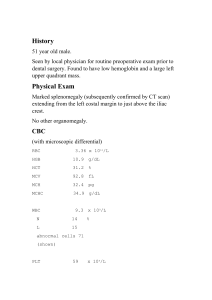
Sysmex xn 1000 flagging interpretation guide Sysmex flag interpretation. Sysmex xn-1000 user manual pdf. Sysmex xn 1000 dimensions. Sysmex flagging guide. Sysmex xn 1000 reference range. Sysmex xn 550 dimensions. Sysmex xn flagging interpretation guide. Sysmex flagging interpretation guide. Sysmex XE-Series Hematology Guide Document: MKT-40-1010 December 2008 By Sysmex America, Inc. This document is copyrighted and all rights reserved. No part of it may be reproduced or transmitted without permission. The information in this guide is subject to change and Sysmex is not liable for technical errors. The guide was created by Sysmex America, Inc. and can be contacted at One Nelson C. White Parkway, Mundelein, IL 60060. Abnormalities detected by XE-Series analyzers are categorized as NEGATIVE (no predefined abnormalities) or POSITIVE (indicating possible sample abnormality). The system generates Interpretive Program (IP) Messages, which can be verified by qualified personnel to resolve issues and obtain accurate results. The guide provides explanations of IP Message criteria, along with suggested actions for troubleshooting. It also emphasizes the importance of using established laboratory protocols in conjunction with the provided guidelines. Some key points from the guide include: * Abnormal Specimen Troubleshooting Guide * Objectives: provide explanation of XE-Series IP Messages and suggest actions to resolve sample related problems * Use of Quick Guide (laminated card) with this document * Classification of modern hematology analyzers as Automated Differential Cell Counters (ADCC) * Interpretive Program (IP) Messages indicating instrument findings The XE-Series Troubleshooting Guide is intended for users of the Sysmex analyzer. The guide provides information on interpreting results from blood cell count tests. The first section discusses abnormal results in white blood cell (WBC) scattergrams, specifically when clustering is abnormal or when WBC counts are below a certain threshold. In these cases, dashes may appear in place of data for certain populations, such as lymphocytes, monocytes, and neutrophils. Users are advised to perform a manual differential count if dashes appear. The guide also explains the interpretation of flags that appear on the analyzer's results. These flags indicate abnormal or unreliable results and require further investigation by the laboratory. For example, an asterisk (*) next to WBC data indicates that the result is unreliable due to the presence of nucleated red blood cells (NRBCs). The second section provides information on flagging interpretation for specific IP messages, including Abnormal NRBC Scattergram and NRBC Abn Scattergram. These messages are generated when NRBCs are detected in the sample. The guide advises users to scan the peripheral smear for abnormal morphology if flags appear. Overall, the XE-Series Troubleshooting Guide provides guidance on interpreting results from blood cell count tests, including how to identify abnormal or unreliable results and what actions to take next. The report provides guidance on interpreting results from the XE-Series blood analyzer. If lymphoblasts or very small lymphocytes are present, review the smear and check for platelet clumps or abnormalities. If NRBCs (newly released red blood cells) are not seen in the smear, review the WBC count and differential (Differential Staining Test) to determine if abnormal white blood cells are present. If so, perform a manual differential according to your laboratory's policy. If NRBCs are present, perform a manual differential according to your laboratory's policy, and convert the manual NRBC count to percentage. Correct the WBC count for the presence of NRBCs counted by using a specific formula. The report also includes guidance on interpreting abnormal results, such as the "Blast? IP" message, which indicates abnormal clustering in the region for blasts in the white blood cell count. This may indicate leukemia or other blood disorders. The report provides suggested action steps for addressing these abnormalities and performing manual differentials according to your laboratory's policy. In general, the report advises: 1. Reviewing the peripheral smear carefully for abnormal cells, such as blasts, immature granulocytes, atypical lymphocytes, and other abnormal cells. 2. Performing a manual differential if abnormal cells are noted or data is missing, following individual laboratory criteria. 3. Reporting results according to your laboratory's policy. If no abnormalities are found, the data with an asterisk (*) can be reported as normal. The XE-Series Results software can generate quantitative results for immature granulocytes (IG) and left shift WBCs, as well as other white blood cell components. The IG Present flag is triggered when the percentage or number of IG exceeds a user-defined value. If abnormal clustering is detected in the scattergrams, an asterisk (*) appears next to the neutrophil, eosinophil, and basophil percentages and numbers. This indicates that the results are unreliable if abnormalities are found during laboratory review. In cases where the IG Present flag is triggered, the suggested action steps are: 1. Examine the peripheral smear for immature granulocytes, band cells, toxic granulation, or other abnormal cells. 