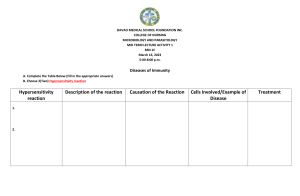
Hypersensitivity Reactions: Types, Mechanisms & Treatment
advertisement

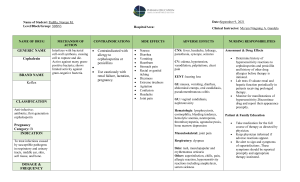
Hypersensitivity Reactions Hypersensitivity Reactions When the immune system "goes wrong" . Immune response should be protective. In this process damage to host occurs. Hypersensitivity denotes a state of increased reactivity of the host to an antigen and implies that the reaction is damaging to the host. The individual must first have become sensitized by previous exposure to the antigen. On second and subsequent exposures, symptoms and signs of a hypersensitivity state occur. Hypersensitivity Reactions Immediate hypersensitivity refers to antibody mediated reactions – symptoms develop within minutes to hours Delayed hypersensitivity refers to cell mediated immunity, symptoms not observed for 24 to 48 hours. Four Classifications Type I (Immediate) Hypersensitivity Type II (cytotoxic) hypersensitivity Type III (immune complex mediated) hypersensitivity Type IV (delayed) hypersensitivity Type I (Immediate) Hypersensitivity Distinguishing feature short lag time. Key reactant is IgE Antigens which trigger response called atopic antigens or allergens. Atopy – inherited tendency to immunologically respond to inhaled or ingested allergens with increased IgE production. Type I (Immediate) Hypersensitivity IgE primarily synthesized in lymphoid tissue of respiratory and GI tract. Regulated by T helper cells. Specific interleukins are involved in development of eosinophils and promote development of mast cells. All act to stimulate overproduction of mucus. Basophils and mast cells have highest number of receptors for Fc portion of IgE on surface. Type I (Immediate) Hypersensitivity Reactions range from mild manifestations associated with food allergies to life-threatening anaphylactic shock. Atopic allergies include hay fever, asthma, food allergies and eczema. Exposure to allergens can be through inhalation, absorption from the digestive tract or direct skin contact. Extent of allergic response related to port of entry, i.e., bee sting introduces allergen directly into the circulation. Caused by inappropriate IgE production This antibody has an affinity for mast cells or basophils. Type I (Immediate) Hypersensitivity Type I (Immediate) Hypersensitivity When IgE meets its specific allergen it causes the mast cell to discharge its contents of vasoactive substances into the circulation. This release leads to symptoms of: sneezing, runny noses, red watery eyes and wheezing. Symptoms subside when allergen is gone. The most common immunological abnormality seen in medical practice, estimated that 30% of US population has allergies. Type I (Immediate) Hypersensitivity Anaphylactic shock is the most serious and fortunately the rarest form of this Type I hypersensitivity. Symptoms are directly related to the massive release of vasoactive substances leading to fall in blood pressure, shock, difficulty in breathing and even death. It can be due to the following: Horse gamma globulin given to patients who are sensitized to horse protein. Injection of a drug that is capable of acting as a hapten into a patient who is sensitive, ie, penicillin. Following a wasp or bee sting in highly sensitive individuals. Foods – peanuts, shellfish, etc. Type I (Immediate) Hypersensitivity Anaphylaxis Type I (Immediate) Hypersensitivity Anaphylaxis Type I (Immediate) Hypersensitivity Anaphylaxis Type I (Immediate) Hypersensitivity Treatment Avoidance of known allergens Localized reactions use OTC antihistamines and decongestants. Asthma uses combination – antihistamines, bronchodilators and corticosteroids. Systemic use epinephrine Hyposensitization – inject antigen to cause production of IgG which binds to antigen (allergen) before it reaches IgE coated cells. Monocolonal anti-IgE – inject, binds to receptors on mast cells blocking them from the IgE. Type I (Immediate) Hypersensitivity Epipen Type I (Immediate) Hypersensitivity Testing In-Vivo Tests - Skin tests Small amount of allergen injected into skin Look for wheal formation of 3mm or greater in diameter Simple, inexpensive, can screen for multiple allergens. Stop anti-histamines 24-72 hours before test. Danger of systemic reaction Not for children under 3 Type I (Immediate) Hypersensitivity Doctors sometimes use skin tests to diagnose allergies. Type I (Immediate) Hypersensitivity The reactions shown here demonstrate allergic response. Type I (Immediate) Hypersensitivity In-Vitro Tests Measure total IgE or antigen-specific IgE Less sensitive than skin tests. RIST, RAST, Allergen specific and Microarray will be covered later. Type II (Cytotoxic) Hypersensitivity Triggered by antigens found on cell surfaces Altered self antigens Heteroantigens Manifested by the production of IgG or IgM antibodies which coat the antigens. Mechanisms Antibody coats cell surface promotes phagocytosis – macrophages, neutrophils and eosinophils have Fc receptors to bind to antibody on target cell. Natural Kill cells have Fc receptors, bind, results in cytotoxicity Complement Coats cells which enhances phagocytosis Complement cascade goes to completion results in cell lysis. Type II (Cytotoxic) Hypersensitivity Transfusion reactions Hundreds of different antigens expressed on RBCs Antibodies can be produced naturally or through exposure, transfusion or pregnancy most common Most well known example due to ABO incompatibility. Individuals form potent antibodies against ABO antigens not present on their red blood cells. Group O individuals have anti-A and if transfused with group A blood will have an immediate, and possibly fatal, reaction Other blood groups may cause delayed reaction or acute reactions. Type II (Cytotoxic) Hypersensitivity Hemolytic disease of the fetus and newborn Mother exposed to blood group antigens due to