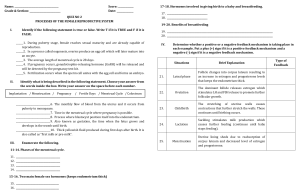
PUBERTY This increase influences the following: -Is the stage of life at which secondary sex changes - development of the uterus, fallopian tubes, and begin. vagina; -In most girls, these changes are stimulated when - typical female fat distribution; the hypothalamus synthesizes and releases - hair patterns; and gonadotropin-releasing hormone (GnRH), which then - breast development. triggers the anterior pituitary to release follicle- -It also closes the epiphyses of long bones in girls stimulating hormone (FSH) and luteinizing hormone the same way testosterone closes the growth plate in (LH). boys. -FSH and LH are termed gonadotropin (gonad= -The beginning of breast development is termed “ovary”; tropin = “growth”) hormones not only because thelarche, which usually starts 1 to 2 years before menstruation. they begin the production of androgen and estrogen, which in turn initiate secondary sex characteristics, but also because they continue to cause the MENSTRUATION production of eggs and influence menstrual cycles -A menstrual cycle (the female reproductive cycle) is throughout women’s lives episodic uterine bleeding in response to cyclic THE ROLE OF ANDROGEN Androgenic hormones are the hormones responsible for: 1) muscular development 2) physical growth 3) increase in sebaceous gland secretions that cause typical acne in both boys and girls during adolescence. In males, androgenic hormones are produced by the adrenal cortex and the testes and, in females, by the adrenal cortex and the ovaries. hormonal changes. -The purpose of a menstrual cycle is to bring an ovum to maturity and renew a uterine tissue bed that will be necessary for the ova’s growth should it be fertilized. Menarche -First menstruation -May occur as early as 9 years of age -It is good to include health teaching information on menstruation to both school-age children and their THE ROLE OF ANDROGEN IN MALES parents as early as fourth grade as part of routine care. The level of the primary androgenic hormone, The length of menstrual cycles testosterone, is low in males until puberty (between ages 12 and 14 years) when it rises to influence pubertal changes in the testes, scrotum, penis, prostate, and seminal vesicles; the appearance of male pubic, axillary, and facial hair; laryngeal enlargement with its accompanying voice change; -differs from woman to woman. -average length is 28 days (from the beginning of one menstrual flow to the beginning of the next). -It is not unusual for cycles to be as short as 23 days or as long as 35 days. maturation of spermatozoa; and closure of growth The length of the average menstrual flow (termed plates in long bones (termed adrenarche). menses) THE ROLE OF ANDROGEN IN GIRLS -4 to 6 days -although women may have flows as short as 2 days or In girls, testosterone influences the following: as long as 9 days 1)enlargement of the labia majora and clitoris 2) formation of axillary and pubic hair. Characteristics Beginning (menarche) THE ROLE OF ESTROGEN When triggered at puberty by FSH, ovarian follicles in females begin to excrete a high level of the hormone estrogen. Interval between cycles Description Average age at onset, 12.4 years; average range, 9–17 years Average, 28 days; cycles of 23–35 days not unusual Duration of menstrual flow Amount Color Odor Average flow, 4–6 days; ranges of 2–9 days not abnormal -Difficult to estimate; -Average 30–80 ml per menstrual period; -Saturating a pad or tampon in less than 1 hr is heavy bleeding Dark red; •A combination of blood, mucus, and endometrial cells Similar to marigolds The Ovaries -Every month during the fertile period of a woman’s life (from menarche to menopause), one of the ovary’s oocytes is activated by FSH to begin to grow and mature. -As the oocyte grows, its cells produce a clear fluid (follicular fluid) that contains a high degree of estrogen and some progesterone. -As the follicle surrounding the oocyte grows, it is propelled toward the surface of the ovary. -At full maturity, the follicle is visible on the surface of the ovary as a clear water blister approximately 0.25 to 0.5 in. across. -At this stage of maturation, the small ovum (barely visible to the naked eye, about the size of a printed THE PHYSIOLOGY OF MENSTRUATION period) with its surrounding follicular membrane and fluid is termed a Graafian follicle. Four body structures are involved: By day 14 or the midpoint of a typical 28-day cycle, 1. Hypothalamus 2. Anterior pituitary gland the ovum has divided by mitotic division into two separate bodies: 3. Ovaries 1.)a primary oocyte, which contains the bulk of the 4. Uterus cytoplasm, and - For a menstrual cycle to be complete, all four 2) a secondary oocyte, which contains so little organs must contribute their part; cytoplasm that it is not functional. -Inactivity of any part results in an incomplete or ineffective cycle -The structure also has accomplished its meiotic The Hypothalamus division, reducing its number of chromosomes to the haploid (having only one member of a pair) number of 23. -Release of the GnRH (also called luteinizing -After an upsurge of LH from the pituitary at about hormone–releasing hormone [LHRH]) from the day 14, prostaglandins are released and the graafian hypothalamus initiates the menstrual cycle. follicle ruptures. -GnRH then stimulates the pituitary gland to send -The ovum is set free from the surface of the ovary, the gonadotropic hormone to the ovaries to produce a process termed ovulation. It is swept into the open estrogen. end of a fallopian tube. -When the level of estrogen rises, release of GnRH is -It is important to teach women that ovulation does repressed and no further menstrual cycles will occur. not necessarily occur on the 14th day of their cycle; The Anterior lobe of the Pituitary Gland (the adenohypophysis) -Under the influence of GnRH, produces two hormones: 1)FSH, a hormone active early in the cycle that is responsible for maturation of the ovum 2)LH, a hormone that becomes most active at the midpoint of the cycle and is responsible for ovulation, or release of the mature egg cell from the