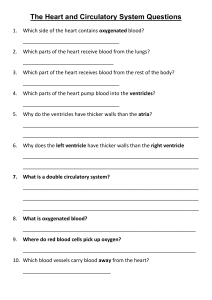
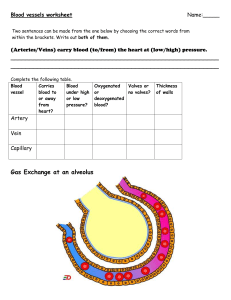
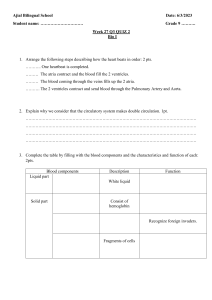
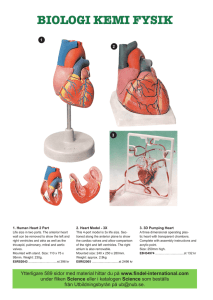
Chapter 8 Transport in mammals Circulatory system The system that contains the heart and the blood vessels and moves blood throughout the body. What happens when carbaminohaemoglobin, hydrogen carbonate ions reach The need for a circulatory system the lungs? The cells of all living organisms need a constant supply of reactants for When blood reaches the lungs, the reactions described above go into reverse. The carbon dioxide of carbaminohaemoglobin leaves the red blood cell. Hydrogen carbonate ions and hydrogen ions recombine to form carbonic acid which is later on breakdown to produce carbon dioxide and water molecules once more. This leaves the haemoglobin molecules free to combine with oxygen, ready to begin another circuit of the body. metabolism, e.g. oxygen and glucose. Single-celled organisms can gain oxygen and glucose directly from their surroundings, and the molecules can diffuse to all parts of the cell quickly due to short diffusion distances. Larger organisms, however, are made up of many layers of cells, meaning that the time taken for substances such as glucose and oxygen to diffuse to every cell in the body would be far too long. To solve this problem their exchange surfaces are connected to a mass transport system. For example, The digestive system is connected to the circulatory system, and the lungs are connected to the circulatory system. What happens when carbaminohaemoglobin, hydrogen carbonate ions reach the lungs? Mass transport is the bulk movement of gases or liquids in one direction, usually via a system of vessels and tubes. The circulatory system in mammals is a well-studied example of a mass transport system; the one-way flow of blood within the blood vessels carries essential nutrients and gases to all the cells of the body. Types of circulatory system Circulatory systems are either described as being open or closed. In a closed circulatory system, blood is pumped around the body and is always contained within a network of blood vessels. All vertebrates and many invertebrates have closed circulatory systems. In an open circulatory system, blood is not contained within blood vessels but is pumped directly into body cavities. Organisms such as arthropods and molluscs have open circulatory systems. Double circulation system Some carbon dioxide remains as carbon dioxide molecules and simply A mechanism in which blood passes through the heart 3. As dissolved carbon dioxide molecules in the blood plasma Humans have closed Double circulation system twice on one complete circuit of the body. It is called a double circulatory system because the blood flows dissolves in the blood plasma. About 5% of the total is carried in this form. from the heart to the lungs, then back to the heart, then around the rest of the body, and then back to the heart again. Double circulation has two parts. 2. As carbaminohaemoglobin Carbon dioxide that is not catalyzed by carbonic anhydrase inside RBC, combines 1. Systemic circulation: The part of the circulatory system that carries blood from the heart to all of the directly with the terminal amine groups (–NH2 ) of some of the haemoglobin body except the lungs, and then back to the heart. molecules. The compound formed is called carbaminohaemoglobin. In the lungs, Oxygen binding to hemoglobin reduces hemoglobin's affinity for carbon dioxide, causing the release of carbon dioxide from carbaminohaemoglobin. Blood is pumped out of the left ventricle into the aorta and travels from there to all parts of the body except the lungs. The carbon dioxide is then released into the alveoli and exhaled. About 10% of the carbon dioxide is carried in this way. It returns to the right side of the heart through the vena cava. 2. Pulmonary circulation: The part of the circulatory system that carries blood from the heart to the lungs and then back to the heart. The blood is pumped out of the right ventricle into the pulmonary arteries, which carry it to the lungs. The final part of the journey is along the pulmonary veins, which return it to the left side of the heart. Carbon dioxide transport The blood transports carbon dioxide in three different ways. 1. As hydrogen carbonate ions in the blood plasma Hydrogencarbonate ions are produced in the Bohr shift process which we already know. These are formed in the cytoplasm of the red blood