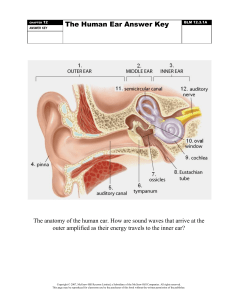
The Somatic Nervous System Chapter 14 Chapter Objectives ▪ Describe the components of the somatic nervous system ▪ Name the modalities and submodalities of the sensory systems ▪ Distinguish between general and special senses ▪ Describe regions of the central nervous system that contribute to somatic functions ▪ Explain the stimulus-response motor pathway Sensory Perception 14.1 Sensory Perception • A component of the somatic nervous system. • The somatic nervous system is responsible for our conscious perception of the environment and our voluntary responses to that perception by means of skeletal muscles. • Sensory receptors detect environmental stimuli and relay information through sensory neurons to the brain for processing. This Photo by Unknown Author is licensed under CC BY General Properties of Receptors • Sensation—a subjective awareness of the stimulus ▫ Most sensory signals delivered to the CNS produce no conscious sensation !!!! Filtered out in the brainstem before reaching the cortex, thus preventing information overload Some signals do not require conscious awareness like pH and body temperature Receptor Classification By Structure Receptor Classification By Location of Stimulus ▪Exteroceptor ▪ Receives external stimuli from environment ▪Interoceptor ▪ Receives internal stimuli from visceral organs ▪Proprioceptor ▪ Receives stimuli about body position and movement Receptor Classification By Function ▪Chemoreceptor (responds to chemical stimuli) ▪Nociceptor (detects pain) ▪Mechanoreceptor (responds to physical stimuli – pressure, vibration, & body position) ▪Thermoreceptor (sensitive to temperature) Sensory Modalities • General sense ▫ Distributed throughout body • Special sense ▫ Specific organ dedicated to it • Modality ▫ Refers to how information is encoded Somatosensation (General Sense) ▪ A group of sensory modalities that are associated with touch, proprioception, and interoception. The receptors are spread throughout the body. Mechanoreceptors of Somatosensation Name Historical Name Location(s) Stimuli Free nerve endings * Dermis, cornea, tongue, joint capsules, visceral organs Pain, temperature, mechanical deformation Mechanoreceptors Merkel’s discs Epidermal–dermal junction, mucosal membranes Low frequency vibration (5–15 Hz) Somatosensation (General Sense) Mechanoreceptors of Somatosensation Name Historical Name Location(s) Stimuli Tactile corpuscle Meissner’s corpuscle Papillary dermis, especially in the fingertips and lips Lamellated corpuscle Pacinian corpuscle Deep dermis, Deep pressure, highsubcutaneous tissue frequency vibration (around 250 Hz) Hair follicle plexus * Wrapped around hair follicles in the dermis Light touch, vibrations below 50 Hz Movement of hair Somatosensation (General Sense) Mechanoreceptors of Somatosensation Name Historical Name Location(s) Muscle spindle * In line with skeletal Muscle contraction muscle fibers and stretch Tendon stretch organ Golgi tendon organ In line with tendons Stretch of tendons Bulbous corpuscle Ruffini’s corpuscle Dermis, joint capsules Stimuli Stretch Gustation ▪ Sense of taste is associated with the tongue and provides information about the foods and liquids we consume. ▪ Basic Taste Sensations: sweet, salty, sour, bitter, umami, and fats/lipids ▪ Water receptors in taste buds located in the pharynx ▪ Taste buds are found in the papillae of the tongue ▪ Composed of chemoreceptors ▪ Chemicals must be dissolved in the saliva to taste ▪ Gustation decrease dramatically with age ▪ Ageusia: loss of the sense of smell Lingual Papillae Taste Buds Gustatory Pathway This Photo by Unknown Author is licensed under CC BY Connection of Taste and Smell • Both taste (gustation) and smell (olfaction) are chemical senses • Sense of taste is heavily connected to sense of smell • Without smell, many foods cannot be properly tasted or distinguished (often severe cold congestion that blocks up the nasal cavities affects our sense of taste for this reason) 17 Olfaction • Olfactory cells Olfaction ▫ Are neurons ▫ Head bears 10 to 20 cilia called olfactory hairs ▫ Have binding sites for odorant molecules and are nonmotile ▫ Axons collect into small fascicles and leave cranial cavity through the cribriform foramina in the ethmoid bone ▫ cranial nerve I Olfactory Pathway ▪ The olfactory tracts reach the olfactory cortex located within the temporal lobe of the cerebrum. Anosmia – loss of the sense of smell Hearing and Equilibrium • Hearing—a response to vibrating air molecules • Equilibrium—the sense of motion, body orientation, and balance • Both senses reside in the inner ear, a maze of fluidfilled passages and sensory cells • Fluid is set in motion and the sensory cells convert this motion into an informative pattern of action potentials (mechanoreceptors!!) Audition (Sense of Hearing) ▪ Anatomy of the Ear Audition (Sense of Hearing) ▪ Anatomy of the Ear This Photo by Unknown Author is licensed under CC BY • Ear has three sections: outer, middle, and inner ear ▫ First two are concerned only with the transmission of sound to the inner ear ▫ Inner ear: vibrations converted to nerve signals Outer Ear • Outer ear—a funnel for conducting vibrations to the tympanic membrane (eardrum) ▫ Auricle (pinna) directs sound down the auditory canal Shaped and supported by elastic cartilage ▫ Auditory canal (external acoustic meatus): passage leading through temporal bone to tympanic membrane Guard hairs protect outer end of canal Cerumen (earwax)—mixture of secretions of ceruminous and sebaceous glands and dead skin cells Middle Ear • Middle ear—located in the air-filled tympanic cavity in temporal bone ▫ Tympanic membrane (eardrum) closes the inner end of the auditory canal (separates it from middle ear) Suspended in a ring-shaped groove in the temporal bone Vibrates freely in response to sound Middle Ear ▫ Auditory (eustachian) tube connects middle-ear to nasopharynx Equalizes air pressure on both sides of tympanic membrane Normally closed, but swallowing or yawning open it Allows throat infections to spread to middle ear ▫ Auditory ossicles Malleus: has long handle attached to inner surface of tympanic membrane Incus: articulates with malleus and stapes Stapes: shaped like a stirrup; footplate rests on oval window— where inner ear begins Middle-Ear Infection • Otitis media (middle-ear infection) is common in children ▫ Auditory tube is short and horizontal allows for URI to spread to middle ear ▫ Infections easily spread from throat to tympanic cavity and mastoid air cells • Symptoms ▫ Fluid accumulates in tympanic cavity producing pressure, pain, and impaired hearing ▫ Can spread, leading to meningitis ▫ Can cause fusion of ear ossicles and hearing loss • Tympanostomy—lancing tympanic membrane and draining fluid from tympanic cavity Inner Ear • Two major functions: hearing and equilibrium • Consists of a labyrinth: bony passageways lined with membranous tubes ▫ Includes: vestibule, three semicircular ducts, and cochlea ▫ Endolymph: fills the inside of the tubes ▫ Perilymph: between bone and membranous tubes • Cochlea: organ of hearing 29 Inner Ear ▪ Cochlea: hearing ▪ Semicircular canals (ducts): dynamic equilibrium ▪ Vestibule (utricle & saccule): static equilibrium Perilymph Endolymph This Photo by Unknown Author is licensed under CC BY-SA-NC Inner Ear: Cochlea • Cochlea has three fluid-filled chambers separated by membranes ▫ Scala vestibuli: superior chamber Filled with perilymph Begins at oval window and spirals to apex ▫ Scala tympani: inferior chamber Filled with perilymph Begins at apex and ends at round window ▫ Scala media (cochlear duct): middle chamber Filled with endolymph Separated from: Scala vestibuli by vestibular membrane Scala tympani by thicker basilar membrane Contains—organ of Corti: acoustic organ that converts vibrations into nerve impulses 16-31 Anatomy of the Cochlea Auditory Pathway Stimulation of Cochlear Hair Cells • Tympanic membrane vibrates in response to sound and pushes on the ossicles • Ossicles stapes pushes on oval window • Causes movement of the perilymph in the inner ear and movement of basilar membrane under cochlear hair cells ▫ As often as 20,000 times per second • Movement of hair cells with basilar membrane stimulates the cells and results in generation of a signal in the cochlear nerve CNVIII 34 Cochlea (Organ of Corti) Deafness • Deafness—hearing loss ▫ Conductive deafness: conditions interfere with transmission of vibrations to inner ear Damaged tympanic membrane, otitis media, blockage of auditory canal, and otosclerosis Otosclerosis: fusion of auditory ossicles that prevents their free vibration ▫ Sensorineural (nerve) deafness: death of hair cells or any nervous system elements concerned with hearing Factory workers, musicians, construction workers Equilibrium • Equilibrium—coordination, balance, and