Benign Prostate Hyperplasia: Causes, Symptoms, & Treatment
advertisement

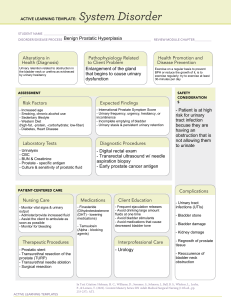
Benign Prostate Hyperplasia Benign Prostate Hyperplasia Enlargement of prostate gland resulting from increase in number of epithelial cells and stromal tissue Most common urologic problem in males 2 Benign Prostate Hyperplasia Occurs in 50% of men over 50 and 90% of men over 80 Approximately 25% will require treatment by age 80. Does not predispose to development of prostate cancer 3 Etiology and Pathophysiology Possible causes • Excessive accumulation of dihydroxytestosterone • Stimulation by estrogen • Local growth hormone action Typically develops in inner part of prostate while prostate cancer is most likely to develop in outer part. 4 Etiology and Pathophysiology Possible risk factors • Family history • Obesity • Increased waist circumference • Physical activity level • Alcohol consumption, smoking • Diabetes 5 Etiology and Pathophysiology Enlargement gradually compresses urethra. • Partial or complete obstruction Compression leads to clinical symptoms. 6 Benign Prostate Hyperplasia Fig. 55-2. Benign prostatic hyperplasia. The enlarged prostate compresses the urethra. 7 Clinical Manifestations Symptoms are usually gradual in onset. Early symptoms are usually minimal because bladder can compensate. Worsen as obstruction increases 8 Clinical Manifestations Symptoms categorized into two groups • Obstructive symptoms • Irritative symptoms 9 Clinical Manifestations Obstructive symptoms • Symptoms due to urinary retention • Decrease in caliber of force of urinary stream • Difficulty in initiating urination • Intermittency • Dribbling at end of voiding 10 Clinical Manifestations Irritative symptoms • Symptoms associated with inflammation or infection • Urinary frequency and urgency • Dysuria • Bladder pain • Nocturia • Incontinence 11 Complications Related to urinary obstruction • Acute urinary retention: complication with sudden, painful inability to urinate • Treatment involves catheter insertion and possible surgery. 12 Complications UTI and sepsis • Incomplete bladder emptying with residual urine provides medium for bacterial growth. 13 Complications Calculi may develop in bladder because of alkalinization of residual urine. Renal failure: caused by hydronephrosis Pyelonephritis Bladder damage 14 Diagnostic Studies History and PE DRE (Digital Rectal Exam) Urinalysis with culture PSA level Serum creatinine 15 Diagnostic Studies TRUS scan Uroflometry Cystoscopy 16 Collaborative Care Goals • Restore bladder drainage. • Relieve symptoms. • Prevent/treat complications. Watchful waiting Dietary changes Timed voiding schedule 17 Collaborative Care Drug therapy offers symptomatic relief of BPH • 5α-Reductase inhibitors • Example: finasteride (Proscar) • ↓ size of prostate gland • Takes 3 to 6 months for improvement • Side effects: decreased libido, decreased volume of ejaculation, ED 18 Collaborative Care • α-Adrenergic receptor blockers • Examples: tamsulosin (Flomax), Promotes smooth muscle relaxation in prostate; facilitates urinary flow • Improvement in 2 to 3 weeks • Side effects: orthostatic hypotension and dizziness, retrograde ejaculation, nasal congestion 19 Collaborative Care Transurethral microwave therapy https://youtu.be/zuN-yXqH-TI?si=50hmkGjezj_EmzIv&t=5 • Outpatient procedure: delivers microwaves directly to prostate through a transurethral probe • Heat causes death of tissue and relief of obstruction. 