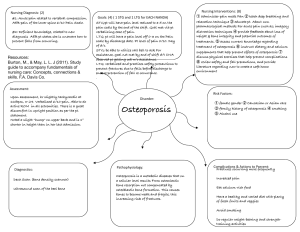
IJPHCS Open Access: e-Journal International Journal of Public Health and Clinical Sciences e-ISSN : 2289-7577. Vol. 4:No. 1 January/February 2017 An overview of osteoporosis and heath promotional strategies for community based osteoporosis prevention in Malaysia Samia A1, Hejar A. R.2*, Suriani I2, Emilia Z.A.3 1 Student, PhD in Epidemiology & Biostatics, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia. 2 Department of Community Health, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia. 3 Department of Environmental and Occupational Health, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Serdang, Selangor, Malaysia. *Corresponding author: Hejar Abdul Rahman, arhejar@yahoo.com ABSTRACT Osteoporosis is a global health problem which affects financial resources for prevention and treatment. It is generally a silent disease, undiagnosed until what would otherwise be a minor trauma from a fall causing a fracture, most commonly occurs at the hip, spine or wrist. It not only causes increase economic burden but also leads to social, physical and psychological consequences which expected to affect more people worldwide by 2050. It is no longer confined to the growing older population but has implications for all age groups. But with the progression of age, bone break down slowly over takes bone formation, resulting in gradual bone loss and more porous, osteoporosis is likely to occur. Such gradual change inevitably contribute progressively to morbidity. An inactive lifestyle, insufficient calcium intake, heavy smoking, excessive alcohol consumption, poor diet, menopausal woman, aged over 50, or have a family history of osteoporosis increase the risk of osteoporotic fractures. Osteoporosis is preventable with proper nutrition and lifestyle habits at the community level through health promotion & education which is effective in improving knowledge and awareness. So educating people on predisposing factors and symptoms of osteoporosis would be one of the best choice for increasing knowledge of osteoporosis inducing behavioural change in the period of peak bone density which is beneficial. Public awareness of osteoporosis remains low, especially in developing countries. So, heath promotional strategies for community based osteoporosis prevention in Malaysia is essential and recommended. Keywords: Osteoporosis, prevention, health promotional strategies, Malaysia Samia A, Hejar A. R., Suriani I, Emilia Z.A. 28 IJPHCS Open Access: e-Journal International Journal of Public Health and Clinical Sciences e-ISSN : 2289-7577. Vol. 4:No. 1 January/February 2017 1.0 Introduction Osteoporosis is a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture (NIH Consensus, 2001). World health organization (WHO) defines osteoporosis as a bone mineral density value more than 2.5 SD below the mean for normal, young, white women (WHO, 2003). Osteoporosis may be invisible and painless, but this ‘silent’ disease results in fractures which cause pain, disability, and ultimately loss of independence or premature death. So, people with osteoporosis to protect themselves against fractures by adopting a bone-healthy lifestyle in tandem with appropriate medical treatment. 2.0 Global Osteoporosis burden Osteoporosis is a global epidemic. The prevalence of osteoporosis is increasing and affects the economic status of the world (Barzanji AT, 2013). Osteoporosis is estimated to affect 200 million women worldwide - approximately one-tenth of women aged 60, one-fifth of women aged 70, two-fifths of women aged 80 and two-thirds of women aged 90 (Kanis JA, 2007). Worldwide, 1 in 3 women over age 50 will experience osteoporotic fractures and 1 in 5 men aged over 50 (Kanis et al, 2000). Globally, osteoporosis causes more than 8.9 million fractures annually, resulting in an osteoporotic fracture every 3 seconds (Johnell O & Kanis JA, 2006). By 2050, the worldwide incidence of hip fracture in men is projected to increase by 310% and 240% in women, compared to rates in 1990 (Gullberg B, Johnell O, Kanis JA, 1997). In the European Union (EU), in 2010, out of 21.3 million people considered to be at a high risk for osteoporotic fractures, 12.3 million were left untreated. Fracture risk in the Asian population is lower compared to the Western population (Kanis et al, 2012). However, with the rapid expansion of the elderly population in Asia, the incidence of osteoporosis is projected to increase