIDs, as it can increase the risk of gastrointestinal bleeding 8. Discuss the importance of promptly reporting any adverse effects or changes in symptoms to the healthcare provider NSAIDs Nursing consideration 9. Monitor the patient's compliance with the medication regimen 10.Monitor for potential interactions with other medications the patient is taking 11.Monitoring liver and kidney function in patients on long-term NSAID therapy or those at risk of organ dysfunction