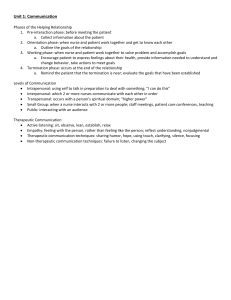
COMMUNICATION AND THERAPEUTIC USE OF SELF Communication-refers to the transmission of feelings, attitudes, ideas and behavior from one person to another. THERAPEUTIC COMMUNICATION -refers to a healing or curative dialogue between people. This is particularly significant to the nurse because it is the basis of therapeutic relationships. -it involves an exchange of information between clients and nurses. -is “other focused” communication, it is about listening rather than talking. -the foundation of therapeutic communication is rapport. Rapport-refers to harmony or accord between people. -it is vital for the formation of trust. PURPOSE OF COMMUNICATION 1. To initiate conversation 2. To establish rapport and build trust 3. To give and gather information 4. To persuade or to convince a viewpoint GOALS OF THERAPEUTIC COMMUNICATION 1. Encourage self-disclosure 2. Increase feelings of self-worth 3. Promote increased understanding (insight) 4. Encourage problem solving 5. Facilitate decision-making ELEMENTS OF THERAPEUTIC COMMUNICATION 1. Trust- is a critical element which you may have to establish or just maintain. 2. Empathy- is the ability to put oneself in other’s place and see things from his/her perspective. You do this by really listening to what he/she is expressing and then acknowledge it. 3. Respect- is conveyed verbally and non-verbally. It includes both respecting the other for who he/she is and what he/she is. 4. Congruence- involves genuineness or authenticity. In other words, you come across as being sincere and meaning what you say. You aren’t trying to be someone you’re not or convey something you don’t mean. 5. Self-awareness- is being aware of how your thoughts, feelings and behavior can help to convey other elements like congruence, respect and empathy. Person with self-awareness can comfortably move the focus away from self and onto the other. 6. Listening- NURSE-PATIENT INTERACTION (NPI)-any nurse-patient contact during which the nurse and the patient have reciprocal influence to each other, communicating verbally and non-verbally. It refers to communication. OBJECTIVES OF THE NURSE-PATIENT RELATIONSHIP 1. 2. 3. 4. 5. 6. Listening-perceiving the patient’s message in the cognitive level and effective domains. Warmth- feeling of cordiality and inaction. Genuineness- being one’s self and not acting out a role, being open and truthful Attentiveness- demonstrating a concentration of time or attention to the nurse Empathy- understanding the patient’s feeling and viewing the world as the patient does. Positive regard- accepting patient as he is. FACTS TO REMEMBER: 1. It’s not friendship 2. Its main benefit is to the patient 3. It’s an opportunity for the patient to deal with his problem that brought him to treatment 4. The nurse approach to the relationship is crucial to the client’s being able to express his feelings PHASES OF NURSE-PATIENT (HELPING) RELATIONSHIP 1. Pre-interaction Phase- before meeting the client, the nurse review available data including the medical and nursing history. Talks to other care givers who may have information about the client. Anticipate health concerns or issues that may arise. Identifies a location and setting that will foster comfortable, private interaction. Plan enough time for initial interaction. 2. Orientation Phase- when the nurse and client meet and get to know one another, the nurse: a. Sets the tone for the relationship by adopting the warm, emphatic, caring manner. b. Recognizes that initial relationship maybe superficial, uncertain, and tentative. 1 c. Expect the client to test the nurse’s competence and commitment d. Closely observe the client and expects to be closely observed by the client e. Begin to make inferences and form judgment about client messages and behaviors. f. Assess the client’s health status g. Priorities the client’s problems and identifies the client’s goal h. Clarifies the client’s and nurse’s roles i. Form contracts with the client that specify who will do that j. Let the client know when to expect the relationship to be terminated. 3. Working Phase- when the nurse and client work together to solve problems and accomplish goals, the nurse: a. Encourage and helps the client with self-exploration b. Provides information needed to understand and change behavior c. Encourage and helps the client to set with the client. d. Takes action to meet the goals set with the client e. Use appropriate self-disclosure and confrontation 4. Termination Phase- during the ending of the relationship, the nurse: a. Reminds the client that termination is near b. Evaluates goal achievement with the client c. Reminisces about the client relinquishing responsibility for his or her care d. Achieves a smooth transition for the client to other caregivers as needed e. Nurse and client express thoughts and feelings about termination. f. Observe client- high level of anxiety during this phase, exhibit the following: 1. Hostility 2. Disparagement of relationship 3. Hallucinations, delusions 4. Regressive behaviors 5. Recall of other separation experience TECHNIQUES OF COMMUNICATION 1. To initiate conversation a. Giving broad opening-is using a general statement or question to encourage the client to set the direction for the session. It means giving the patient an opportunity to set direction of the conversation Example: The client enters the room, takes a seat and looks expectantly at the nurse. The nurse may say... a. “Is there anything that you want to talk about?” b. “How are you today?” b. Giving recognition- it means focusing on the positive aspects of the patient’s personality. Example: Nurse: “I