ovary. -> It also stimulates growth of the uterine lining during the second half of the menstrual cycle. -it occurs 14 days before the end of their cycle. -If their menstrual cycle is only 20 days long, for example, their day of ovulation would be day 6 (14 days before the end of the cycle). If their cycle is 44 days long, ovulation would occur on day 30, not at the halfway point—day 22. After the ovum and the follicular fluid have been discharged from the ovary, the cells of the follicle remain in the form of a hollow, empty pit. -The FSH has done its work at this point and now decreases in amount. -The second pituitary hormone, LH, continues to rise in amount and directs the follicle cells left behind in the ovary to produce lutein, a bright-yellow fluid high in progesterone. quantities of glycogen (an elementary sugar) and -With lutein production, the follicle is renamed a mucin (a protein). corpus luteum (yellow body). -It takes on the appearance of rich, spongy velvet. -The basal body temperature of a woman drops -Is termed the progestational, luteal, premenstrual, slightly (by 0.5° to 1°F) just before the day of or secretory phase. ovulation because of the extremely low level of progesterone that is present at that time. The Third Phase of the Menstrual Cycle (Ischemic) -It rises by 1°F on the day after ovulation because of -If fertilization does not occur, the corpus luteum in the concentration of progesterone, which is the ovary begins to regress after 8 to 10 days, and thermogenic. therefore, the production of progesterone -The woman’s temperature remains at this elevated decreases. level until approximately day 24 of the menstrual -With the withdrawal of progesterone, the cycle, when the progesterone level again decreases endometrium of the uterus begins to degenerate (at -If conception (fertilization by a spermatozoon) about day 24 or day 25 of the cycle). occurs as the ovum proceeds down a fallopian tube -The capillaries rupture, with minute hemorrhages, and the endometrium sloughs off. and the fertilized ovum implants on the endometrium of the uterus, the corpus luteum remains throughout the major portion of the pregnancy (to about 16 to 20 weeks). -If conception does not occur, the unfertilized ovum atrophies after 4 or 5 days, and the corpus luteum (now called a “false” corpus luteum) remains for only 8 to 10 days. --As the corpus luteum regresses, it is gradually replaced by white fibrous tissue, and the resulting structure is termed a corpus albicans (white body). The Uterus Uterine changes that occur monthly as a result of stimulation from the estrogen and progesterone produced by the ovaries. The First Phase of the Menstrual Cycle (Proliferative) -Immediately after a menstrual flow (which occurs during the first 4 or 5 days of a cycle) -the endometrium, or lining of the uterus, is very thin, approximately one cell layer in depth. -As the ovary begins to produce estrogen (in the follicular fluid, under the direction of the pituitary FSH), the endometrium begins to proliferate so rapidly the thickness of the endometrium increases as much as eightfold from day 5 to day 14. -ALSO CALLED the proliferative, estrogenic, follicular, or postmenstrual phase. The Fourth Phase of the Menstrual Cycle (Menses) *Menses, or a menstrual flow, is composed of a) a mixture of blood from the ruptured capillaries; b)mucin; c) fragments of endometrial tissue; d) and the microscopic, atrophied, and unfertilized ovum. -Because it is the only external marker of the cycle, however, the first day of menstrual flow is used to mark the beginning day of a new menstrual cycle. -Contrary to common belief, a menstrual flow contains only 30 to 80 ml of blood; -if it seems to be more, it is because of the accompanying mucus and endometrial shreds. -The iron loss in a typical menstrual flow is approximately 11 mg. -This is enough loss that many adolescent women could benefit from a daily iron supplement to prevent iron depletion during their menstruating years CERVICAL CHANGES -The mucus of the uterine cervix also changes in structure and consistency each month during a menstrual cycle. -At the beginning of each cycle, when estrogen secretion from the ovary is low a) Cervical mucus is thick and scant. b) Sperm survival in this type of mucus is poor. The Second Phase of the Menstrual Cycle -At the time of ovulation, when the estrogen level (Secretory) has risen to a high point: a) Cervical mucus becomes thin, stretchy (spinnbarkeit), and copious. *After ovulation, the formation of progesterone in the corpus luteum (under the direction of LH) causes the glands of the uterine endometrium to become corkscrew or twisted in appearance and dilated with Spinnbarkeit Sperm penetration and survival in this thin mucus are both excellent. The second half of the cycle a) progesterone becomes the major influencing hormone b) cervical mucus again thickens c) sperm survival is again poor. During ovulation a) the body of the cervix is softer b) the cervical os is slightly open ACTIONS OF SEX HORMONES: Estrogen and Progesterone Estrogen -Controls development of female secondary sex characteristics -Assists in the maturation of the ovarian follicles -Causes uterus to increase in size and weight -Increases myometrial contractility in uterus and fallopian tubes -Increases uterine sensitivity to oxytocin -Inhibits FSH production Stimulates LH production Progesterone -Decreases uterine motility and contractility -Causes uterine endometrium to increase its supply of glycogen, arterial blood, secretory glands, amino acids, and water -Vaginal epithelium proliferates -Causes cervix to secrete thick, viscous mucus -Increases breast glandular tissue -Prepares breast for lactation Hormone for “Pregnancy” PROSTAGLANDINS (PGs) -Oxygenated fatty acid produced by the cells of the endometrium -Also classified as hormones and are found in and around the follicle at the time of the ovulation -Necessary for follicular rupture OXYTOCIN -A natural hormone secreted by the hypothalamus and stored in the Posterior Pituitary Gland -Manages labor and delivery and lactation Has synthetic form for induction of labor