significantly, so that by 2050, 50% of all hip fractures would occur in this region (Cooper et al, 1992). It is projected that 45% of the osteoporotic hip fractures will occur in Asia by 2050, an increase from 26% in 1990 (Gullberg B, Johnell O, Kanis JA, 1997). Osteoporotic fractures incur significant healthcare and economic burdens. A recent study in the South Korean population indicated that the societal cost of osteoporotic fractures, inclusive of direct and indirect medical costs, increased from USD $8.8 million in 2007 to $149.3 million in 2011(Kim J et al, 2015). Another study in the Eastern Saudi Arabian population showed that the treatment cost of osteoporotic fractures of the femur for the first year was USD $628.95 million, with a projected lifetime cost of $9.34 billion in 2025(SadatAli et al, 2015). Samia A, Hejar A. R., Suriani I, Emilia Z.A. 29 IJPHCS Open Access: e-Journal International Journal of Public Health and Clinical Sciences e-ISSN : 2289-7577. Vol. 4:No. 1 January/February 2017 3.0 Epidemiology of Osteoporosis in Malaysia The prevalence of osteoporosis in Malaysia was reported as 24.1% in 2005, predominantly affecting the hip among the elderly (Lim et al, 2005). Osteoporosis research in Malaysia is very limited. The most comprehensive survey in hip fracture incidence was performed in 1996–1997 which was a retrospective study, whereby it was demonstrated that the rate was 218/100,000 for women and 88/100,000 for men (Lee JK & Khir ASM, 2007). The direct hospitalization cost for hip fracture in 1997 was estimated conservatively at RM 22 million (Lee JK & Khir ASM, 2007). In Malaysia, significant ethnic differences in hip fracture incidence were found, 63% of patients presenting with hip fractures were Chinese. This was followed by Malays at 20% and Indians, 13%. Race-specific incidence data showed that the fracture rates are highest among the Chinese (160 per 100 000) followed by Indians (150 per 100 000) and Malays (30 per 100 000) (Damodaran et al, 2000). Race and sex-specific incidence data showed that the incidence was highest among Chinese females (220 per 100 000), followed by Indian females (200 per 100 000) (Damodaran et al, 2000). The age-specific incidence was 500 per 100 000 for patients above 75 years, compared to 10 per 100 000 in those between 50 and 54 years and individuals above 50 years of age was 90 per 100,000 populations (Lee & Khir, 2007). These figures translate to a 5.2% lifetime risk for a woman living to an average female life expectancy of 74 years. Hence a fracture induced by osteoporosis is likely to be a primary cause of mortality for at least 2.6% of the female population of Malaysia (Lau et al, 2001). Females were twice as commonly affected compared to males. The percentage of females in the population of Malaysia of 70 years and over was 54.2% in 1990 and has estimated that it will increase to 56.7% by 2020 (Karim, 1997). All these considerations suggest that while few adequately detailed clinical studies have been undertaken in Malaysia to make accurate predictions, the next decade will see a strong increase in osteoporosis-related trauma and resulting morbidity. 4.0 Pathogenesis and Risk factors In osteoporosis, bone mass decreases gradually and painlessly, resulting in weak, fragile, brittle bones which are prone to fractures. There are several factors associated with osteoporosis including age, endocrine changes, lifestyles, general health condition, and certain medications (Dontas, 2007). Samia A, Hejar A. R., Suriani I, Emilia Z.A. 30 IJPHCS Open Access: e-Journal International Journal of Public Health and Clinical Sciences e-ISSN : 2289-7577. Vol. 4:No. 1 January/February 2017 Table 1: Secondary causes of osteoporosis Endocrine Hyperthyroidism, Hyperparathyroidism, Cushing disorder disease Gastrointestinal Postgastrectomy, Chronic liver disease, Malabsorption disorder syndrome Bone disease Osteogenesis imperfect, Malignancy Drugs Steroid, Heparin, Furosemide, Thyroxin, progesterone, cytotoxic drugs. Others Hypercalciuria, Vitamin D deficiency, Hemochromatosis, Hypophosphatasia. Source: U.S. Department of Health and Human Services. Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Office of the Surgeon General, 2004 Primary osteoporosis is characterized by reduction of bone mass due to the aging process. Secondary osteoporosis is caused by exogenous drugs or systemic disease affecting bone metabolism. These causes which list out above in Table 1 must be excluded before primary osteoporosis is diagnosed as some of these are treatable medical conditions. Studies had postulated a few mechanisms in the pathogenesis of primary osteoporosis. One theory is related to chronic inflammatory process influence on the bone turnover. Proinflammatory cytokines have been implicated in the regulation of osteoblasts and osteoclasts and activation of immune system in the ageing process (Ginaldi et al, 2005; De Martinis et al, 2006). Pelvic bone marrow adipose tissue (BMAT) is another factor postulated in the pathogenesis. MRI-measured BMAT is strongly inversely correlated with dual-energy x-ray absorptiometry (DXA) measured Bone marrow density (BMD) independent of other predictor variables (Lorentzon M, 2006). More research in this area is currently being carried out. Table 2: Risk factors Non-modifiable 1.Advancing age 2.Ethnic group (Oriental & Caucasian) 3.Female gender 4.Premature menopause (<45 years) including surgical menopause 5.Family history of osteoporosis or fracture in first degree relative 6.Personal history of fracture as an adult Modifiable 1.Low calcium and/or vitamin D intake 2.Sedentary lifestyle 3.Cigarette smoking 4.Alcohol intake of more than 3 units daily 5.Caffeine intake of more than 330 mg daily (more than 3 cups daily) 6.Low body weight (BMI < 19 kg/m2) 7.Estrogen deficiency 8.Frequent falls Source: U.S. Department of Health and Human Services. Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Office of the Surgeon General, 2004 The risk factors for osteoporosis are well established in many epidemiological studies. They are classified into modifiable and non-modifiable risk factors which are pointed in Table 2 Samia A, Hejar A. R., Suriani I, Emilia Z.A. 31 IJPHCS Open Access: e-Journal International Journal of Public Health and Clinical Sciences e-ISSN : 2289-7577. Vol. 4:No. 1 January/February 2017 above. Intervention on the modifiable risk factors forms the basis for counseling and primary prevention of osteoporosis in the community. 5.0 Behavioral risks for osteoporosis and fracture Five factors that are related to behavior or lifestyle have been evaluated for their relationship to osteoporosis and osteoporosis related fragility fractures: nutrition, cigarette smoking, alcohol consumption, physical activity and falls. 5.1 Nutrition Calcium is effective for preventing osteoporotic fractures in postmenopausal women. A metaanalysis reviewed the literature from 1966 to 1997 assessing the effectiveness of calcium supplementation for the prevention of osteoporotic fractures in postmenopausal women. The main finding of the review was that increased calcium intake among postmenopausal women appears to be associated with a small reduction in risk of fracture. Most of these trials found about a 30% reduction in fracture risk among those taking around 1 gram of calcium supplement/day. The meta-analysis suggests that 1g/day of dietary calcium is associated with a 24% reduction in risk of hip fracture. The rate of bone loss in untreated women aged 60 to 80 years is about 0.75% per year and that a 1000 mg calcium supplement halves the rate of bone loss, 10 years of calcium supplementation would lead to about a 4% higher bone mass in treated than untreated women. The study also stated that a 4% difference in proximal femur bone mass is equivalent to 0.25 SD, and the relative risk of hip fracture per 0.25 SD increase in bone mass is 0.78 (a 22% reduction in risk of hip fracture) (Cummings & Nevitt 1997). Vitamin D has been extensively studied regarding its impact on osteoporotic fracture risk reduction. In fact, vitamin D deficiency has been associated with greater incidence of hip fracture even in developed country, including postmenopausal women (Chapuy et al, 1992). Women with osteoporosis in United States, who were hospitalized due to hip fractures, 50% were found to have signs of vitamin D deficiency (LeBoff et al, 1999). A meta-analysis of 29 studies, with over 63,000 individuals analyzed, looked at calcium and calcium in combination with vitamin D trials for use in prevention of fracture and bone loss was recently reported in Australia. The authors concluded that treatment was associated with a 12% risk reduction in fractures of all types. Trials with higher compliance revealed significant risk reduction compared to studies with lower compliance. In the 8 studies with greater than 80% compliance, a 24% risk