20 Collaborative Care Transurethral microwave therapy (cont’d) Postop urinary retention is common • Patient sent home with catheter 2 to 7 days • Antibiotics, pain medication, and bladder antispasmodic medications given 21 Collaborative Care Transurethral microwave therapy (cont’d) • Not appropriate therapy when rectal problems exist • Side effects: bladder spasm, hematuria, dysuria, and retention 22 Collaborative Care Transurethral needle ablation (TUNA) • ↑ temperature of prostate tissue for localized necrosis • Low-wave frequency used • Only tissue in contact with needle affected 23 Collaborative Care Transurethral needle ablation (cont’d) • Majority of patients show improvement in symptoms. • Outpatient uses local anesthesia and sedation. • Lasts 30 minutes with little pain and quick recovery 24 Collaborative Care Transurethral needle ablation (cont’d) • Complications include urinary retention, UTI, and irritative voiding symptoms. • Some patients require a catheter. • Hematuria up to a week 25 Collaborative Care Laser prostatectomy • Delivers a laser beam transurethrally to cut or destroy parts of the prostate • Common procedure: visual laser ablation of the prostate (VLAP) • Takes several weeks to reach optimal results • Urinary catheter inserted 26 Collaborative Care Laser prostatectomy (cont’d) • Contact laser techniques • Minimal bleeding during and after procedure • Fast recovery time • Patients may take anticoagulants. • Photovaporization of the prostate 27 Collaborative Care Invasive therapy indicated when • Decrease in urine flow sufficient to cause discomfort • Persistent residual urine • Acute urinary retention • Intermittent catheterization can reduce symptoms and bypass obstruction 28 Collaborative Care Transurethral resection (TURP) • Removal of obstructing prostate tissue using resectoscope inserted through urethra • Outcome for 80% to 90% is excellent. • Relatively low risk • Performed under spinal or general anesthesia and requires hospital stay 29 https://youtu.be/aBelQBJNDNM?si=n7E1xcpbOfEcMjYH&t =21 Fig. 55-3. Transurethral resection of the prostate. 30 Collaborative Care Transurethral resection (cont’d) • Bladder irrigated for first 24 hours to prevent mucous and blood clots • https://youtu.be/9wGZ7YjuaFA?si=mOZJtrtqTe0Sn17G&t=29 • Complications include bleeding, clot retention, dilutional hyponatremia, retrograde ejaculation. 31 Nursing Implementation Preoperative care Use aseptic technique when using urinary catheter. Administer antibiotics preoperatively. 32 Nursing Implementation Preoperative care Provide patient opportunity to express concerns over alterations in sexual function. Inform patient of possible complications of procedures. 33 Planning Goals for postoperative care • No complications • Restoration of urinary control • Complete bladder emptying • Satisfactory sexual expression 34 Nursing Implementation Postoperative care Postop bladder irrigation to remove blood clots and ensure drainage or urine Administer antispasmodics. Teach Kegel exercises. 35 Nursing Implementation Postoperative care Observe patient for signs of infection. Dietary intervention-high fiber Stool softeners to prevent straining 36 Nursing Implementation Focus: early detection and treatment Yearly physical exam and DRE for men over 50 Educate patients that alcohol, caffeine, and cold and cough meds can increase symptoms. 37 Nursing Implementation Discharge instructions on indwelling catheter Managing incontinence 2 to 3 L fluids per day Signs and symptoms of UTI, wound infection 38 Nursing Implementation Preventing constipation Avoiding heavy lifting Refraining from driving, intercourse after surgery as directed 39 Nursing Implementation Sexual counseling if erectile dysfunction becomes a problem Avoiding bladder irritants Yearly digital rectal examination (DRE) 40 Student Response Question A patient with benign prostatic hyperplasia is scheduled for a transurethral resection of the prostate (TURP). The nurse assesses the patient’s knowledge of the procedure and its effects on reproductive function, and determines a need for further teaching when the patient says, 1. “It is possible that I’ll be sterile following this procedure.” 2. “It is likely that I will become impotent from this procedure.” 3. “I understand that some retrograde ejaculation may occur.” 4. “I will have a catheter for a couple of days to keep my urinary system open.” 41