cell because this is where the enzyme carbonic anhydrase is found. Most of the hydrogen carbonate ions then diffuse out of the red blood cell into the blood plasma, where they are carried in solution. About 85% of the carbon dioxide transported by the blood is carried in this way. Why chloride shift is important? If the chloride shift did not happen, the inside of the red blood cell would develop an overall positive charge, because hydrogen ions (from the dissociation of carbonic acid) would accumulate and would decrease blood pH. The pressure in the systemic circulation is considerably higher than in the pulmonary circulation. Single circulatory system A circulatory system in which the blood passes through the heart only once on a complete circuit. The chloride shift The chloride shift is the movement of chloride ions into red blood cells that occurs when hydrogen carbonate ions are formed . The hydrogen carbonate ions that are produced inside red blood cells, diffuse out of the cells and into the blood plasma. These ions have a negative charge and, to balance their movement, chloride ions (which also have a negative charge) move from the blood plasma into the red blood cells. This is called the chloride shift. Blood vessels Three main types of vessels make up the circulatory system. 1. Arteries: these are vessels with thick, strong walls that carry high-pressure oxygenated blood away from the heart. Small arteries are called arterioles. Large arteries are called aorta. Only exception is the pulmonary artery which carries deoxygenated blood from the heart to the lungs. Why haemoglobin/Bohr shift is important? Or How haemoglobin helps to 2. Veins: these are vessels with relatively thin walls that carry low-pressure maintain pH? deoxygenated blood back to the heart. Small veins are called venules. Large veins are called vena cava. Vena cava has two types: Superior vena cava: carries blood from the head, chest, and upper extremities. Inferior vena cava: it is the body's largest vein that carries blood from all parts Haemoglobin removes excess hydrogen ions from the solution. When carbon dioxide dissolves and dissociates, a high concentration of hydrogen ions is formed. This produces a low pH. If the hydrogen ions were left in the solution, the blood would be very acidic. By removing the hydrogen ions from the solution, haemoglobin helps to maintain the pH of the blood close to neutral. It is acting as a buffer. of the body below the diaphragm. Only exception is the pulmonary vein which carries oxygenated blood from the Biological buffers are organic substances that maintain a constant pH over a given range by neutralizing the effects of hydrogen ions. lungs to the heart. In the Lungs, Oxygen from the alveoli binds to hemoglobin, breaking down haemoglobinic acid and releasing hydrogen ions. 3. Capillaries: are tiny vessels that link arterioles and venules. It is the place where all the exchanges occur. Capillaries deliver nutrients, hormones, and other requirements to body The hydrogen ions combine with hydrogen carbonate ions to reform carbonic acid. cells, and take away their waste products. Capillaries form a network throughout every tissue in the body except the Carbonic acid then breaks down into water and carbon dioxide which is exhaled. brain, cornea, and cartilage. Reaction of carbonic anhydrase Carbon dioxide is continually produced by respiring cells. It diffuses from the cells and into the blood plasma, from where some of it diffuses into the red blood cells. In the cytoplasm of red blood cells, there is an enzyme, carbonic anhydrase which converts carbon dioxide and water into carbonic acid. Then carbonic acid breaks down into hydrogen ions and hydrogen carbonate ions. Hydrogen ions cannot diffuse out from the RBC but hydrogen carbonate ions can. Hydrogen ions readily combine with the haemoglobin, forming haemoglobinic acid, HHb. When haemoglobin does this, it releases the oxygen which it is carrying. Endothelium: a tissue that lines the inner surface of a structure such as a blood The Bohr shift vessel. Changes in the oxygen dissociation curve as a result of carbon dioxide levels Squamous epithelium: one or more layers of thin, flat cells forming the lining of are known as the Bohr effect or Bohr shift. some hollow structures, e.g. blood vessels and alveoli. The amount of oxygen haemoglobin carries is affected not only by the partial Smooth muscle: a type of involuntary muscle that can contract steadily over long pressure