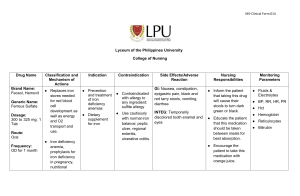
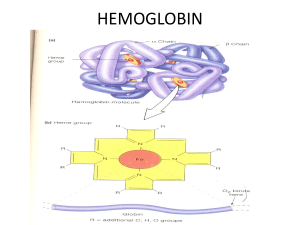
ANEMIA 2021-2022 Professor Doctor Ahmed K Yassin Elmeshhedany Internist & Clinical Hematologist MBChB , DM, CABM, FIBMS(Clinical Hematology.) FRCP(London) Hawler Medical University College of Medicine Department of Medicine Objectives • What is pallor • Etiology • Assessing seriousness • Managements • Paleness (pallor in Latin) is abnormal loss of color from normal skin or mucous membranes due to reduced amount of the blood in the skin arteries. • Note: Due to issues in the blood or the vessels (e.g., vasoconstriction) Paleness should be distinguished from other causes of prominent white skin: • Fair skin. • Myxedema • Albinism • Vitiligo Paleness does not always mean you are ill. • Low environmental temperature • Skipped meal • Dehydration • Exertion or fear Sudden pallness caused by many medical conditions • Motion sickness • Orthostatic hypotension • Fainting (vasovagal syncope) • Dehydration • Stomach upset • Acute infection (usually with fever) • • • • • • Allergy to drugs Rapid stomach emptying (dumping syndrome) Migraine Heat stroke Hypothermia Heart failure due to heart attack, arrhythmia, infective endocarditis or other heart disorder, when the heart can not efficiently pump the blood into the circulation • Low blood sugar (hypoglycemia), common in insulindependent diabetics after an exercise, skipped meal or insulin overdose • Blood loss due to external or internal bleeding (in car accidents, shooting or stitch injuries), heavy menstrual bleeding, surgery • Shock – a sudden, deep fall of blood pressure – due to poisoning, severe infection, burns, severe blood loss • Side effect of medications: – warfarin, corticosteroids, aspirin and other anti-rheumatic drugs may cause intestinal bleeding – iron poisoning • Drug overdose: amphetamine (speed), cocaine • Chemical poisoning (pesticides), plant poisoning (Atropa belladonna) • Death Lecture outlines • What is anemia • Acute anemia, chronic anemia. • What is effects of anemia on organs ( skin, heart, brain, bowel, kidneys,etc) • What is the effects of anemia on patient and age groups ( child, adult, heart problem, neuopsychiatric problem, etc) Case 1 • M is 2 years old boy referred to you because of pallor, jaundice, hepatosplenomegally Case 2 • S is 23 years old girl with recent history of progressive pallor, • On history she has joint pain and fever. • Examination showed jaundice, hepatosplenomegally. Case 3 • J is 65 years old male with history of progressive exertional dyspnea • Examination showed pallor • No organomegally Case 4 • S& I are 22 years old young couple planning for marriage • They asked your opinion as accidently the laboratory evaluation is showing abnormal indices. Etiology of anemia • Blood loss • Underproduction • Decrease red cell survival (note: instead of the usual 120 days, it’s lower, and the bone marrow cannot compensate) • Sequestration The most common worldwide Pallor and chronic blood loss (Iron deficiency anemia) A source of blood loss should be determined. This can be simple, such as menorrhagia, epistaxis, hemorrhoids, PUD, etc. or very grave, e.g., malignancy of the GI tract. Hence, these serious causes should not be missed for a simple cause. In iron deficiency, the treatment is not an issue, but determining the etiology is a matter of importance. Case 1 • You received 65 years old male with hypochromic microcytic anemia and low serum ferritin • Whats your DDX • How you manage this case • What therapy will you use, and why Notes on case 1 • In such a case with this age, even if not anemic but with low serum ferritin (always means iron deficiency; A reduced ferritin is the most reliable initial marker to diagnose iron deficiency without anemia), the first thing you should consider is malignancy. • Other causes may include: • Malnutrition; with a lot of modifications made to the diet of a person as they get older for health concerns and teeth hygiene, iron deficiency with malnutrition can occur. • Malabsorption, e.g., due to PPI abuse. Case 2 • You received 17 years old girl with hypochromic microcytic anemia and low serum ferritin • Whats your DDX • How you manage this case • What therapy you will use, why Prevalence of IDA: • Iron Deficiency Anaemia is the most common form of anaemia, with an estimated > 500 million people affected