orientation in three-dimensional space • Vestibule receptors for equilibrium Three semicircular ducts Two chambers saccule and utricle Equilibrium Head position is sensed by…utricle and saccule composed of Macula tissue (hair cells with support cells) • Head movement sensed by semicircular canals Static Equilibrium ▪ The maculae are specialized for sensing linear acceleration, such as when gravity acts on the tilting head, or if the head starts moving in a straight line. The difference in inertia between the hair cell stereocilia and the otolith in which they are embedded leads to a shearing force that causes the stereocilia to bend in the direction of that linear acceleration. Dynamic Equilibrium Semicircular canals (ducts) • Rotary movements detected by the three semicircular ducts • Bony semicircular canals of temporal bone hold membranous semicircular ducts • Each duct is filled with endolymph and opens up as a dilated sac ampulla • Each ampulla contains crista ampullaris—mound of hair cells and supporting cells Dynamic Equilibrium ▪ Rotational movement of the head is encoded by the hair cells in the base of the semicircular canals. As one of the canals moves in an arc with the head, the internal fluid moves in the opposite direction, causing the cupula and stereocilia to bend. The movement of two canals within a plane results in information about the direction in which the head is moving, and activation of all six canals can give a very precise indication of head movement in three dimensions. Disorders of the Ear ▪ Otitis media infection middle ear ▪ Otitis externa infec external auditory canal ▪ Otalgia earache ▪ Presbycusis loss of the ability to hear high-pitched sounds ▪ Deafness: ▪ Conduction deafness ▪ Sensorineural deafness ▪ Vertigo loss of equilibrium ▪ Tinnitus ringing/clicking sounds in ear • https://www.youtube.com/watch?v=bwCz3Q8y-PM • balance---- https://www.youtube.com/watch?v=-jc4gkN8w7o • More Hearing and balance hearing and balance Vision ▪ Accessory Structures of the Eye Lacrimal Apparatus Source: https://commons.wikimedia.org/wiki/File:Tear_system-pt.svg • Lacrimal apparatus makes, distributes and drains tears. • Tears from lacrimal gland wash and lubricate eye, deliver O2 and nutrients, and prevent infection with a bactericidal lysozyme • Tears flow through lacrimal punctum (opening on eyelid edge) to lacrimal sac, then into nasolacrimal duct emptying into nasal cavity Structures of the Eye ▪ The wall of the eye is composed of three layers: the fibrous tunic, vascular tunic, and neural tunic. The Tunics • 1) Tunica fibrosa—outer fibrous layer ▫ Sclera: dense, collagenous white of the eye ▫ Cornea: transparent region of modified sclera in front of eye that admits light • 2) Tunica vasculosa (uvea)—middle vascular layer ▫ Choroid: highly vascular, deeply pigmented layer behind retina ▫ Ciliary body: extension of choroid; a muscular ring around lens Supports lens and iris Secretes aqueous humor ▫ Iris: colored diaphragm controlling size of pupil (opening) If there is a lot of melanin in chromatophores (cells) of iris—brown or black eye color If there is reduced melanin—blue, green, or gray eye color • 3) Tunica interna—retina and beginning of optic nerve The Optical Components • Optical components—transparent elements that admit light, refract light rays, and focus images on retina: cornea, aqueous humor, lens, vitreous body ▫ Cornea: transparent anterior cover ▫ Aqueous humor Serous fluid secreted by ciliary body into posterior chamber— posterior to cornea, anterior to lens Then moves through pupil to anterior chamber Reabsorbed by scleral venous sinus at same rate it is secreted The Optical Components ▫ Lens Lens fibers—flattened, tightly compressed, transparent cells that form lens Suspended by suspensory ligaments from ciliary body Changes shape to help focus light Rounded with no tension or flattened with pull of suspensory ligaments ▫ Vitreous body (humor) fills vitreous chamber Jelly fills space between lens and retina The Neural Components • Include retina and optic nerve • Retina ▫ Pressed against rear of eyeball by vitreous humor ▫ Detached retina causes blurry areas of vision and can lead to blindness • Macula lutea—patch of retina on visual axis of eye (3 mm diameter) ▫ Fovea centralis: center of macula; finely detailed images due to packed receptor cells • Optic disc—blind spot ▫ Optic nerve exits retina and there are ▫ no