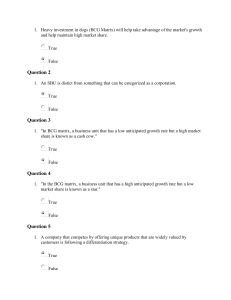
Vaccine 28 (2010) 6265–6272 Contents lists available at ScienceDirect Vaccine journal homepage: www.elsevier.com/locate/vaccine Oral vaccination of badgers (Meles meles) with BCG and protective immunity against endobronchial challenge with Mycobacterium bovis Leigh A.L. Corner a , Eamon Costello b , Damien O’Meara b , Sandrine Lesellier a,e , Frank E. Aldwell c , Mahavir Singh d , R. Glyn Hewinson e , Mark A. Chambers e , Eamonn Gormley a,∗ a School of Agriculture, Food Science & Veterinary Medicine, University College Dublin, Dublin 4, Ireland Central Veterinary Research Laboratory, Backweston, Celbridge, Co. Kildare, Ireland Immune Solutions Ltd., Centre for Innovation, The University of Otago, Dunedin, New Zealand d LIONEX GmbH, Inhoffenstr. 7, 38124 Braunschweig, Germany e TB Research Group, Department of Statutory and Exotic Bacteria, Veterinary Laboratories Agency Weybridge, New Haw, Addlestone, Surrey KT15 3NB, UK b c a r t i c l e i n f o Article history: Received 25 May 2010 Received in revised form 18 June 2010 Accepted 30 June 2010 Available online 15 July 2010 Keywords: Oral BCG Badgers Tuberculosis Vaccine a b s t r a c t Eurasian badgers (Meles meles) are a reservoir host of Mycobacterium bovis and are implicated in the transmission of tuberculosis to cattle in Ireland and Great Britain. The development of a vaccine for use in badgers is considered a key element of any long-term sustainable campaign to eradicate the disease from livestock in both countries. The aim of this study was to investigate the protective response of badgers vaccinated orally with Bacille Calmette–Guérin (BCG) encapsulated in a lipid formulation, followed by experimental challenge with M. bovis. A group of badgers was vaccinated by inoculating the BCG–lipid mixture containing approximately 108 colony forming units (cfu) of BCG into the oesophagus. The control group was sham inoculated with the lipid formulation only. Thirteen weeks after vaccination all the badgers were challenged with approximately 104 cfu of M. bovis delivered by endobronchial inoculation. Blood samples were taken throughout the study and the cell mediated immune (CMI) responses in peripheral blood were monitored by the IFN-␥ ELISA and ELISPOT assay. At 17 weeks after infection all the badgers were examined post-mortem to assess the pathological and bacteriological responses to challenge. All badgers in both groups were found to be infected. However, a significant protective effect of BCG vaccination was measured as a decrease in the number and severity of gross lesions, lower bacterial load in the lungs, and fewer sites of infection. The analysis of immune responses showed that vaccination with BCG did not generate any detectable CMI immunological responses, however the levels of the responses increased in both groups following M. bovis infection. The results of the study showed that vaccination with oral BCG in the lipid formulation generated a protective effect in the badgers. © 2010 Elsevier Ltd. All rights reserved. 1. Introduction Bovine tuberculosis, caused by Mycobacterium bovis infection, is present in the Eurasian badger (Meles meles) populations in Ireland and Great Britain [1,2]. The badger is a significant reservoir of infection for domestic animals and continued infection in the badger population has significant economic effects on the cattle industry. That infection in the badger population is a source of infection for cattle in Ireland and GB was demonstrated by the reduction in the incidence of tuberculosis in cattle herds following removal of infected badgers [3,4]. Vaccination of badgers is seen as a key element in any long-term strategy to eradicate the disease from cattle. The BCG (Bacille Calmette–Guérin) vaccine, an avirulent live ∗ Corresponding author. Tel.: +353 1 716 6073; fax: +353 1 716 6091. E-mail address: egormley@ucd.ie (E. Gormley). 