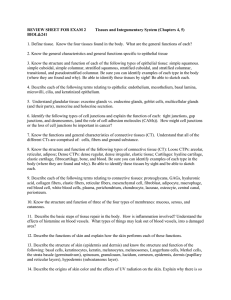
BIOL 221 - Epithelium Cristofre Martin Department of Biochemistry St. George’s University Lecture objectives • • • • • • • • • Students should be able to: List the various levels of organization in the body. List the basic tissue types. Explain functions and locations of epithelial tissues. Describe the types of secretion from epithelial cells. List the distinctive characteristics of epithelium. Describe basic cell shapes, and layering variations. List locations in the body of the different epithelium. Discuss mitotic rate in epithelium, and why it makes epithelium vulnerable to traditional chemotherapy. • Describe the various cell junctions and their functions. • Identify slides of epithelium • Describe human diseases of the epithelium. Levels of organization in the body Cell: the smallest functional unit in the body. Eg. Neuron cell Tissue: a group of like cells that are similar in both structure and function. Eg. Lung tissue Organ: an organized group of tissues, accomplishing specific functions. Eg. heart Organ system: group of organs working together. Eg. Circulatory system Types of tissue • Epithelial – Coverings – Lining of body surfaces Eg. skin • Connective – Support Eg. bone, cartilage, ligaments and fat • Muscle -location and movement • Nervous -control, sensory Eg. Brain, nerves Epithelium • Epithelial tissue is found as a covering and lining in the body. It includes: 1. the outer (epidermal) layer of skin 2. the lining of the digestive tract 3. the lining of blood vessels, kidney tubules, glands and outgrowths of the digestive tract (liver, gall bladder) Functions of epithelial tissues: • Protection from mechanical damage, sun exposure and bacteria • Reduction of friction • Absorption of nutrients by the lining of the small intestine into the blood • Filtration of wastes from the blood plasma by the lining of kidney tubules • Regulation of water loss • Sensory surface for reception of stimuli • Secretion of materials (glandular) Characteristics of epithelium • • • • Cells are close together and avascular Form sheets of cells One surface is free (luminal surface); the opposing surface rests on a basement membrane that anchors the cells to the connective tissue Lateral cell surfaces are in close contact Apex (free surface of cell) (apical end) Base of cell(basal end) Epithelial tissues are classified based on cell shape and the number of cell layers Squamous – flattened Cuboidal - cubes Columnar - columns Squamous cells have a flat, two dimensional appearance. 8/5/24 Squamous cells have a flat, two dimensional appearance. Cuboidal: shaped like a cube: height, width and depth (when visible) are about the same. The nucleus is usually centrally located. Most secretory cells of glands are cuboidal epithelial cells. In addition, the ducts of most exocrine glands are lined by cuboidal cells as are most of the tubules in the kidneys. Columnar: length is greater than width; nucleus is usually located toward the base of the cell. They have the largest cytoplasmic volumes of all epithelia. Cells possess the organelle density and energy reserves to engage in secretory or absorptive functions. Simple columnar epithelia with microvilli line the small intestine. Ciliated types are found in small bronchioles of the respiratory tract and in the fallopian tubes of the female reproductive tract. Microilli vs cilia? Classification based on the number of layers • simple • stratified • pseudostratified • transitional Simple: a single layer; all cells touch the basement membrane and the outer surface or the lumen. Simple epithelia secrete fluids that lubricate tissues. Other simple epithelia line body tracts as protective, absorptive, or secretory cells. As linings in the alveoli(air sacs), kidneys, and blood vessels, simple squamous types assist in diffusion, osmosis and filtration phenomena. Stratified: more than one layer, only the top layer is in contact with the surface; only the bottom layer rests on the basement membrane. (basal lamina). Stratified epithelia are found covering the exterior body surfaces and lining portions of the body tracts where friction phenomena occur. A multilayered epithelium allows deeper cells to replace the more superficial cells as they are damaged or cast off from the epithelial free surface. Although most prevalent in the skin and portions of the digestive and reproductive tract, stratified epithelia can be found in some large ducts and tubules. 