receptors there !!!!!!!!!! • Blind spot—use test illustration above (IN LAB) ▫ Close right eye, stare at X and red dot disappears Neural Tunic (Retina) ▪ Photoreceptors – sensitive to light ▪ Cones – for bright light & high acuity color vision ▪ Rods – for dim light & peripheral vision ▪ Fovea centralis: site of highest visual acuity; has only cones Formation of an Image • Light passes through lens to form tiny inverted image on retina • Iris diameter controlled by two sets of contractile elements ▫ Pupillary constrictor: smooth muscle encircling pupil Parasympathetic stimulation narrows pupil ▫ Pupillary dilator: spoke-like myoepithelial cells Sympathetic stimulation widens pupil Refraction of Light ▪ The bending of light rays by the anterior surface of the cornea, the lens, and the internal eye fluids (aqueous & vitreous humor) to focus directly on the retina. ▪ It produces an inverted image on the retina. Eventually, the brain will revert the image to its original orientation. Disorders of the Eye ▪ Astigmatism unequal curvature of the lens or cornea ▪ Cataracts clouding of the lens ▪ Glaucoma increased intraocular pressure which may increase and compress on the retina and optic nerve. ▪ Retinal detachment the retina detaches from the vascular layers and allow the jellylike vitreous humor to seep between them and can cause permanent blindness. ▪ Diplopia double vision ▪ Strabismus cross eyed ▪ Colorblindness ▪ Nyctalopia “night blindness” that is usually the result of a vitamin A deficiency • Hyperopia farsighted can see far can't see close well • Myopia near sighted can see near not far • Presbyopia reduced ability to accommodate for near vision WITH AGE Central Processing 14.2 Sensory Pathways ▪ Ascending Pathway (Tract) ▪ carries peripheral sensations to the brain Sensory Homunculus ▪ A map of the location of the somatosensory receptors in the body onto the somatosensory cortex. Referred Pain • Referred pain: pain in viscera often mistakenly thought to come from the skin or other superficial site ▫ Results from convergence of neural pathways in CNS ▫ Brain interprets that visceral pain is coming from skin and cannot distinguish the source • Example: heart pain felt in shoulder or arm because both areas send pain input to spinal cord segments T1 to T5 • Very important to keep in mind while diagnosing pts 60 Referred pain Motor Responses 14.3 Spinothalamic tract is part of the anterolateral system that passes up the anterior and lateral columns of the spinal cord It carries signals for pain, pressure, temperature, light touch, tickle, and itch Spinoreticular tract travels up anterolateral system Carries pain signals!!resulting from tissue injury emotional aspect of pain and is important point in pain control Spinocerebellar Tracts Carry proprioceptive signals from limbs and trunk up to the cerebellum Motor Pathways Descending (motor) tracts • Descending tracts—carry motor signals down brainstem and spinal cord!! • Involve two motor neurons ▫ Upper motor neuron originates in cerebral cortex or brainstem and terminates on a lower motor neuron ▫ Lower motor neuron soma is in brainstem or spinal cord Axon of lower motor neuron leads to muscle or other target organ Corticospinal Tracts • Corticospinal tracts carry MOTOR signals from cerebral cortex for precise, finely coordinated movements • Tectospinal tract—begins in midbrain region (tectum) ▫ Reflex turning of head in response to sights and sounds • Lateral and medial vestibulospinal tracts ▫ Begin in brainstem vestibular nuclei ▫ Receive impulses for balance from inner ear ▫ Control extensor muscles of limbs for balance control ▫ Reticulospinal tracts very involved with pain modulation/control “ descending analgesic pathways” which naturally reduce transmission of pain signals to the brain Reflex Arc ▪ Reflexes are rapid, automatic responses to specific stimuli. ▪ Five Components of a Typical Reflex Arc: ▪Receptor cell ▪Sensory neuron ▪Interneurons (association neurons) ▪Motor neuron ▪Effector cell Classification of Reflexes ▪ Development ▪ Innate reflexes ▪ Acquired reflexes ▪ The Nature of the Response ▪ Somatic reflexes ▪ Visceral reflexes ▪ Polysynaptic reflexes ▪ Monosynaptic reflexes ▪ The Processing Site ▪ Spinal reflexes ▪ Cranial reflexes Patellar Reflex (Somatic) This Photo by Unknown Author is licensed under CC BY-NC-ND Withdrawal Reflex (Somatic) This Photo by Unknown Author is licensed under CC BY-NC-ND