worldwide. • It is more common in developing countries like ours. • It is frequently encountered in Erbil area. Iron absorption: • Normal mixed diet contains about 10-20 mg of iron /day. This present in inorganic or organic forms. • Dietary sources include: meats especially liver and kidney, egg yolk, some green vegetables like Peas, lentil and beans. Milk has low iron content generally. • Usually only 5-10% of ingested iron is absorbed. • After ingestion of iron containing foods, Iron is released from protein complexes by acid and proteolytic enzymes in stomach and SI, and then is maximally absorbed in duodenum and less so the (note: upper) Jejunum. • Note: iron absorption is increased when there is iron deficiency or when there is increased demand for iron; when the iron levels are low or there is increased demand on iron for cellular processes, the production of hepcidin (negative regulator of iron absorption) is decreased to allow iron to enter the plasma to meet iron demand[1]. (note: ferric, ferrous) Note: A careful history of diet is thus important Note (extra): iron status and absorption • At physiological pH, iron exists in the oxidized, ferric (Fe3+) state. To be absorbed, iron must be in the ferrous (Fe2+) state or bound by a protein such as heme. The low pH of gastric acid in the proximal duodenum allows a ferric reductase enzyme, duodenal cytochrome B (Dcytb), on the brush border of the enterocytes to convert the insoluble ferric (Fe3+) to absorbable ferrous (Fe2+) ions Distribution of Body Iron Plasma (transferrin) (~0.1%) Myoglobin (~10%) Storage iron (~25%) Hemoglobin (~65%) Causes of Iron Deficiency: • Blood loss: Most common cause in developed countries; Most likely from the gastrointestinal tract (hookworm infestation, Duodenal ulcer, Ca stomach or colon, Crohn's, ulcerative colitis, hemorrhoids, salicylates). In females, bleeding from genital tract is also quite common. • Blood loss could be from simple or very serious causes • Nutritional: Quite common cause of Iron deficiency in developing and underdeveloped countries, especially if inadequate intake is coupled with increased demand (e.g., infancy and pregnancy and adolescence). • Inadequate absorption: Malabsorption syndromes e.g. Celiac disease. Body Iron distribution Hemoglobin ~65% Blood loss Iron Def. Anaemia. Clinical Findings: • Clinical features related to underlying pathology, if any. • Early stages: no significant findings (note: They may present because they look pale or depressed to family members) • As anemia progresses: 1. Signs and Symptoms of anemia: Pallor, Fatigue, decrease exercise capacity, shortness of breath. 2. Mucosal changes in severe IDA: • Glossitis: smooth red tongue • koilonychia 3. PICA (craving to eat unusual substances like dirt, clay, ice, salt, hair or cardboard). 4. No Organomegaly Glossitis Koilonychia (Spooning of the nails) Note: When you see a pale hand on clinical examination, your next step is to check the nails for koilonychia, evidence of chronic liver disease, and ask about paresthesia. Blood Picture in IDA: 1. Hemoglobin: reduced • PCV: reduced. • MCH, MCV, MCHC all reduced. 2. Leucocytes and platelets usually normal. 3. Red cells on film: Hypochromic, microcytic. 4. Bone marrow aspirate: Non-specific changes. Depleted Iron stores on Staining the marrow with a stain for iron (Diagnostic). (note: rarely needed[1]) Blood Film findings in IDA: Normochromic, normocytic NORMAL IDA Hypochromic, Microcytic Diagnosis of IDA: 1. Hematological findings 2. Serum Iron and TIBC: • Serum Iron reduced. • Total Iron binding capacity increased • S. Iron/TIBC: Transferrin saturation reduced (< 15%). 3. S. Ferritin (< 15ug/L) • Note: low serum ferritin is diagnostic of iron deficiency[1] • Note: the most sensitive laboratory test for IDA, however, serum ferritin can be elevated in inflammation (i.e., it’s an acute phase reactant), and so is not always a reliable test of iron status if it is within normal limits. Thus, when obtaining a serum ferritin level, the patient should ideally be free of any infection or disease process, which might lead to increased inflammation or an immunological response. Therefore, a low serum ferritin is meaningful for ID, but a normal ferritin is less meaningful and may be reflective of inflammation[1]. 