reduction for all fractures was identified. The author’s conclusions were that calcium, or calcium in combination with vitamin D supplementation, was effective in the preventive treatment of osteoporosis in people aged 50 years or older. It appeared that the best effect was seen with minimum doses of 1200 mg of calcium and 800 units of vitamin D daily (Tang et al, 2007). Samia A, Hejar A. R., Suriani I, Emilia Z.A. 32 IJPHCS Open Access: e-Journal International Journal of Public Health and Clinical Sciences e-ISSN : 2289-7577. Vol. 4:No. 1 January/February 2017 5.2 Cigarette smoking Smoking is widely considered a risk factor for future fracture. A meta-analysis reviewed 29 cross-sectional studies that related smoking to bone density and 19 cohort and case-control studies that reported risks of hip fracture in smokers and non-smokers. Lower BMD was found in postmenopausal women who smoked, and the relative risk of hip fracture rose progressively with age (Law M.R & Hackshaw A.K, 1997). For osteoporotic fracture, the risk ratio increased with age, but decreased with age for hip fracture. A smoking history was associated with a significantly increased risk of fracture compared with individuals with no smoking history, but the risk ratios were lower than for current smoking (Kanis et al, 2005). In another meta-analysis, 59,232 men and women (74% female) from ten prospective cohorts were followed for a total of 250,000 person-years. The effect of current or past smoking, on the risk of any fracture, any osteoporotic fracture and hip fracture alone was examined using a Poisson model for each sex from each cohort. Current smoking was associated with a significantly increased risk of any fracture compared to non-smokers (RR=1.25; 95% Confidence Interval (CI) =1.15-1.36). Risk ratios were significantly higher in men than in women for all fractures and for osteoporotic fractures, but not for hip fracture. Low BMD accounted for only 23% of the smoking-related risk of hip fracture (Kanis et al, 2005). 5.3 Exercise Physical activity is movement that involves movement as housework, gardening, walking, and climbing stairs. Exercise is a specific form of physical activity which is planned, purposeful physical activity performed with the intention of acquiring fitness or other health benefits. Bone marrow density depends on the level of physical activity, in particular, immobilization induces marked loss of skeletal tissue, for example in an immobilized limb or during prolonged bed rest (Kiratli BJ, 2001). Forty-three RCTs with 4320 participants included in mata analysis to evaluate role of exercise for preventing and treating osteoporosis in postmenopausal women. The most effective type of exercise intervention on bone mineral density for the neck of femur appears to be non-weight bearing high force exercise such as progressive resistance strength training for the lower limbs (MD 1.03; 95% confidence interval (CI) 0.24 to 1.82). The most effective intervention for BMD at the spine was combination exercise program (MD 3.22; 95% CI 1.80 to 4.64) compared with control groups (Howe et al, 2011). Evidence based on per-protocol analyses of individual trials in children and adolescents indicated that programs incorporating regular weight-bearing exercise can result in 1% to 8% improvements in bone strength at the loaded skeletal sites. In premenopausal women with high exercise compliance, improvements ranging from 0.5% to 2.5% have been reported. It was found a small and significant exercise effect among pre- and early pubertal boys [SMD, effect size, 0.17 (95% CI, 0.02-0.32)], but not among pubertal girls [-0.01 (-0.18 to 0.17)], adolescent boys [0.10 (-0.75 to 0.95)], adolescent girls [0.21 (-0.53 to 0.97)], premenopausal women [0.00 (-0.43 to 0.44)] or postmenopausal women [0.00 (-0.15 to 0.15)] (Riku Nikander et al, 2010). These considerations suggest that there is as yet no compelling evidence for the efficacy of exercise program in fracture prevention. Notwithstanding, there is good evidence that the Samia A, Hejar A. R., Suriani I, Emilia Z.A. 33 IJPHCS Open Access: e-Journal International Journal of Public Health and Clinical Sciences e-ISSN : 2289-7577. Vol. 4:No. 1 January/February 2017 avoidance of immobilization wherever possible is a valuable adjunct to a global program for osteoporosis. In addition, regular physical activity is associated with improved health and reduced mortality generally (Lee et al, 1995). Thus, exercise can be encouraged but cannot be depended upon to reduce the fracture burden in the community. 