of oxygen but also by the partial pressure of carbon dioxide. periods of time. When the partial pressure of carbon dioxide in the blood is high, the saturation percentage of haemoglobin is reduced. Elastic arteries They are relatively large arteries, which have a lot of elastic tissue and little Haemoglobin has a low affinity for oxygen at low concentrations of oxygen. Low partial pressure (at respiring cells) of oxygen means, a low concentration of oxygen. muscle tissue in their walls. The elasticity of these artery walls is important in allowing them to stretch, which reduces the likelihood that they will burst. The artery walls stretch as the high-pressure blood surges into them and then recoil inwards as the pressure drops. 1. At low partial pressure of oxygen, haemoglobin binds less to the oxygen because of its less affinity, so the saturation percentage is low. 2. At medium pressure (at pulmonary veins and artery) of oxygen, haemoglobin binds more easily to oxygen because of its high affinity and saturation increases quickly. 3. At high pressure (at lungs) of oxygen, haemoglobin binds easily to oxygen because of its high affinity and saturation increases quickly. Muscular arteries Arteries that take blood from an elastic artery and deliver it close to its final destination have more smooth muscle in their walls which allows them to constrict and dilate. Vasoconstriction: the narrowing of a muscular artery or arteriole, caused by the contraction of the smooth muscle in its walls in response to The haemoglobin dissociation curve Partial pressure: is the pressure exerted by a single gas in a mixture of gases which helps to measure specific concentration of a gas. Saturation: a sample of haemoglobin that has combined with a maximum nerve impulses from the brain. amount of oxygen is said to be saturated. combined with oxygen, calculated as a percentage of the maximum amount the relaxation of the smooth muscle in its walls in response to nerve Percentage saturation: the degree to which the haemoglobin in the blood is Vasodilation: the widening of a muscular artery or arteriole, caused by with which it can combine. impulses from the brain. Dissociation curve: a graph showing the percentage saturation of a pigment (such as haemoglobin) with oxygen, plotted against the partial pressure of oxygen. Heart structure The human heart has a mass of around 300g and is roughly the size of a closed fist. Cardiac muscle: The muscle of the heart. Coronary arteries: arteries that branch from the aorta and spread over the walls of the heart, supplying the cardiac muscle with nutrients and oxygen. Heart structure The heart is a hollow, muscular organ located in the chest cavity. It is protected in the chest cavity by the pericardium, a tough and fibrous sac. The heart is divided into four chambers. The two top chambers are atria and the bottom two chambers are ventricles. The left and right sides of the heart are separated by a wall of muscular tissue, called the septum which is very important for ensuring blood doesn’t mix between the left and right sides of the heart. Haemoglobin Oxygen is transported around the body inside red blood cells in combination with the protein haemoglobin. Each haemoglobin molecule is made up of four polypeptides, each containing one haem group. Each haem group can combine with one oxygen molecule. Overall, then, each haemoglobin molecule can combine with four oxygen molecules (eight oxygen atoms). The portion of the septum that separates the left and right atria is called the interatrial septum, while the portion of the septum that separates the left and right ventricles is called the interventricular septum. Structural features of a WBC • White blood cells all have a nucleus, although the shape of this varies in different types of white cells. • Most white blood cells are larger than red blood cells, although one type, lymphocytes, may be slightly smaller. • White blood cells are either spherical or irregular in shape, not a biconcave disc. Valves Valves prevent the backward flow of blood. There are two types of valves. Lymphocytes Lymphocytes are smaller than phagocytes. They have a large nucleus that fills most of the cell. 1. B-lymphocytes and allow blood to flow from the atria into the ventricles but prevent it from going in the There are two types of lymphocytes, which are produced in the bone marrow. 