4. Bone marrow Iron: as determined by Prussian blue stain for marrow Iron is depleted. (Diagnostic). Iron stain on marrow Iron is represented by blue granules Normal Marrow Normal storage Iron (note: diagnostic) Iron deficient marrow Absent storage iron Management of IDA: 1. Check and exclude causes of Iron deficiency especially pathological blood loss (note: it’s VERY IMPORTANT to determine a cause before you start treating IDA) 2. In adults, iron deficiency equal blood loss unless proved otherwise 3. Oral Iron therapy: treatment of choice (note: Iron pills can change the color of stool to a greenish or grayish black. The patient should be warned) 4. Parenteral Iron: is only indicated if there is malabsorption or intolerance to oral iron (note: parenteral iron can have serious adverse effects) * * e.g., continued menorrhagia, hemorrhoids, etc. Differential diagnosis of IDA (from other causes of hypochromic Anaemia: 1. Thalassemia: Clinical features, Iron studies, Hb electrophoresis. 2. Sideroblastic Anaemia: Clinical features, Iron studies, bone marrow, iron stain. 3. Lead poisoning: History, Iron studies, blood film, urine lead. 4. Anemia of Chronic disorders: History, Iron studies. Anaemia of chronic disorders (note: iron malutilization): • A hematological syndrome that accompanies certain nonhematological diseases and is mild to moderate anemia, variable hypochromia, and hypoferremia despite adequate iron stores. • Anaemia is usually normochromic normocytic, but sometimes hypochromic. • Severity of anemia is often related to the severity of the underlying disease. • Note – laboratory findings: • MCV is normal or decreased • Serum iron is low • TIBC is low or normal • Transferrin saturation is normal or decreased • Serum ferritin is high or normal Causes of Anemia of chronic disorders 1. Chronic infections: - like T.B., osteomyelitis, chronic abscess, SBE. 2. Chronic inflammatory disorders: - like Rheumatoid arthritis, SLE, PAN, etc. 3. Non-hematological malignancy. 4. Chronic Renal failure. Note: The treatment is to treat the underlying condition. CONCLUSION • IRON DEFICIENCY IS COMMONEST TYPE OF ANEMIA • BLOOD LOSS MUST BE EXCLUDED • ORAL IRON IS BEST Pallor & jaundice (Haemolytic anemias) Case 1 • You are asked to see 15 years old boy with pallor and jaundice with positive family history (i.e., congenital disease) • What is your DDx • How you can diagnose HS Note: Thalassemia major usually presents before 2 years. Hereditary spherocytosis can present at any age from the neonatal period to the ninth decade, depending on severity. Case 2 • You received 4 years old boy with 1 day history of severe pallor, jaundice and black urine • He has no organomegally but severe tachycardia and hypotension • How you manage such patient • What is your diagnosis • Favism Case 3 • MRs H is 35 years old lady with history of SLE on therapy, recently she developed increasing pallor • What is your DDx • Note: Could be due to autoimmune hemolysis, menstrual bleeding, druginduced, anemia of chronic disease, etc. • How you can confirm the diagnosis Objectives • What is hemolytic anemia • Causes • Types • Management Definition of Hemolytic anemia • Note: In a healthy individual about 1% of the circulating erythrocytes are being destroyed (removed) daily due to senescence and new blood corpuscles are produced by bone marrow. • Note: With decreased survival/increased destruction, the bone marrow increases production of RBCs to compensate. The bone marrow can usually increase RBC production 6-8 fold to keep pace with cell breakdown, thus giving a compensated hemolytic anemia[1]. Anemia results when bone marrow production can no longer compensate for the shortened RBC survival; this condition is termed uncompensated hemolytic anemia. • Anemia resulting from an increased rate of red cell destruction (decreased red cell survival) • Note: can be immune or nonimmune; acquired or congenital Destruction may be predominantly: 1. Extra-vascular 2. Intra-vascular General evidence of hemolysis: • 1. Evidence of RBC and Hb breakdown: - Increased unconjugated (Indirect) Bilirubin (note: may cause jaundice) - Increased urinary Urobilinogen. - Increased Stool Sterecobilinogen. - Absent Hb binding protein (Haptaglobin). • 2. Evidence of increased red cell production: - Reticulocytosis (An elevation in the number of reticulocytes – immature RBCs) – blood. (healthy marrow) (note: normal range is 0.5-1.5%) - Erythroid hyperplasia – marrow. General evidence of hemolysis (Cont.): •3. Evidence of RBC Damage: - Spherocytes, fragmented red cells. -Special tests: red cells survival studies. •4. If intravascular hemolysis: - Hemoglobinuria. - Hemoglobinaemia. - Hemosidrinuria (if prolonged). Classification of Hemolytic anemia Could be broadly classified into: • Inherited Hemolytic anemias. • Acquired Hemolytic anemias. Causes of inherited Hemolytic anemia: 1. Enzymopathies: • G6PD deficiency. • Pyruvate kinase deficiency. 