5.4 Falls Falls are often the cause of hip fracture, which may result in death, morbidity, and admission to a nursing home. Muscle strength, in particular lower extremity, should be one of the factors assessed and treated in older persons at risk for falls (Moreland et al, 2004). Some stress upon a fragile bone is generally required to precipitate a fracture. Although fragility fractures may be defined as resulting from minimal trauma, this is merely a convention to make the distinction from severe trauma (e.g. road traffic accidents) capable of breaking any bone, including an osteoporotic bone. In many cases, particularly with hip and wrist fractures, a fall from a standing height is involved and the forces involved may be substantial (Bouxsein ML, 2001). A study shown, both active and inactive ambulatory elderly subjects, there was a strong improvement in lower extremity function based on walking speed and sit-to-stand speed, in serum 25(OH) D levels (Moreland et al, 2004). In a meta-analysis vitamin supplementation appeared to reduce falls by 20%, and furthermore if 15 patients were treated with vitamin D, 1 fall could be prevented (Bischoff et al, 2004). 6.0 Population-based prevention Osteoporotic patients are likely to get fragility fractures if left untreated (Stovall, 2013). A balanced diet that contains an abundance of fruits, vegetables, protein sources but no cola beverages has shown to support bone status. Sufficient calcium and vitamin D supplements have shown to decrease the risk of fractures. Exercise is a safe way to prevent bone loss (Tucker, 2009). Bone mass and rates of bone loss are continuously distributed throughout the population, so it is not possible to distinguish precisely an individual with disease from the normal population. All of the previously mentioned high risk population for osteoporosis should be aware. Thus, research should be done to identify the high risk population and assess knowledge, practice, and attitudes about osteoporosis. But there are several problems with these approaches. The first is that not all these risk factors are necessarily causally related to osteoporosis; in particular, uncertainties exist with respect to smoking and moderate alcohol consumption. A second problem relates to the ability to change a lifestyle habit, as illustrated by the limited success of risk factor intervention in coronary heart disease (Ebrahim S, 1997). This raises a third problem, namely that the value and feasibility of population program in osteoporosis prevention have not been coherently evaluated. This consideration even applies to falls, where intuition indicates that attempts to prevent falls in elderly people might be of benefit in reducing fractures. There is, however, currently no controlled trial evidence showing that strategies which prevent falls serve to decrease the risk of fracture in individuals (Chang et al, 2004). Samia A, Hejar A. R., Suriani I, Emilia Z.A. 34 IJPHCS International Journal of Public Health and Clinical Sciences e-ISSN : 2289-7577. Vol. 4:No. 1 January/February 2017 Open Access: e-Journal A further problem relates to the effect of remedial factors on the frequency of fractures within a community. Despite the high prevalence of many of these factors, the increase in risk associated with each is relatively small, as is the attributable risk. Where the attributable risk is small, the same overall reduction in hip fracture incidence might be achieved by targeting that segment of the population with the risk factor itself rather than the whole population. If all the risk factors identified for hip fracture were causal and could be reversed, the impact on fracture incidence might be as high as 50% (Marks R, 2010). In practice, it is not feasible to modify the majority of these risk factors, so the potential effect of risk factor modification at the population level is substantially smaller. 