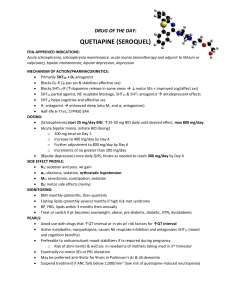
Strength of Research Structured Abstract Limitations of the Research Structured abstract does not include limitations of research. Introductory/ Background Literature review is brief. Research Question Excludes complex patients with dual diagnosis. Selection issues Does not include patients that have dual diagnosis of either bipolar I and anxiety or bipolar I and substance abuse disorder. Strict inclusion criteria The research does not Relevancy to Topic of Interest Abstract accurately and succinctly written. Easy to understand. Explained to the reader why this research on quetiapine filled a gap in the literature and relevant to the care of bipolar I patients. Article has a clear purpose statement that explains the necessity of this research in clinical practice. Notes Summarized the sample, research methods, results, and conclusions. Article explains that a gap exists in current literature regarding second-generation antipsychotics when combined with lithium or divalproex increases the time between relapse events (both depression and mania). Included patient Bipolar 1 patients who problem, were prescribed intervention, a) Lithium + comparison between quetiapine groups and outcomes, b) Lithium + placebo using the PICO c) Divalproex + acronym. quetiapine d) Divalproex + placebo Article clearly explains patient selection to be in the study, how randomization was done once a patient was selected to be in the study, and the occurrence of informed consent. Article focuses on for Bipolar I patients who had achieved 12 to 36 weeks of stability on lithium or divalproex monotherapy. include patients with Bipolar II or cyclothymia. Selection issue Used two identical multicenter doubleblind, placebocontrolled studies that examined combining quetiapine with lithium or divalproex after acute stabilization from a manic episode. There was masking of the treatment/ intervention so that neither the patient or clinician knew whether the patient was receiving quetiapine or placebo. Patients were randomly assigned to a specific treatment arm. Large sample size n=3,414 patients. maintenance after an acute manic phase of the illness. Patients with bipolar I have multiple instances of mood instability that effect quality of life and level of functioning. This article provides evidence regarding the best strategies to prolong times between a relapse with mania or depression. There was no proxy measurement of SES. Gender was identified in binary manner. Patient population included people in different countries. There was a broad racial representation. The results of the study are generalizable to a clinic population in the twin cities. Method validated This method relies assessment tools for heavily on self-report assessing symptoms of of symptoms. mania and/or depression were used to measure time to recurrence of symptoms. Tools to evaluate mood can be incorporated into clinic practice. Relapse was measured by multiple factors. Hospitalization for mania, depression, or a suicide attempt. Additionally, symptoms were assessed with the YMRS or MARDS score > 20 in two consecutive assessments = relapse. As a future PMHNP, knowing the tolerability of a medication and the frequency of side effects is important in clinical practice. Serious adverse events were experienced by 2.9% of patients in quetiapine + lithium and 3.7% of patients on quetiapine + divalproex. Assessments including measuring symptoms and function between mood episodes. Results included safety and tolerability data in addition to answering the primary research question on whether adjunctive quetiapine lengthens the time to symptom relapse in bipolar I patients. Results included efficacy outcome measure with reporting confidence intervals of four groups. Lithium plus quetiapine Lithium plus placebo Divalproex plus lithium and divalproex plus placebo. Tolerability of medication was assessed subjectively and with results of metabolic data. Most studies are not double blinded with placebo controls. The findings of this study have implications to how patients are best treated. Quetiapine combination treatment with either lithium or divalproex extended the time between mood episodes compared to placebo. Quetiapine monotherapy added to lithium or divalproex therapees were both equally effective. Results derived from statistical methods that used appropriate statistical methods of ANOVA to measure change over time. Statistical tools for analysis were the correct tools to analyze data. A Cox proportional hazards model measured time events. Confidence intervals were clearly presented. P values are not the appropriate way to report results using these statistical tests. Results study included biological data in addition to subjective data. Biological data included glucose, lipid levels, weight. Ethical issues Effect sizes were not included in data reported. Changes in clinical practice should occur because of the strength of the research methods. Hgb A1Cs were not collected. Diabetes, fatty liver disease and cardiovascular implications to the physical health of bipolar I patients are important information to understand when prescribing atypical second-generation antipsychotics. Original studies were IRB approved and post-hoc analysis was also approved. An ethical issue is that bipolar I patients with additional disease burden of having cooccurring issues of anxiety or substance use disorder were excluded from the research. A single fasting blood sugar test was higher with quetiapine. Results were ethical. Discussion included critical appraisal of randomized control study. Drop-out rate was explained in the discussion but with a lack of a comparison group to patients not enrolled in a study it is not clear of the patients in this randomized study dropped out of care any more frequently than those not included in the study. Discussion did not over or under report the significance of the research results. Funding was from both industry and non-industry sources I will begin to prescribe quetiapine in addition to lithium or divalproex. Industry funding from Pfizer, AstraZeneca, JDS Pharmaceuticals This study provides data on long-term outcomes of using quetiapine treatment beyond the 12 weeks usually required to bring a medication to market.