1. Atrioventricular valves: The valves between the atria and the ventricles. They 2. T-lymphocytes opposite direction. Tricuspid valve: located between the right atrium and the right ventricle. Mitral valve (Bicuspid): located between the left atrium and the left ventricle. Monocytes/macrophages They are made in the bone marrow and circulate in the blood as monocytes. When there is any attack from bacteria or viruses, they eventually leave the blood. When they leave the blood they become macrophages. Monocytes and macrophages can live for several months. They play a crucial role in initiating immune responses, since they do not destroy pathogens completely, but cut them up to display antigens that can be recognized by lymphocytes. Semilunar valves: The valves in the entrances to the aorta and the pulmonary artery. These valves allow blood to flow from the ventricles into the arteries, but stop it going the other way. Pulmonary valve: located between the right ventricle and the pulmonary artery. Aortic valve: located between the left ventricle and the aorta. Neutrophils About 60-70% of the white blood cells in the blood are neutrophils. It can be recognized by its lobed nucleus and granular cytoplasm. They travel throughout the body, often leaving the blood by squeezing through the walls of capillaries to move through the tissues engulfing any pathogens that they find. During an infection, neutrophils are released in large numbers from their stores, but they are short-lived cells (5.4 days). Phagocytes Phagocytes are cells that protect the body by ingesting harmful foreign particles, bacteria, and dead or dying cells. Phagocytes are produced throughout life in the bone marrow. They are stored there before being distributed around the body in the blood. They are scavengers, removing any dead cells as well as invasive microorganisms. There are two types of phagocytes: 1. Neutrophils or 2. Monocytes/macrophages Why valves are important? Valves in the heart open when the pressure of blood behind them is greater than the pressure in front of them and close when the pressure of blood in front of them is greater than the pressure behind them. Valves are important for keeping blood flowing forward in the right direction and stopping it from flowing backward. They are also important for maintaining the correct pressure in the chambers of the heart. The Walls of the Heart The muscular walls of the atria are thinner than those of the ventricles. When the atria contract, the thin muscular walls do not generate much pressure, but White blood cells (Leukocytes) White blood cells, like red blood cells, are made in the bone marrow. enough to force blood down into the ventricles, through the atrioventricular valves. In contrast, the walls of the ventricles are thicker and more muscular. They can be divided into two main groups: 2. lymphocytes. inwards, increasing its pressure and pushing it out of the heart through the right and 1. phagocytes and Following the contraction of the atria, the ventricles contract and squeeze blood left semilunar valves. Left & right ventricle Some capillaries are even narrower than the diameter of a red blood cell but they can still pass through these vessels by squashing. This is possible because the cells have a specialized cytoskeleton which is made up of a mesh- The muscle of the left ventricle is significantly thicker than the right ventricle. This is because the blood leaving the right ventricle travels less distance than blood leaving the left ventricle. The blood pumped out from the right ventricle travels to the lungs, whereas blood like network of protein fibres. Red blood cells have no nucleus, no mitochondria, and no endoplasmic reticulum. The lack of these organelles means that there is more room for leaving the left ventricle has to travel to the rest of the body to deliver oxygen for respiration. To reach the rest of the body, the blood leaving the left ventricle must be under high pressure. haemoglobin, so maximising the amount of oxygen that can be carried by each This is generated by the contraction of the muscular walls of the left ventricle. red blood cell. The right ventricle generates less pressure from the contraction of its thinner walls, as blood only has to reach the lungs. Structural features of a red blood cell The cardiac cycle Red blood cells are shaped like a biconcave disc. The sequence of events that takes place during one heartbeat. Our heart beats Red blood cells are very small and have a size of about 7 μm. This small size means that no haemoglobin molecule within the cell is very far around 70 times a minute. from the cell surface membrane, and the haemoglobin molecules can therefore Diastole: is when the heart muscle relaxes. quickly exchange oxygen with the fluid outside the cell. Systole: is when the heart muscle contracts. Because of their size, they can easily squeeze through blood capillaries and bring oxygen as close as possible to cells that require it. Volume and pressure changes Contraction of the heart muscle causes a decrease in volume in the corresponding chamber of the heart, which then increases again when the muscle relaxes. Volume changes lead to corresponding pressure changes. 