2. If abnormal cells are detected, perform a manual differential count and report according to laboratory criteria. 3. If no abnormalities are found, the data with the asterisk (*) can be reported. Additionally, if the Left Shift? IP flag is triggered, it indicates that the instrument has detected abnormal clustering in the region for left shift WBCs (bands) in the scattergrams. The suggested action steps for this scenario are: 1. Examine the peripheral smear for abnormalities. 2. If no abnormalities are found, the data with the asterisk (*) can be reported. Note: The text appears to be a guide for interpreting results from an XE-Series analyzer, specifically flags related to immature granulocytes and left shift WBCs. **Interpretation of Abnormal WBC Results** The presence of abnormal cells in a blood sample can indicate various conditions. The following steps should be taken when such cells are detected: 1. **Scan the Peripheral Smear**: Check for atypical or variant lymphocytes, immature lymphs (such as seen in ALL or CLL), and other abnormal cells. 2. **Manual Differential**: If abnormal cells are noted, perform a manual differential to determine their type and percentage. 3. **Report Results**: Report the results according to individual laboratory criteria. **Abnormal Cell Indicators** - **Atypical Lympho?**: Indicates significant clustering in the region for atypical lymphocytes on the DIFF scattergram. - **Suspect, Atypical Lympho?**: Suggests that the instrument has detected abnormal lymphocytes. **Suspect, Abn Lympho/L_Blasts?**: Indicates the presence of abnormal lymphocytes or lymphoblasts. **Interpretation Guide** * When an asterisk (*) appears next to the Neutrophil, Lymphocyte, and Monocyte percentages, these results are unreliable if abnormalities are found. * Abnormal lymphocytes or lymphoblasts detected by the instrument may indicate conditions such as leukemia or lymphoma. **WBC IP Messages** The XE-Series Flagging Interpretation Guide provides instructions for interpreting certain messages related to white blood cell counts. **Suspect Abnormal Lymphocytes or Blast Cells?** If atypical or variant lymphocytes or lymphoblasts are present on a peripheral smear, follow these steps: 1. Scan the smear to identify any abnormalities. 2. If atypical lymphocytes exceed the normal reference range, report their presence and estimate the percentage. 3. Perform a manual differential if necessary. 4. Report any other abnormal morphological findings. **Suspect NRBC?** The NRBC IP message is generated when the XESeries analyzes the sample in CBC + DIFF + NRBC mode and detects clustering between lymphocytes and red blood cell ghosts on the DIFF scattergram. If abnormalities are found during review of the sample, an asterisk (*) appears next to the WBC count. **WBC Count Interpretation** The WBC count is corrected if NRBCs exceed a programmed limit (0.01/100 WBC). An "and" (&) symbol is used to indicate this correction. These messages are part of the XE-Series Flagging Interpretation Guide, Section 2: WBC IP Messages, Document Number MKT-40-1010, December 2008. 1. If NRBCs are present, reanalyze the sample in CBC + DIFF + NRBC mode. This will provide a quantitative NRBC % and #, as well as automatically corrected WBC and Lymph counts. Report this data if other IP messages are absent. 2. Review morphology with presence of NRBCs: - Check the smear for abnormal cell morphology (abnormal RBC and NRBCs). - Comment on abnormal morphology per laboratory criteria. 3. For suspect, RBC Lyse Resistance? messages: - If WBC/BASO scattergrams show abnormal clustering near RBC ghost populations, this message is seen. - An asterisk (*) appears next to the WBC and HGB results, indicating these are unreliable if abnormalities are found during laboratory review of the sample. 