previous pregnancy with antigen positive child or transfusion. Antibody must be IgG Crosses placenta and coats fetal RBCs, destruction of RBCs causes increased bilirubin and anemia. If first pregnancy is first exposure infant usually not affected. Subsequent pregnancies have increased risk and the disease ranges from mild to fatal. All pregnant women are screened for blood group antibodies. Type II (Cytotoxic) Hypersensitivity Autoimmune hemolytic anemia Patients form antibodies to antigens on their on RBCs. Warm antibodies react at 37C Cold antibodies react best in-vitro at 4C and will dissociate at 37C This will be discussed in detail during Immunohematology. Drug induced hemolysis Some drugs may act as haptens, attach to the RBC membrane causing antibodies to be formed. Antibody reacts with drug on RBC causing hemolysis. Type II (Cytotoxic) Hypersensitivity Peripheral Smear Type II (Cytotoxic) Hypersensitivity Tests Coomb’s or anti-human globulin test. Direct Coomb’s Add anti-IgG to washed drop of RBCs If cells are coated with IgG then agglutination will occur. Indirect Coomb’s Incubate patient serum with RBCs of known antigenic make up. Wash and add anti-IgG If patient has antibody against antigen on RBC agglutination will occur. Type II (Cytotoxic) Hypersensitivity Some individuals make antibody which cross reacts with self antigens found in both the lung and kidney. Goodpasture syndrome most well known example Antibody produced against basement membrane protein. This protein present in lungs and kidneys. Antibody binding results in inflammation Symptoms are hemoptysis and hematuria. Others will be discussed later Hashimoto’s disease Myasthenia Gravis Diabetes mellitus Type II (Cytotoxic) Hypersensitivity Type III (immune complex mediated) Hypersensitivity Similar to Type II, IgG or IgM involved and destruction is complement mediated. Difference is that antigen is SOLUBLE. Soluble antigen and antibody combine to form complexes. Usually complexes cause no symptoms, quickly disappear from the circulation. Size of complexes produced seems important in determining whether they will be eliminated quickly from the body or retained long enough to cause damage. In some individuals the immune complexes persist in circulation causing clinical symptoms, some of them serious. Type III (immune complex mediated) Hypersensitivity Mechanism Soluble immune complexes which contain a greater proportion of antigen than antibody penetrate blood vessels and lodge on the basement membrane At the basement membrane site, these complexes activate the complement cascade. During complement activation, certain products of the cascade are produced,`attract neutrophils to the area. Such substances are known as chemotactic substances. Once the polymorphs reach the basement membrane they release their granules, which contain lysosomal enzymes which are damaging to the blood vessel. This total process leads to the condition recognized histologically as vasculitis. Type III (immune complex mediated) Hypersensitivity Type III (immune complex mediated) Hypersensitivity Tissues most frequently affected are: Glomerular basement Vascular endothelium Joint linings Pulmonary alveolar membranes Classical clinical symptoms of immune complex disease are due to blood vessel involvement, i.e., vasculitis. Blood vessels of joints and the kidney are most frequently affected, giving rise to symptoms of arthritis and glomerulonephritis. Type III (immune complex mediated) Hypersensitivity Arthus Reaction Immunized rabbits to antigen Rabbits then injected intradermally with antigen Localized inflammatory reaction occurred followed by hemorrhagic necrotic lesion. Occurred due to immune complexes depositing in dermal blood vessels. Complement, neutrophils and platelets caused toxic affects. Rare in humans. Serum Sickness Due to passive immunization with animal serum, bovine or horse. Vaccines and bee stings may also trigger. Symptoms appear 7 – 21 days after exposure to animal serum. Headache, fever, nausea, vomiting, joint pain, rashes and lymphadenopathy. Symptoms due to antibody being formed at same time antigen is present = immune complexes form. Benign, self limiting, 7-30 days for recovery. Type III (immune complex mediated) Hypersensitivity Chronic immune complex diseases are naturally occurring diseases caused by deposits of immune complex and complement in the tissues. Systemic Lupus Erythematosus (SLE) Acute glomerulonephritis Rheumatic fever Rheumatoid arthritis Type IV (delayed) Hypersensitivity Used to describe the signs and symptoms associated with a cell mediated immune response. Results from reactions involving T lymphocytes. Characteristics of this phenomenon are: Delayed, taking 12 hours to develop. Causes accumulation of lymphs and macrophages. Reaction is not mediated by histamine. Antibodies are not involved in the reaction. Type IV (delayed) Hypersensitivity Most well known is the Koch Phenomenon Inject tuberculoprotein (PPD test) intradermally Reaction results in an area of induration of 5 mm or more in diameter and surrounded by erythema Reaction which occurs within 48 hours is a positive. Type IV (delayed) Hypersensitivity Positive TB Test Type IV (delayed) Hypersensitivity Contact dermatitis due to contact with chemicals Poison ivy, oak and sumac give off urushiol. Nickel, rubber, formaldehyde, hair dyes, comsetics Latex allergies Function as haptens Causes erythema, swelling and formation of papules Hypersensitivity Pneumonitis Response of sensitized T cells to inhaled allergens. Caused by chronic inhalation of microorganisms. Occupationally related – pigeons, farmers Type IV (delayed) Hypersensitivity Type IV (delayed) Hypersensitivity Summary References http://www.thebody.com/nih/immune_system.html http://pathmicro.med.sc.edu/ghaffar/hyper00.htm http://home.kku.ac.th/acamed/kanchana/bsi.html