noticed that you took a bath today” Nurse: “I’m glad you’re participating with our activity” 2. To establish rapport and build trust 1.Giving information-responding with the needed facts Example: Client: “Can I go home now?” Nurse: “Yes you can go home but not now because you’re still undergoing treatment” 2.Use of silence3.Self-disclosure-sharing personal information or an opportune moment to convey understanding Example: Client: “My son death was like losing major part of your life.” Nurse: “I have a similar feeling when my daughter dies” 4.Empathy-experiencing another feeling temporarily Example: Client: “This whole thing is a mistakes. I shouldn’t even be here.” Nurse: “It’s sounds like it is difficult for you to be here.” 5.Genuineness- giving honest feedback when the client is ready; it means acting incongruent manner with the client Example: Client: “You looked bored Nurse: “I’m not bored but I do feel very tired” Client: “Do you think I’m weird” 2 Nurse: “Sometimes” 6.Respect-conveying openness, a nonjudgmental attitude, and a desire to hear what the client has to say. 3. To gather information 1.Focusing- assisting a patient explore a specific topic Example: Client: “I can’t decide about my…..” Nurse: “Let’s talk about that. Perhaps if we talk about it, it will help you decide” 2.Restating-repeating what the patient has said to indicate that the nurse is listening and interested. This may encourage the client to elaborate. Example: Client: “I don’t belong here” Nurse: “You don’t belong here” 3.Validating-confirming one’s observation Example: “Are you saying that……” 4.Reflecting-paraphrasing what the client has said Example: Client: “The cop was out to get me. He has no reason to pull me over. It was a real set-up.” Nurse: “You believe it was unfair for the police to pull you over.” 5.Confrontation- acknowledging discrepancies in the client’s verbal and non-verbal behavior. Example: Client: “I don’t have problem with alcohol.” Nurse: “You said that alcohol hasn’t created any problem for you, yet you have had 3 bottles before this session and your wife nags you about your drinking.” 3 THERAPEUTIC AND NON-THERAPEUTIC COMMUNICATION Quick Checklist for Effective Communication: Open ended questions Focus on feelings State behaviors observed Reflect, restate, rephrase verbalizations of patient Natural responses Effective Communication: Appropriate Simple Adaptive Concise Credible TECHNIQUE Offering self: Making self-available and showing interest and concern Active listening: Paying close attention to what the patient is saying by observing both verbal and nonverbal cues. (Just to be there to listen) Exploring: Delaying further into the subject or area Giving broad openings: Allowing the client to take the initiative to introduce a topic Silence : Planned absence of verbal remarks to allow patient and nurse to think over what is being discussed any say more. Stating the observed/ Making observation: Verbalizing what is observed in the patient to for validation and to encourage discussion. Encouraging comparisons: Asking to describe similarities and differences among feelings, behaviors and events. Identifying themes: Asking to identify recurring thoughts, feelings and behaviors. Summarizing: Recapping what has been talked about. Reviewing the main points of discussions and making appropriate conclusions. Placing the event in time and sequence: Asking for relationship among events. Voicing doubt: Voicing uncertainty about the reality of patient’s statements, perceptions and conclusions. Encouraging description of perceptions: Asking for patient’s to describe feelings, perceptions and views of their situations. Presenting reality or confronting: Stating what is real and what is not without arguing with the patient. EXAMPLE I will walk with you to the dayroom. Maintaining eye contact and making verbal remarks to clarify and encourage further communication. Tell me more about your son. What do you want to talk about today? You sound angry. Can you tell me what makes you more comfortable, working by yourself or working as a member of a team? When do you always feel the need to check the doors and windows? During this meeting, we discussed about what you will do when you feel the urge to hurt yourself again and this include… When did you begin to experience these ticks, before or after you entered grade school? I find it hard to believe… What are these voices telling you to do? I know you hear these voices but I do not hear them. I am __ , your nurse, and this is a hospital not a beach resort. Seeking clarification: Asking patients to elaborate, I am not familiar with your line of work; can you or give examples of ideas or feelings to seek describe it further for me. clarification of what is unclear. I don’t think I understand what you are saying. Verbalizing the implied: Rephrasing patient’s words Patient: I won’t be bothering you anymore soon. to highlights an underlying message and to clarify Nurse: Are you thinking of killing yourself? statements. Restating: Repeating the exact words of patients to Patient: I can’t sleep; I stay awake all night. remind them of what they said and to let them know Nurse: You can’t sleep at night. they are heard. 