2. Membrane defect: • Hereditary spherocytosis. • Hereditary Ovalocytosis. 3. Haemoglobinopathies: • Thalassaemias: quantitative Hbpathies. • Qualitative Hbpathies: Hb S, C, D, E etc. Inherited Hemolytic Anemia Due to RBC enzyme defects 1. G6PD Deficiency. 2. Pyruvate Kinase Deficiency. 3. Others (very rare). Glucose 6 Phosphate Dehydrogenase Deficiency (G6PD Deficiency) Definition of G6PD Deficiency • Sex-linked inherited disorder (note: i.e., it usually affects males) • Characterized usually by acute hemolytic episodes following exposure to oxidant stress (infection, drugs or fava beans), due to deficiency of RBC enzyme G6PD. G6PD Deficiency • More than 100 million people effected worldwide. • Quite frequent in Iraq with 6-13% of the population affected. • One of the most frequent causes of acute hemolysis in Erbil region, especially during the fava bean season. Favism • Occurs on consumption of Fava beans. • Usually occurs within 24 hours of ingestion. • Most frequent in spring (March-May). • 2/3 of cases occur in 1-6 year old children. • Males predominate. Clinical features of favism • Sudden Pallor • Jaundice. • Red or dark urine (note: cola-colored urine) due to Hemoglobinuria. • Lasts usually for 2-6 days followed by spontaneous recovery. • No organomegaly. Note: G6PD deficiency can cause neonatal jaundice (i.e., present at birth) Hemoglobinuria in favism Note: Patient should be admitted and urine should be examined every day. With removal of the offending agent, the urine gradually recovers. Day Recovering hemoglobinuria 1 2 3 4 5 6 Blood Film in acute hemolytic episode in G6PD deficiency. Blister Cell Other Laboratory tests in favism: • Hemoglobin in urine and plasma. • Increase urine urobilinogen. • Indirect hyperbilirubinemia. • Methemoglobin reduction test For G6PD deficiency (Screening test) • Specific Assay for red cell G6PD Management of G6PD deficiency: • Note: The usual treatment for hemolytic anemia in G6PD-deficient patients is supportive care (e.g., IV fluid) plus removal and avoidance of further triggers. In severe hemolysis, blood transfusions may be required; hemodialysis may be needed if acute kidney injury occurs. • Blood transfusion during the episode may be needed. • Spontaneous recovery. • No Cure. • Patient should avoid Fava beans, certain drugs, e.g. certain antimalarials, sulphonamides, septrin, aspirin, salazopyrine, Nalidixic acid, Nitrofurantoin, Naphthelene (mothballs). • Note: It may be more practical to instruct the patient to tell their physician they have this issue before they get prescribed the medication than give the patient a long expanding list of medications Inherited Hemolytic Anemia Due to Membrane Defects 1.Hereditary Spherocytosis. 2. Hereditary Ovalocytosis (Elliptocytosis) Hereditary Spherocytosis (HS): • Definition: Inherited disorder resulting from an intrinsic defect involving red cell membrane, leading to RBCs which are osmotically fragile and spherocytic in shape. • Usually inherited as Autosomal dominant. • Not common in Iraq. Note: Osmotic fragility test, used in the diagnosis of HS More hypotonic (of hemolysis) Note (extra): osmotic fragility test • The osmotic fragility test (OFT) is used to measure erythrocyte resistance to hemolysis while being exposed to varying levels of dilution of a saline solution. When erythrocytes are exposed to a hypotonic environment, water enters the cell and causes swelling and eventual lysis. The susceptibility of osmotic lysis of erythrocytes is a function of surface area to volume ratio (SAVR) • Osmotic fragility of RBCs is defined as the ease with which the cells burst in hypotonic solutions and is expressed in terms of the concentration of the saline solution in which the cells are hemolyzed. • The classic osmotic fragility test, originally described by Parpart et al (1947), involves a small amount of fresh blood being added to a series