7.0 Recommended strategies Population-based strategies are, therefore, the only practicable preventive measure. They can also be advocated as a component of the adequate care of osteoporosis, even where high risk strategies are applied. Health promotional program could be applied to national campaigns to improve bone health and can be disseminated through social campaigns, school education and health education by health professionals. Refer to Table 3 for an overview of recommended health promotional strategies for specific target groups in Malaysia. One of the most important initiatives for minimizing the burden of osteoporosis related fractures is to identify people who have sustained a minimal trauma fracture early and initiate appropriate treatments. Table 3: An overview of heath promotional strategies for osteoporosis in Malaysia Target group Older/ elderly people Key message Vitamin D and calcium intake Avoidance of smoking and alcohol intake Falls prevention Adequate sun exposure. Pregnant women and their child in utero Children and adolescents A balanced diet, high in calcium and vitamin D, during pregnancy can promote healthy bone formation for the child in utero. Healthy bone habits including a wellbalanced diet, calcium intake, vitamin D and skeletal loading are important during growth to reach a high peak bone Recommended health promotional approach Mass media: television and radio campaigns Run healthy lifestyle programs ie. exercise, falls prevention It is important to be informed about osteoporosis and discuss investigation and treatment options with a health care professional in primary health care clinic. Encourage GPs to discuss bone health with patients who are pregnant during antenatal visit Raising awareness of importance of nutrition during pregnancy for bone health amongst health professionals. Greater emphasis on bone health in health and sport curriculum Provide education to parents on how to promote their children’s bone health Educate physical education teachers Promotion of high calcium foods through school canteens Samia A, Hejar A. R., Suriani I, Emilia Z.A. 35 IJPHCS International Journal of Public Health and Clinical Sciences e-ISSN : 2289-7577. Vol. 4:No. 1 January/February 2017 Open Access: e-Journal Middle age and post menopausal women Men mass. Rapid bone loss occurs in the years following menopause and it is a common time for women to develop osteoporosis. The Osteoporosis SelfAssessment Tool is a simple way to assess risk. Men can develop osteoporosis and it is often underdiagnosed and undertreated, more so than in women. Pre menopausal female athletes People taking certain medications or treatments People with co-morbid conditions Female athletes are at risk of developing amenorrhea which can affect the ability to maintain bone mass. People undergoing chemotherapy and long term users of glucocorticoid therapies are at increased risk and should discuss prevention/treatment options with a health care professional. Certain conditions or diseases can increase the risk of developing osteoporosis, sometimes earlier in life. Television, web-based and radio campaigns, Online forums – Facebook, Twitter Displays, presentations or information sharing at: Women’s Gyms Beauty Therapists, Coffee Shops, Public toilets, Bus/train Mass media - television and radio campaigns or talk back radio Encouraging GPs and Pharmacists to discuss bone health with patients at risk of developing osteoporosis. Displays, presentations or information sharing at: Gyms, sports clubs/events, Bus/train stations, public toilets Mass media as television and radio campaigns or talk back radio Encouraging GPs and Pharmacists to discuss bone health with patients at risk of developing osteoporosis. Advertisements at sporting events Mass media - television and radio campaigns or talk back radio Raising awareness of the risks amongst sporting health professionals. Education for pharmacists to highlight risks. Education for GPs to highlight risks. Educate public about the risks Education of relevant health professionals regarding risks Education for GPs to highlight risks. Educate public about the risks Education of relevant health professionals regarding risks 8.0 Conclusion Osteoporosis takes many years of slow and insidious imbalance between osteoblastic bone deposition and osteoclastic bone resorbing which is the real risk of morbidity associated with fracture. The concept of skeletal health for all age groups has been neglected. There is also lack of driving force and support to promote bone health. There is still a lack of awareness Samia A, Hejar A. R., Suriani I, Emilia Z.A. 36 IJPHCS Open Access: e-Journal International Journal of Public Health and Clinical Sciences e-ISSN : 2289-7577. Vol. 4:No. 1 January/February 2017 among health care providers Preventive measure should be taken in Malaysia to prevent this incipient