24 Pseudostratified: all cells touch the basal lamina, but not all reach the outer surface. There is a perception of layers. Pseudostratified epithelia are most prevalent in the respiratory tract as ciliated types. Transitional: large dome-shaped cells on the luminal surface in a relaxed state. Name comes from the ability of this epithelium to accommodate stretching in the urinary tract as fluid pressures vary. It is found as a lining of the ureters, urethra, and bladder. Nomenclature The classification or naming system used to identify epithelia is based on three key criteria: 1. No. of cell layers 2. Cell shapes 3. Surface modifications The exceptions to this nomenclature are pseudostratified and transitional epithelia. If stratified epithelium consists of differently shaped cell in the various layers (a common condition), the tissue is named according to the shape of the cells on the free surface. • Note: there are limits to the thickness of epithelial tissues, since they are AVASCULAR and nutrients must be distributed by diffusion. • Skin and esophagus are about 30 cells deep. Epithelial cells of the human body Epithelial cells of the human body • Simple squamous lines blood vessels, pleural and peritoneal cavities • Stratified squamous non-keratinized lines moist body surfaces: mouth, esophagus, vagina • Stratified squamous keratinized- epidermis. Outer layers lose their nuclei, become flattened, accumulate keratin. (waterproof) (Compare water loss of keratinized face and non-keratinized lips) Epithelial cells of the human body • Simple cuboidal - kidney tubules; thyroid follicles…. • Stratified cuboidal - two or more layers of cuboidal cells. This is found in sweat glands. • Simple columnar - lines the stomach and intestines. • Simple columnar with cilia is found in the oviducts/ fallopian tubes. • Cilia- tiny hair-like structures on the surface of cells which help move entire cells or particles along the outer surface of cells. • Microvilli -increase surface area for absorption. Brush border- microvillus covered surface of simple cuboidal or simple columnar epithelium Epithelial cells of the human body • Stratified columnar- two or more layers of cells, the luminal layer is columnar. Found in excretory ducts of some glands. • Pseudo-stratified columnar epithelium: • with cilia (hairlike): found in trachea and bronchi. • with stereocilia (bundles of actin filaments): found in vas deferens and epididymis (male reproductive tract), inner ear Cell Junctions Many cells are held together by junctions, which vary in structure, depending on their function. Types of cell junctions: • Tight junctions (occluding junctions) • Anchoring junctions • Communicating junctions Tight junctions Tight junctions encircle the cell like a belt around pants.Tight junctions connect plasma membranes of adjacent cells in a sheet.This prevents small molecules slipping between cells and through the cellular layer. Nutrients absorbed from the digestive tract must pass through the cells to enter the blood. Tight junctions prevent substances from moving between cells Tight junction Intermediate filaments Desmosome Tight junctions are composed of strands of proteins – mainly claudin and occludin and associate with actin filaments in the cell. Gap junctions Space between cells Plasma membranes of adjacent cells Extracellular matrix Fig. 6-32b Tight junctions play a crucial role in the protection of the sperm in the testes and the brain. For example, tight junctions of Sertoli cells form the bloodtestes barrier which protects developing sperm. Tight junctions also maintain the blood brain barrier. Tight junction The cells lining the small intestine form a sheet one cell layer thick. One surface faces the lumen, the opposite surface rests on the basal lamina, which is in direct contact with connective tissue, containing many blood vessels. Anchoring junctions • Anchoring junctions mechanically attach the cytoskeleton of a cell to the cytoskeletons of other cells or to the extracellular matrix. • Anchoring junctions are most common in tissue subject to mechanical stress, such as muscle and the epithelium of the skin. • Cytoskeletal elements include: – A. Intermediate filaments: sturdy, long term molecules. – B. Actin filaments: delicate, often transient molecules. Types of Anchoring Junctions • Cadherin-mediated junctions – Desmosomes – Adherens junctions – Integrin-mediated junctions hemidesmosomes Cadherin mediated junctions Cadherins are single pass transmembrane glycoproteins* that attach adjacent cells. Desmosomes connect adjacent cells and are anchored to intermediate filaments. Adherens junctions also attach surrounding cells and are anchored to actin filaments. *Glycoprotein: protein +saccharide side chain. In desmosomes, the cytoplasmic end of the cadherin is connected to intermediate filaments. The other end projects outward from the plasma membrane, joining directly with a cadherin protruding from an adjacent cell, binding the cells together. (Note the reinforcing plaque.) 