4. Suggested action steps: - Scan the peripheral smear: - Look for abnormal RBC morphology - Perform a slide estimate of the WBC count - Perform a manual differential according to your laboratory's policy - Report results verified by slide review and individual laboratory guidelines. - If WBC results are not verified, prepare a dilution using CELLPACK as the diluent: - Reanalyze the diluted sample to verify WBC results. - Observe for clinically significant change in counts. - Report verified results according to individual laboratory guidelines. Abnormal, RBC Abn Distribution IP Message **Document Number:** MKT-40-1010 December 2008 **Page:** 1 of 2 When the histogram pattern from the RBC channel is abnormal or agglutinin reacts with RBC < 0.5 x 10^6/µL, the RBC Abn Distribution IP Message is generated. If an abnormal reticulocyte scattergram is present, follow the suggested guidelines for the HGB/Turbidity Interference and RDW-SD. Note that if the RBC morphology is abnormal, the 'rules of 3' may not always hold true. The RET Abn Scattergram IP Message indicates increased activity in the reticulocyte parameters on the XE-Series instrument. This message appears when the instrument detects increased activity in the threshold area or upper particle plateau area on the scattergram. Asterisks (*) appear next to the RET%, PLT, and IRF parameters if these results are unreliable due to abnormalities found during laboratory review of the sample. To troubleshoot this issue, prepare a 1:5 dilution with CELLPACKTM diluent to minimize interference. Run the diluted sample in manual mode (not capillary mode). If the flag is eliminated, multiply the absolute count by 5 and report. However, do not apply the same dilution factor to RBC counts, as these should remain unchanged. Decisions on reporting with a comment or performing an alternative method should be based on laboratory practices. If the flag persists, rule out analyzer functional errors by reanalyzing the patient sample and running a known normal patient sample to ensure there are no dilutional errors. If the RBC count is not adequate or if there are issues with the diluted sample, take the following steps to resolve the problem: 1. Check the peripheral smear for signs of polychromasia, NRBCs, Howell-Jolly Bodies, or basophilic stippling. If these abnormalities are present, note that they may affect the test results. 2. Alternatively, perform the reticulocyte analysis using an alternative method. If you suspect RBC agglutination (clumping), follow these steps: 1. Scan the peripheral smear for signs of agglutinated RBCs. 2. Warm the sample to 37°C for 15-30 minutes and then reanalyze it in manual mode after mixing it by inversion 10 times. Performing these steps can help resolve issues with RBC count or agglutination and provide accurate test results. Looking for a plasma replacement if cold agglutination is present, warming the sample may not work in some cases; using room temperature CELLPACK can be an option. Testing procedures are needed to confirm the presence of a cold agglutinin or warm-reacting antibody. Additional tests may be required based on laboratory policy. Suspect turbidity and HGB interference if MCHC is > 36.5 g/dL, as this could interfere with HGB detection; dilute specimen and reanalyze MCH and MCHC parameters. If RBC morphology is abnormal, the usual rules for calculating HGB levels don't apply. The plasma and cellular HGB should be measured separately in such cases. For samples with high WBC counts and suspected turbidity interference, make a diluted sample using CELLPACKTM as the diluent. If the HGB results change after dilution, report the new HGB values and recalculate MCH and MCHC accordingly. Also, if the WBC count exceeds the laboratory's established linearity limit, report the corrected WBC value from the diluted sample. Other possible causes of falsely increased or decreased HGB levels include abnormal plasma proteins, severe hyponatremia, and cold agglutinins. In such cases, consider performing a plasma replacement procedure, diluting the sample after allowing it to stand for 10 minutes, or pre-warming the specimen according to lab protocol. When encountering an Iron Deficiency? IP Message on the XE-Series system, check the peripheral smear for microcytic and hypochromic RBCs. Report any clinically significant RBC morphological abnormalities found. If extremely microcytic RBCs are present, estimate the PLT count. Consider suggesting confirmatory testing for iron deficiency anemia according to laboratory policy. In cases where the "rules of 3" don't hold true due to abnormal RBC morphology, recalculate indices using the cellular HGB value. For samples with high WBC counts and suspected turbidity interference, make a diluted sample and report corrected values accordingly. Other possible causes of falsely increased or decreased HGB levels include abnormal plasma proteins, severe hyponatremia, and cold agglutinins. The HGB Defect? IP Message suggests that the suspect has an abnormality in their red blood cells (RBCs) or platelets. To determine this, follow these steps: 1. Examine the peripheral smear for any irregularities in RBC morphology, such as microcytosis (small size), hypochromia (lack of hemoglobin), target cells, sickle cells, or HGB C crystals. 2. Report any clinically significant abnormalities according to individual laboratory policy. If extremely microcytic RBCs are present: 1. Estimate the platelet count. 