Urinary System Assessment: Structure, Function, Diagnostics
advertisement

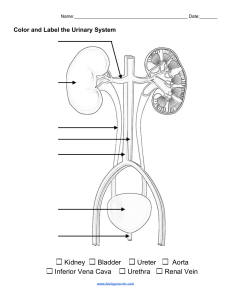
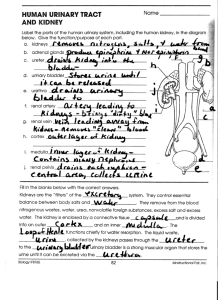
Chapter 49 Assessment: Urinary System KEY POINTS STRUCTURES AND FUNCTIONS OF URINARY SYSTEM • The urinary system is divided into the upper system, consisting of 2 kidneys and 2 ureters, and the lower system, consisting of a urinary bladder and urethra. Kidneys • The primary functions of the kidneys are to (1) regulate the volume and composition of extracellular fluid (ECF) and (2) excrete waste products from the body. • The outer layer of the kidney is termed the cortex, and the inner layer, which is made of coneshaped projections, is called the medulla. • The nephron is the functional unit of the kidney. Each kidney has 800,000 to 1.2 million nephrons. • A nephron is composed of a glomerulus, Bowman’s capsule, and tubular system. The tubular system consists of the proximal convoluted tubule, loop of Henle, distal convoluted tubule, and a collecting tubule. • Urine formation is the result of a multistep process of filtration, reabsorption, secretion, and excretion of water, electrolytes, and metabolic waste products. Glomerular Function • Blood is filtered in the glomerulus. • The hydrostatic pressure of the blood within the glomerular capillaries causes a portion of blood to be filtered across the semipermeable membrane into Bowman’s capsule. 1 Copyright © 2023 by Elsevier, Inc. All rights reserved. • The glomerular filtrate is similar in composition to blood, except that it lacks blood cells, platelets, and large plasma proteins. • The amount of blood filtered by the glomeruli in a period is termed the glomerular filtration rate (GFR). The normal GFR is about 125 mL/min. Tubular Function • The functions of the tubules and collecting ducts include reabsorption and secretion. • Reabsorption is the passage of a substance from the lumen of the tubules through the tubule cells and into the capillaries. Tubular secretion is the passage of a substance from the capillaries through the tubular cells into the lumen of the tubule. • The loop of Henle is important in conserving water and concentrating the filtrate through reabsorption. • Two important functions of the distal convoluted tubules are final regulation of water balance and acid-base balance. • Antidiuretic hormone (ADH) is needed for water reabsorption. • Aldosterone acts on the distal tubule to cause reabsorption of sodium (Na+) and water. In exchange for Na+, potassium ions (K+) are excreted. • Acid-base regulation involves reabsorbing and conserving most of the bicarbonate (HCO3−) and secreting excess H+. • Atrial natriuretic peptide (ANP) acts on the kidneys to increase sodium excretion. • Parathyroid hormone (PTH) acts on renal tubules to increase reabsorption of calcium. It maintains the appropriate level of calcium in the blood. Other Functions of the Kidney 2 Copyright © 2023 by Elsevier, Inc. All rights reserved. • The kidneys make erythropoietin in response to hypoxia and decreased renal blood flow. Erythropoietin stimulates red blood cell (RBC) production in the bone marrow. • Vitamin D is activated in kidneys. Vitamin D is important for calcium balance and bone health. • Renin, which is made and secreted by juxtaglomerular cells, is important in BP regulation. • Prostaglandin (PG) synthesis, primarily PGE2 and PGI2, occurs in kidneys, mostly in the medulla. These PGs have a vasodilating action, thus increasing renal blood flow and promoting Na+ excretion. Ureters • The ureters are tubes that carry urine from the renal pelvis to the bladder. • Circular and longitudinal smooth muscle fibers, arranged in a meshlike outer layer, contract to promote the peristaltic one-way flow of urine. Bladder • The urinary bladder is a stretchable organ located behind the symphysis pubis and anterior to the vagina and rectum. It stretches with filling without its pressure increasing. • Its primary functions are to serve as a reservoir for urine and to help the body eliminate waste products. • On the average, 200 to 250 mL of urine in the bladder causes moderate distention and the urge to urinate. Urethra • The urethra is a small tube that incorporates the smooth muscle of the bladder neck and extends to the striated muscle of the external meatus. 3 Copyright © 2023 by Elsevier, Inc. All rights reserved. • The primary function of the urethra is to serve as a conduit for urine from the bladder neck to outside the body during voiding and to control voiding. • The female urethra is significantly shorter than the male urethra. Urethrovesical Unit • Together, the bladder, urethra, and pelvic floor muscles form the urethrovesical unit. It receives neuronal input from the autonomic nervous system. • Normal voluntary control of this unit is defined as continence. • Any disease or trauma that affects function of the brain, spinal cord, or nerves that directly innervate the bladder, bladder neck, external sphincter, or pelvic floor can affect bladder function. GERONTOLOGIC CONSIDERATIONS: EFFECTS OF AGING ON URINARY SYSTEM • Healthy adults experience a 10% decline in glomerular function every decade starting at age 40 • Atherosclerosis has been found to accelerate the decrease of renal size with age. • Older adults maintain body fluid homeostasis unless they encounter diseases or other physiologic stressors. ASSESSMENT OF URINARY SYSTEM • A health history for the urinary system consists of assessment of past health history; medications; surgeries, particularly pelvic surgeries or urinary tract instrumentation; any previous hospitalizations related to renal or urologic diseases and all urinary problems during past pregnancies; and a review of systems using functional health patterns. 4 Copyright © 2023 by Elsevier, Inc. All rights reserved. • The physical examination for urologic disorders includes height and weight, an inspection of the skin (integrity, color, and peripheral edema), and examination of the abdomen and costovertebral area. DIAGNOSTIC STUDIES OF URINARY SYSTEM • Radiologic studies (kidney-ureter-bladder x-rays, computed tomography, magnetic resonance imaging, and renal angiography), ultrasonography, and biopsy are used to diagnose problems of the urinary system. • Blood tests, including BUN, creatinine, electrolytes, and fasting glucose, may be helpful. • Urine studies • A urinalysis may provide information about possible abnormalities, indicate what further studies need to be done, and supply information on the progression of a diagnosed disorder. • Because almost all creatinine in the blood is normally excreted by the kidneys, creatinine clearance is the most accurate indicator of renal function. The result of a creatinine clearance test closely approximates that of the GFR. • Urodynamic studies are used to assess the function of the bladder. 5 Copyright © 2023 by Elsevier, Inc. All rights reserved.