8/5/24 Fig. 6-32c Desmosome 1 µm In adherens junctions, cadherins attach to an actin framework which forms a less stable link than intermediate filaments. 8/5/24 Integrin mediated junctions Hemidesmosomes anchor epithelial cells to the underlying basement membrane. Integrins are composed of two different subunits that extend outward from the basement membrane. Together these units bind a protein component of the extracellular matrix like two hands grasping a pole. Keratin filaments and hemidesmosomes connect epithelial cells to the basal lamina. Human disease such as epidermolysis bullosa simplex cause severe blistering of the skin and are the result of mutations in keratin genes that are expressed in the basal cell layer of the epidermis. Epidermolysis bullosa simplex (EBS) is characterized by fragility of the skin that results in non-scarring blisters of the skin caused by little or no trauma. EBS disease is characterized by rupturing of cells in the basal layer of the epidermis between the nucleus and the hemidesmosomes which connect the keratin filaments to the basal lamina. Communicating Junctions • Communicating junctions link the cytoplasm of adjacent cells. • They are open channels for the rapid flow of ions and small molecules. • These junctions are formed by connexons, complexes of 6 identical transmembrane proteins. The proteins are arranged in a circle, creating a channel that protrudes from the cell surface. • When the channels of two adjacent cells align perfectly, a gap junction is formed. Connexons hold two cells slightly apart, hence the term “gap junction”. Connexons can respond to the level of ions in a cell, closing a channel when appropriate. Gap junctions are present in heart muscle and play a significant role in signal transmission there. Recall: only tight junctions involve direct contact of adjoining cell membranes. 8/5/24 Fig. 6-32d Gap junction Glands • Exocrine glands have ducts. Secretions of liver, salivary glands, pancreas, empty into the GI tract; mammary, sebaceous, and sweat glands empty externally. • Endocrine glands are ductless and empty secretions directly into the blood. Glands of the skin Sebaceous glands -Clumps of epithelial tissue distributed within dermis and all over the body -Secrete an oily, fat-based substance into hair follicle pore that serves to bring it to the surface -Lubricates and waterproofs the skin Eccrine sweat glands -concentrated on hands and soles of feet and forehead, secrete sweat (water and NaCl) to cool body -also secrete sweat during fear or strong emotion. -composed of tubes of cuboidal cells Merocrine secretion: Cells that secrete products via the merocrine method form membrane-bound secretory vesicles internal to the cell. These are moved to the apical surface where the vesicles coalesce with the membrane on the apical surface to release the product. Most common mechanism of secretion. Example, eccrine sweat glands Aprocrine secretion: The apical portions of cells are pinched off and lost during the secretory process. This results in a secretory product that contains a variety of molecular components including those of the membrane. Example, mammary glands, sweat pheromones in some animals (possibly humans). Holocrine secretion: Involves death of the cell. The secretory cell is released and as it breaks apart, the contents of the cell become the secretory product. Example, sebaceous glands Epithelium and mitosis • Epithelium has a very high mitotic rate. • Anything that interferes with mitosis in the body affects the epithelium. • Ex., Anti-mitotic chemotherapy often causes hair loss, skin lesions, loss of GI epithelium • High mitotic rate and exposure to radiation such as UV light makes skin cells prone to cancer (mutation)
![Histology [Compatibility Mode]](http://s3.studylib.net/store/data/008258852_1-35e3f6f16c05b309b9446a8c29177d53-300x300.png)