2. If the RET (red cell estimation) was not ordered, the XE-Series 2100 may generate an Action Message stating "Count RET". The operator can reanalyze the specimen in CBC + MCV mode to determine whether to switch to report the PLT-O. 3. Suggest confirmatory testing for hemoglobinopathies if indicated by the RDW-CV (red cell distribution width-corrected). Additionally, the text discusses an IP Message related to fragmented RBCs: To investigate this issue: 1. Examine the peripheral smear for the presence of fragmented RBCs and other forms of poikilocytosis. 2. Report any clinically significant abnormalities according to individual laboratory policy. If extremely microcytic RBCs are present, follow the same steps as above. Count RET Channel. The operator can reanalyze the specimen in CBC + RET mode. The XE judges whether or not to switch to report PLT-O. If RBC morphology is abnormal, the "rules of 3" do not always hold true. #### Abnormal PLT Abn Distribution The PLT Abn Distribution IP Message XE-Series Resultsis generated by calculation and size comparison of certain PLT items (PDW, RBC 2.95 [106/µL]PL%* [% of PLT lower discriminator],PU%* [% of upper discriminator], PMFV, HGB 8.0 [g/dL]PLT, PLCR* [platelet large cell rates], HCT 28.2 [%]MPV, PU* [platelet upper discriminator]). MCV 95.6 [fL] MCH 27.1 [pg]* These are all non-reportable parameters that MCHC 28.4 g/dL] PLT & 191 * [103/µL] are used as part of this flagging algorithm. RDW-SD 98.4 [fL] RDW-CV 29.6 [%] Dashes may appear in place of data for MPV —— [fL] the MPV or the MPV is marked with an RET % 3.62 [%] asterisk (*). The asterisk (*) indicates these results are unreliable if RET # 0.1068 [ratio] abnormalities are found during the IRF 0.353 laboratory’s review of the sample. #### Suggested Action Steps 1. For laboratories with the XE-2100L or XE-2100D, proceed to Step 2. 1. For laboratories with the XE-2100, re-analyze the sample ordering a CBC and RET. By ordering the CBC and RET, an optical platelet (PLT-O) is performed using fluorescent flow cytometry. 2. Scan the peripheral smear for the presence of abnormal PLT morphology: large or giant platelets, small platelets, platelet clumps, fragmented RBCs, microcytic RBCs 3. Perform a manual platelet estimate to ensure the count is accurate. If platelet estimate confirms accuracy of count, it may be reported. 4. Report any clinically significant RBC and/or PLT morphology according to individual laboratory guidelines. **Troubleshooting Guide for PLT IP Messages** When the XE-2100 analyzer detects abnormal platelet (PLT) scattergrams, it generates an "Abnormal, PLT Abn Scattergram" message. This occurs when there is clustering in the PLT-O area on the RETIC and RET-EXT scattergrams. The analyzer will not report a PLT count if abnormalities are found. **Symptoms of Unreliable Results** The asterisk (*) symbol next to certain results (PLT-I, MPV, etc.) indicates that they may be unreliable due to sample abnormalities. **Suggested Action Steps** 1. Examine the peripheral smear for abnormal platelet or red blood cell morphology. 2. Perform a manual platelet estimate to ensure accuracy. 3. Report any clinically significant white blood cell, red blood cell, and/or platelet morphology. Additionally, if the analyzer detects clustering in the upper right ghost regions of scattergrams, it will generate a "PLT Clumps?" message, indicating unreliable results for certain values. **Action Steps for PLT Clumps? Message** 1. Examine the peripheral smear for abnormal platelet or red blood cell morphology. 2. Perform an alternate procedure to ensure accurate platelet count if clumps are present. By following these troubleshooting steps, you can resolve issues with unreliable results and ensure accurate laboratory testing. !!! Fibrin strands or platelet clumps? Examine the feathered edge carefully. If present, verify white blood cell (WBC) and platelet (PLT) counts using a manual slide estimate. If the estimate doesn't match the instrument count, proceed to the next step for an accurate count. 1. When analyzing the citrate tube results, focus only on the WBC and PLT counts. To adjust for Na Citrate dilution, multiply these values by 1.1. 2. If recollection is not feasible, estimate platelet count levels (low, normal, or high) and note if "platelet clumps present" due to inability to report an accurate count. 3. For samples without abnormalities, data with asterisks (*) can be reported. This article references various resources related to hematology and blood analysis. It includes publications from the late 1980s and early 1990s, such as "Clinical Hematology and Fundamentals of Hemostasis" by Denise M. Harmening and "Diagnostic Hematology" by Bernadette Rodak. Additionally, it cites an article titled "Lipemia and Hemoglobin Determinations" published in the Medical Laboratory Observer journal. The text also mentions a medical textbook called "Hematology: Basic Principles and Practice." Furthermore, it provides information on the Sysmex XE-2100 automated blood analyzer, including operator's manuals and troubleshooting guides from 2004 and 2008, respectively.