4 Reflecting: Throwing back the patient’s statement in a form of question helps the patient identify feelings. General leads: Giving encouragement to continue. Using neutral expression to encourage patients to continue talking. Asking questioning: Using open-ended questions to achieve relevance and depth in discussion. Empathy: Recognizing and acknowledging patient’s feelings. Focusing: Concentrating on a single point. Patient: I think I should leave now. Nurse: Do you think you should? Go on. You were saying… How did you feel when the doctor told you that you are ready for discharge soon? It’s hard to begin to live alone when you have been married for more than thirty years. Let us talk about your best friend in high school. You were saying…. Interpreting: Providing a view of the meaning or Patient: I always take this bag wherever I go. importance of something. Nurse: That bag must always be with you. Encouraging evaluation: Asking for patient’s views What do you think led the count to commit you here? of the meaning or importance of something. Can you tell me. Suggesting collaboration: Offering to help patients Perhaps you can discuss this with your children so solve problems. they will know how you feel and what you want. Accepting: Indicates that you are being receptive. Yes, I know. I follow what you said. Simply nodding. Encouraging goal setting: Asking patients decide on What do you think are the things you have to change the type of change needed. in yourself? If you decide to leave home when your husband beat Encouraging formulation of a plan of action: Probing for step by step actions that will be needed. you again what will you do next? Encouraging consideration of options: Asking Have you thought of the possible effects of your patients to consider the pros and cons of possible decisions to you and your family? options. Giving information: Providing information that will Nobody deserves to be eaten and there are people help patients make better choices. who can help and places to go when you do not feel safe at home anymore. Limit setting: Discouraging non- productive feelings Please stop now. If you don’t, I will have to ask you and behaviors and encouraging productive ones. to leave the group and go to your room. Good morning, Ana. Giving recognition Supportive confrontation: Acknowledging the I understand your feeling rejected when your difficulty in changing, but pushing for action. children sent you here but if we look at it this way… Role playing: Practicing behaviors for specific I’ll play your mother, tell me exactly what you would situations, both the nurse and patient play particular say when we meet on Sunday. role. Rehearsing: Asking the patient for a verbal Supposing you meet these people again, how would description of what will be said or done in a you respond to them when they ask you join them for particular situation. a drink? Feedback: Pointing out specific behaviors and I see you combed your hair today. giving impressions of reactions. Encouraging evaluation: Asking patients to What did you feel after participating in the group evaluate their actions and the outcomes. therapy? Reinforcement: Giving feedback on positive Everyone was able to give their opinions when we behaviors. talked one by one and each of us wanted patiently for our turn to speak. BLOCKS OR BARRIERS TO COMMUNICATION Avoid these pitfalls: Giving advise Talking about self Telling client is wrong Entering into hallucinations and delusions of client False reassurance Cliché (a saying or expression that has been so overused that it has become boring and unoriginal Giving approval Asking WHY? 5 Changing subject Defending doctors and other health team members NON-THERAPEUTIC TECHNIQUE Overloading: Talking rapidly, changing subjects too often, and asking for more information than can be absorbed at one time. Value judgments: Giving one’s own opinion, evaluating, moralizing or implying one’s values by using words such as “nice”, “bad”, “right”, “wrong”, “should” and “ought”. Incongruence: Sending verbal and non-verbal messages that contradict one another. Underloading: Remaining silent and unresponsive, not picking up cues, and failing to give feedback. False reassurance/ agreement: Using cliché’s to reassure client Invalidation: Ignoring or denying another’s presence, thoughts or feelings. Changing the subject: Introducing new topic inappropriately, a pattern that may indicate anxiety. Giving advice: Telling the client what to do, giving opinions or making decisions for the client, implies client cannot handle his or her own life decisions and that the nurse is accepting responsibility for client. Internal validation: Making an assumption about the meaning of someone else’s behavior that is not validated by the other person (jumping to conclusion) EXAMPLE What’s your name? I see you like sports. Where do you live? You shouldn’t do that, its wrong. The nurse tells a patient “I’d like to spend time with you” and then walks away. The patient asks and the nurse simply walks away. It’s going to be alright. This sunshine is good for my roses. I have beautiful rose garden. The client is crying or discussing his fear of surgery, when the nurse asks “ how many children do you have?” If I were you…. Or it would be better if you do it this way… The nurse sees a suicidal client smiling and tells another nurse the patient is in cheerful mood. OTHER INEFFECTIVE BEHAVIORS AND RESPONSES: Defending- Your doctor is very good Requesting an explanation- Why did you do that? Rejecting- You are not supposed to talk like that Literal responses- If you feel empty then you should eat more. Looking too busy. Appearing uncomfortable is silence Being opinionated. Avoiding sensitive topics. Arguing and telling client he is wrong. Having a closed posture- Crossing arms on chest. Making false promises- I’ll make sure to call you when you get home. Ignoring the patient- I can’t talk to you now. Making sarcastic remarks. Laughing nervously. Showing Disapproval-You should not do these things. Cliché- always look at the brighter side of life so you will not feel depressed. eaf’24 6