1. When volume decreases, pressure increases. 2. When volume increases, pressure decreases. Atrial systole The stage of the cardiac cycle is when the atria are filled with blood, and muscles in the walls of the atria contract. Red blood cells (Erythrocytes) The red colour of red blood cells is caused by the pigment haemoglobin, a globular protein. When the walls of the atria contract, atrial volume decreases and pressure increases. The pressure in the atria rises above that in the ventricles, forcing the atrioventricular (AV) valves open. Then, blood is forced into the ventricles. The main function of haemoglobin is to transport oxygen. Red blood cells do not live very long. Old ones are broken down in the liver, and new ones are constantly made in the bone marrow. They do not have nucleus. Ventricular systole The stage of the cardiac cycle is when the ventricles are filled with blood, and the muscles in the walls of the ventricles contract. When the walls of the ventricles contract, ventricular volume decreases and pressure increases. The pressure in the ventricles rises above that in the atria, forcing the AV valves to close, and preventing backflow. The pressure in the ventricles rises above that in the aorta and pulmonary artery. This forces the semilunar(SL) valves to open so blood is forced into the arteries and out of the heart. Diastole/ cardiac diastole The ventricles and atria are both relaxed. The pressure in the ventricles drops below that in the aorta and pulmonary artery, forcing the SL valves to close, and preventing backflow. The atria continue to fill with blood via the vena cava and pulmonary vein. The volume of fluid that leaves the capillary to form tissue fluid is the result of two opposing forces. 1. Hydrostatic pressure/ Water potential 2. Solute concentration Pressure in the atria rises above that in the ventricles, forcing the AV valves open. Blood flows passively into the ventricles without the need of atrial systole. Oedema: is a build-up of fluid in the body The cycle then begins again with atrial systole. Tissue fluid The almost colorless fluid that fills the spaces between body cells. It forms from the fluid (plasma) that leaks from blood capillaries. Tissue fluid is almost identical in composition to blood plasma. However, it contains far fewer protein molecules than blood plasma, because these are too large to escape easily through the capillary endothelium. Red blood cells are much too large to pass through, so tissue fluid does not contain these, but some white blood cells can squeeze through and move around freely in tissue fluid. Plasma: a pale yellow liquid blood component, in which the blood cells float. It carries a very large range of different substances in solution. Plasma proteins: a range of several different proteins dissolved in the blood plasma. Tissue fluid Control of heartbeat Blood comprises about 55% blood plasma and about 45% different types of Myogenic: a word used to describe muscle tissue that controls heartbeat without blood cells. Over 90% (95%) of blood plasma is water, while less than 10% consists of dissolved substances, mostly proteins. any external stimulus. Sinoatrial node (SAN) or pacemaker: a patch of cardiac muscle in the right atrium of the heart that contracts and relaxes in a rhythm, sets the pattern for the rest of the Over 99% of the solid particles in blood are red blood cells (erythrocytes). heart muscle. The rest are pale or colorless white blood cells (leukocytes) and platelets Atrioventricular node (AVN): a patch of tissue in the septum of the heart that (thrombocytes). transmits the wave of excitation from the walls of the atria and transmits it to the Purkyne tissue. Purkyne tissue: a network of Purkyne fibers that carry the cardiac impulse from the AVN to the ventricles of the heart and cause them to contract. SAN Atrium AVN Purkyne tissue Ventricle