epidemic. Efforts should be made to raise awareness about osteoporosis as a serious and debilitating disease, increase the priority of osteoporosis at national health policy planning, consider osteoporosis on the list of chronic & disabling diseases, define essential care levels at a national level, define future strategies, projects and plan to fight osteoporosis, to reduce the incidence of osteoporosis related fractures. Programs on prevention, identification of high-risk individuals, and early diagnosis, and treatment intervention, prevention of falls, rehabilitation program for patients with fracture should be designed for Malaysians as well as tackling vitamin D insufficiency. Efforts to create a national osteoporosis and osteoporosis related fracture database should be a top priority. Declaration The authors declare that there is no conflict of interest regarding publication of this article. Authors declare that this paper is our original work, quotations and citations have been duly referenced. Also, this paper has not been submitted previously or concurrently for any other publication. References Barzanji AT, Alamri FA, and Mohamed AG,(2013), Osteoporosis: a study of knowledge, attitude and practice among adults in Riyadh, Saudi Arabia, Journal of Community Health, 38(6): 98-105. Bischoff HA, Stahelin HB, Dick W, et al. (2003), Effects of vitamin D and calcium supplementation on falls: a randomized controlled trial. Journal of Bone Mineral Research, 18:343–51. Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, et al. (2004), Effect of Vitamin D on falls: a meta-analysis, Journal of the American Medical Association; 291(16). Bouxsein ML, (2001), Biomechanics of age-related fractures. In: Marcus R, Feldman D, Kelsey J, eds. Osteoporosis, 2nd ed. Vol. 1. San Diego, CA, Academic Press, 2001:509– 531. Chang JT et al, (2004), Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomized clinical trials, British Medical Journal, 328:680– 683. Chapuy MC, Arlot ME, Duboeuf F, Brun J, Crouzet B, Arnaud S, Delmas PD, Meunier PJ,(1992), Vitamin D3 and calcium to prevent hip fractures in the elderly women, The New England Journal of Medicine, 327(23):1637-42 Clinical Practice Guideline 2012, Malaysian Osteoporosis Society. Retrieved from http://www.moh.gov.my/attachments/7513.pdf on 14th October, 2016. Samia A, Hejar A. R., Suriani I, Emilia Z.A. 37 IJPHCS Open Access: e-Journal International Journal of Public Health and Clinical Sciences e-ISSN : 2289-7577. Vol. 4:No. 1 January/February 2017 Cooper C, Campion G, Melton L J, (1992), Hip fractures in the elderly: a world-wide projection, Osteoporosis International, 2: 285–289 Cumming RG, Nevitt MC, (1997), Calcium for prevention of osteoporotic fractures in postmenopausal women, Journal of Bone and Mineral research, 12(9):1321-9. Damodaran P, Subramaniam R, Omar SZ, Nadkarni P, Paramsothy M, (2000), Profile of a menopause clinic in an urban population in Malaysia, Singapore medical journal, 41, 431–435. De Martinis M, Di Benedetto MC, Mengoli LP, Ginaldi L, (2006), Senile osteoporosis: Is it an immune-mediated disease? Inflammation Research, 55:399-404. Dontas I.A and CK Yiannakopoulos, (2007), Risk factors and prevention of osteoporosisrelated fractures, Journal of Musculoskeletal Neuronal Interact, 7(3): 268-72. Ebrahim S, Smith GD, (1997), Systematic review of randomized controlled trials of multiple risk factor interventions for preventing coronary heart disease, British Medical Journal, 314:1666–1674. Ginaldi L, Di Benedetto MC, De Martinis M, (2005), Osteoporosis, inflammation and ageing, Immunity & Ageing, 2: 14. Gullberg B, Johnell O, Kanis JA, (1997), World-wide projections for hip fracture, Osteoporosis International,7:407-413. Howe TE, Shea B, Dawson LJ, Downie F, Murray A, Ross C, Harbour RT, Caldwell LM, Creed G, (2011), Exercise for preventing and treating osteoporosis in postmenopausal women, Cochrane Database of Systematic Reviews, Issue 7 Johnell O and Kanis JA, (2006), An estimate of the worldwide prevalence and disability associated with osteoporotic fractures, Osteoporosis International 17:1726. Kanis JA, (2007) WHO Technical Report, University of Sheffield, UK: 66. Retrieved from https://www.shef.ac.uk/FRAX/pdfs/WHO_Technical_Report.pdf on 14th October, 2016 Kanis JA, Johnell O, Oden A, et al. (2000) Long-term risk of osteoporotic fracture in Malmo. Osteoporosis International, 11:669. Kanis JA, Johnell O, Oden A, Johansson