of solutions with tonicity ranging from 0.1%-0.9%. Results are then plotted against the NaCl concentrations, yielding an osmotic fragility curve that is then compared to obtained normal control values. • In a disease such as hereditary spherocytosis, erythrocytes have a smaller ratio of surface area to volume and are thus more susceptible to osmotic stress; A spherocyte will burst at higher saline concentrations, as the RBC’s ability to take in water before stretching the surface membrane is thus more limited than normal, and it is, therefore, particularly susceptible to osmotic lysis. • Thus, in this case, the osmotic fragility curve will shift to the right. That is, the lysis will start at an even lower hypotonic challenge. Management of HS • No Cure. • Aim is to minimize consequences of disease. • One of the rare absolutes in Medicine is “TRUE UNCOMPLICATED HS ALWAYS RESPONDS TO SPLENECTOMY”. • Note: Splenectomy corrects the anemia and normalizes (increases) the RBC survival in patients with HS, but the morphological abnormalities persist. • Note: In general, splenectomy is not indicated in patients with mild HS. Indications include (symptomatic) anemia and complications such as gall bladder stones. • All should receive folate supplements. Autoimmune HA • Dropping hemoglobin level • Evidence of hemolysis • Evidence of autoimmunity (note: e.g., Direct Coomb’s test positive, which detects antibody or complement on human RBC membranes.) • Can be primary (note: no underlying etiology demonstrated; approximately 50% of cases[1]) or secondary Secondary AIHA • Autoimmune diseases • Lymphoproliferative diseases (LPD) (note: e.g., Non-Hodgkin’s lymphoma) • Cancer (note: e.g., thymoma, ovarian Ca, prostate Ca) • Infections • Drugs Note:[1] • Antibiotics (cephalosporins, beta-lactamase inhibitors, cotrimoxazole) • Antiviral drugs: HAART • Anti-PD-1 monoclonal antibodies (nivolumab, pembrolizumab) • Chemotherapy (carboplatin, oxaliplatin) • Non-steroidal anti-inflammatory drugs (diclofenac) • Others: methyldopa Treatment of AIHA • If Hb less than 10gm/dL • Start prednisolone 1mg/kg • When Hb >10gm/dL, start tapering • If no response, intolerance, contraindication, non-compliance, do splenectomy • Note: other immunomodulatory agents (e.g., rituximab, IVIG, cyclophosphamide, etc.) may be tried before a splenectomy conclusion • • • • Hemolytic anemia are of diverse etiology Indirect hyperbilirubinemia, reticulocytosis Hemolysis can be life threatening sometimes Folate supplementation is crucial. Questions? • How you can differentiate hereditary spherocytosis from immune hemolytic anemia MEGALOBLASTIC ANEMIA Hawler Medical University College of Medicine Department: MEDICINE OBJECTIVES • REVIEW PREVIOUS LECTURE • WHAT IS MEGALOBLASTIC ANEMIA • PATHOPHYSIOLOGY • CAUSES • MANEGEMENT MEGALOBLASTIC ANEMIA Definition • Note: a metabolic anemia • Anemias characterized by distinctive cytological and functional abnormalities in blood and marrow due to impaired DNA synthesis (note: can affect all proliferating cells) • It maybe due to: – Vitamin B12 (cobalamin) deficiency – Folate deficiency – Or interference with DNA synthesis by other mechanisms ; relatively heat-stable Summary of Absorption of B12 Duodenum STOMACH Vit B12 R-binder Intrinsic Factor CELLS of the Body Trancobalamin II od stream Blood stream TCII absorbed Cells of ileum This reaction is extremely important for normal Synthesis of DNA This reaction is important for normal myelination of neurons. Blood Picture in Megaloblastic anaemia Film: Normochromic, Anisocytosis poikilocytosis, macrocytosis, tear drop cells • Variable degree of anaemia, may reach a low of 2-3g/dl. • MCV increased >100 fl, maybe up to 135. • Low retics. • Leucocytes may be reduced, some neutophils maybe hypersegmented. • Platelets may be reduced. Blood Film in Megaloblastic anaemia Hypersegmented Neutrophils Bone marrow findings in Megaloblastic Anaemia • Hypercellular marrow. • Erythroid hyperplasia, with megaloblastic maturation. • Granulopiesis: Giant forms seen. • Abnormal megakaryocyte nuclear segmentation. Megaloblasts versus Normoblasts • Megaloblasts are larger. • Show a shift towards more immature precursors. • Nucleo-cytoplasmic maturation dissociation. • Note: As the DNA doesn't synthesize normally, nuclear maturation is delayed, while cytoplasmic maturation continues at normal rate, thus forming a cell with mature cytoplasm with relatively immature, large, open nucleus, known as a megaloblast. Early erythroblasts Megaloblast Normoblast Cobalamin Deficiency Causes of B12 Deficiency Impaired Absorption REDUCED INTAKE - Unusual; Gastric - Pernicious anaemia. - Gasterctomy. INTESTINAL -Ileal resection -Blind loop Syndrome -Crohn’s dis. -Celiac Disease -Strict Vegetarians Pernicious Anaemia • • • • The best known of megaloblastic anaemias due to Cobalamin deficiency. Not common in Iraq. Mostly a disease of the elderly. Characterized by stomach atrophy, loss of intrinsic factor and Hydrochloric acid. Pernicious Anaemia • Mostly autoimmune in nature. • Characterized classically by a combination of Megaloblastic anaemia, Glossitis and Neuropathy (Subacute Combined Degeneration of the Cord/SCDC). Note: A patient just feeling like he’s “getting old” Presentation: • Symptomless in some • Symptoms of anemia • Anorexia. • Weight loss • Diarrhea or constipation • St. Bruising • Infections (impaired Bactericidal function of phagocytes) Pallor with Tinge of Jaundice -All rapidly growing DNA synthesizing tissues are affected. -Gonads are affected and infertility is common. -Recurrent fetal loss. GLOSSITIS Clinical features of cobalamin Deficiency. Neurological Manifestations Begins with Paresthesia in feet and fingers due to early peripheral neuropathy, with disturbance of sense of vibration and proprioception. If untreated, there is progression to spastic ataxia resulting from demyelination of the lateral and posterior columns of spinal cord. Brain maybe affected, with Subacute Combined Degeneration of the Cord TIP: IF not Managed early enough, then changes cannot be reversed by treatment perversion of taste, smell and vision; dementia and psychological disturbances may occur Note: Vitamin B12 deficiency is a cause of reversible dementia that must be ruled out in the evaluation of neurocognitive decline. Folate Deficiency Causes of Folate Deficiency Reduced Intake Frequent in infants and ELDERLY Excess utilization Impaired Absorption Prematurity, pregnancy, lactation, Hemolysis, Malignancy Malabsorption, Celiac dis, Lymphoma, regional enteritis, jejunal resection DRUGS Methotrexate, Anticonvulsants, Hydroxyurea, ARA-c. Clinical features of Folate deficiency • Exactly the same as those of cobalamin Deficiency (B12), except for the absence of neurological manifestations. • The hematological findings on blood picture and bone marrow exam are also indistinguishable. Further Diagnostic evaluation of Megaloblastic anaemias • Serum B12 and folate.(should be done before transfusions or initiating therapy). • Search and exclude causes for B12 and folate, e.g. gastrectomy, crohn’s disease, intake of certain drugs, intestinal surgery, vegetarians, patients with increase folate demands e.g. multiple pregnancy, hemolysis etc. Differential Diagnosis of macrocytic anemia Other than megaloblastic anemia, macrocytosis maybe seen in the following conditions: 1. Infancy (physiological). 2. Alcoholism. 3. Liver disease. 4. Reticulocytosis (following acute blood hemolysis, or hemolysis). 5. Aplastic anemia. 6. Acquired Sideroblastic anemia. 7. Leukemia and pre-leukemia. 8. Myxoedema. Management: In cobalamin deficiency: • Hydroxocobalamin by injection. • Should never give folate on its own in cobalamin deficient because although response will be seen, aggravation or induction of neurological complications may be induced. • Note: B12 given first and if there is no response, folate is started, but don’t start with folate alone if you’re not sure which is deficient [Dr. Ahmad] In folate deficiency: • Folic acid orally • The length of therapy is dependent on the underlying pathology. Assessment of therapy response: • The patient will feel better rapidly after starting therapy. • Reticulocytes will increase within 3-5 days reaching a peak in 7-10 days. • Hb will increase at a rate of 1 g/dl per week. • Leucocytes and platelets will return to normal counts within days. • The marrow will start changing from megaloblastic to normoblastic within 12 hours, and this process will be complete within 2-3 days. Conclusions • Megaloblastic hemopoiesis either due to B12 or folate deficiency • Neurological deficit is a sign of B12 deficiency • B12 only from animal origin Question • How long after gastrectomy a patient can develop B12 deficiency.