H, De Laet C, Eisman JA, Fujiwara S, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A,(2005), Smoking and fracture risk: a meta-analysis, Osteoporosis International,16(2):155-62. Kanis JA, Oden A, McCloskey EV, Johansson H, Wahl DA, Cooper CA, (2012), systematic review of hip fracture incidence and probability of fracture worldwide, Osteoporosis International, 23, 2239–2256. Karim HA, (1997), The elderly in Malaysia: demographic trends, Medical journal of Malaysia, 52: 206-12. Kim J, Lee E, Kim S, Lee TJ,(2015), Economic burden of osteoporotic fracture of the elderly in South Korea:A national survey. Value in Health Regional Issues, 9C (2016) 36 – 41 Samia A, Hejar A. R., Suriani I, Emilia Z.A. 38 IJPHCS Open Access: e-Journal International Journal of Public Health and Clinical Sciences e-ISSN : 2289-7577. Vol. 4:No. 1 January/February 2017 Kiratli BJ, (2001), Immobilization osteopenia. In: Marcus R, Feldman D, Kelsey J, eds. Osteoporosis, 2nd ed. Vol. 2. San Diego, CA, Academic Press, 2001:207–227. Lau EM, Lee JK, Suriwongpaisal P, Saw SM, Das De S, Khir A and Sambrook P,(2001), The incidence of hip fracture in four Asian countries: the Asian Osteoporosis Study (AOS). Osteoporosis International, 12, 239-243. Law MR, Hackshaw AK, (1997), A meta-analysis of cigarette smoking, bone mineral density and risk of hip fracture: recognition of a major effect, British Medical Journal, 315:841– 846. LeBoff MS, Kohlmeier L, Hurwitz S, Franklin J, Wright J, Glowacki J,(1999), Occult vitamin D deficiency in postmenopausal US women with acute hip fracture, The Journal of the American Medical Association, 281(16):1505-11. Lee IM, Hsieh CC, Paffenbarger RS (1995), Exercise intensity and longevity in men: the Harvard Alumni Health Study, Journal of the American Medical Association,273:1179– 1184. Lee JK, Khir ASM, (2007), The incidence of hip fracture in Malaysians above 50 years of age: Variation in different ethnic groups, Asia Pacific League of Associations for Rheumatology (APLAR), International Journal of Rheumatic Diseases, 10, 300–305. Lim PS, Ong FB, Adeeb N, Seri SS, Noor Aini et al.(2005), Bone health in urban midlife Malaysian women: risk factors and prevention, Osteoporosis International, 16: 2069-79. Lorentzon M, Mellstrom D, Haug E, Ohlsson C,(2006), Smoking in young men is associated with lower bone mineral density and reduced cortical thickness, Journal of Endocrinology and Metabolism, 92(2): 497-503. Marks, R. (2010). Hip fracture epidemiological trends, outcomes, and risk factors, 1970– 2009. International Journal of General Medicine, 3: 1–17. Moreland JD, Richardson JA, Goldsmith CH, Clase CM, (2004), Muscle weakness and falls in older adults: a systematic review and meta-analysis. Journal of American Geriatric Society; 52:1121–1129. NIH Consensus development panel on osteoporosis prevention, diagnosis and therapy (2001), The Journal of the American Medical Association, 285(6):785–795. Riku Nikander, Harri Sievänen, Ari Heinonen, Robin M Daly, Kirsti Uusi-Rasi and Pekka Kannus, (2010), Targeted exercise against osteoporosis: A systematic review and metaanalysis for optimizing bone strength throughout life, BMC Medicine, 8:47 Sadat-Ali M, Al-Dakheel, DA, Azam MQ, Al-Bluwi MT, Al-Farhan MF,AlAmer HA, AlMeer Z,Al-Mohimeed A,Tabash IK, Karry MO et al.(2015), Reassessment of osteoporosis-related femoral fractures and economic burden in Saudi Arabia. Achieve Osteoporosis. 10, 37. Stovall DW,(2013), Osteoporosis diagnosis and management, In John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK.13-23. Samia A, Hejar A. R., Suriani I, Emilia Z.A. 39 IJPHCS Open Access: e-Journal International Journal of Public Health and Clinical Sciences e-ISSN : 2289-7577. Vol. 4:No. 1 January/February 2017 Tang BM, Eslick GD, Nowson C, Smith C, Bensoussan A, (2007),Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: a meta-analysis, The Lancet, 370(9588):657-66 Tucker KL, (2009), Osteoporosis prevention and nutrition, Current Osteoporosis Report, 7(4):111-7. U.S. Department of Health and Human Services, (2004), Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Office of the Surgeon General. World Health Organization (WHO), Prevention and management of osteoporosis (2003), Report of a WHO scientific group, WHO Technical Report Series, 921. Geneva. Retrieved from http://apps.who.int/iris/bitstream/10665/42841/1/WHO_TRS_921.pdf, on 19th October, 2016. Samia A, Hejar A. R., Suriani I, Emilia Z.A. 40