0264-410X/$ – see front matter © 2010 Elsevier Ltd. All rights reserved. doi:10.1016/j.vaccine.2010.06.120 strain of M. bovis, is the only vaccine currently available for use in domestic and wild animals. Several studies have shown that BCG is protective in cattle [5], deer [6], brushtail possums [7], ferrets [8], wild boar [9] and badgers [10,11]. In wild brushtail possums BCG was found to prevent infection and had high protective efficacy (69–95%) [12,13]. Badgers have also been successfully vaccinated by administering BCG by a variety of different routes: intradermal [10] and subcutaneous and mucosal [11]. For the BCG vaccine to be used to control tuberculosis in wild badgers on a wide scale, and in a cost-effective manner, it is likely that oral delivery would be the method of choice. As has been shown in the control of wildlife rabies in Europe and North America, a vaccination program based on the delivery of vaccine in an oral bait to a wild animal population can be successfully undertaken [14,15]. Vaccination studies including the oral route of delivery have shown that it is necessary for BCG to be delivered live in order to generate immunity [16]. In studies where 6266 L.A.L. Corner et al. / Vaccine 28 (2010) 6265–6272 unprotected BCG did not induce protection it was suggested that this might be due to killing of the BCG in the stomach, as intragastric vaccination was ineffective compared with intraduodenal vaccination [17]. In other studies, protection has been achieved by encapsulating BCG in a lipid matrix formulation [18]. The matrix is composed of triglycerides of fatty acids with varying concentrations of myristic acid, palmitic acid, stearic acid, oleic acid and linoleic acid that provides a stable storage and delivery vehicle for BCG [18,19]. When lipid-encapsulated BCG was delivered to mice by mouth, the bacilli established replicating populations in the lymph nodes of the alimentary tract, principally in the mesenteric lymph nodes (MLNs) draining the gastro-intestinal tract [20]. It also appears that encapsulation prolongs the in vivo survival of the BCG and helps to confer long lasting protective immune responses [21]. Studies have shown that the oral vaccine can induce protective immune responses in mice [22], guinea pigs [23,24] brushtail possums [25] and cattle [26]. Oral BCG has also been shown to prevent M. bovis infection in wild possum populations following natural exposure to M. bovis [13,27]. The aim of the study reported here was to determine if live BCG, encapsulated in the lipid matrix, would induce a protective response when administered by the by intra-oesophageal route to badgers. Vaccinated badgers were challenged by the endobronchial route with virulent M. bovis and the response to infection determined by post-mortem examination and culture, and measurement of immunological responses. 2.2. Vaccination with BCG 2. Methods The BCG Pasteur strain used in this study has frequently been used in animal studies and was recommended by a joint WHO, FAO/OIE consultative group in 1994 for use in vaccine trials in animals [28]. The BCG was formulated in a lipid matrix, as previously described [19]. This preparation is liquid at 37 ◦ C (which enables dispersal of viable bacilli), but solidifies below 30 ◦ C. The lipid was an animal derived fractionated complex lipid which contained triglycerides of the following fatty acids: 1% myristic acid, 25% palmitic acid, 15% stearic acid, 50% oleic acid and 6% linoleic acid, and has been used in previous oral BCG vaccination studies in mice and possums [18,19]. For formulation, broth-cultured BCG was pelleted and resuspended in the lipid medium that had been warmed to 37 ◦ C to achieve a final concentration of 1 × 108 colony forming units (cfu)/ml of lipid [18]. BCG (and control) formulations were transferred to 20 ml Luer-Lock syringes and allowed to solidify at 4 ◦ C while being gently mixed. Before use, the syringes containing the lipid mixtures were warmed to room temperature, then a 1.5 mm plastic cannula was attached and, to ensure accurate dosing, the cannula was filled with lipid. Badgers were vaccinated by passing the cannula approximately 10 cm down the oesophagus and inoculating 1 ml of the BCG–lipid mixture. The control group (N = 7) was sham inoculated with the lipid formulation only. The vaccinated badgers (N = 7) received approximately 108 cfu of BCG as determined by retrospective counts following extraction of BCG from representative samples of the lipid-formulated vaccine [18]. To detect excretion of BCG, fresh faeces were collected from pens on days 1, 2, 3 4, 9 and 17 post-vaccination. 2.1. Handling of captive badgers 2.3. M. bovis suspension and experimental infection All work with badgers was carried out under licences issued by National Parks and Wildlife Service and the Department of Health and Children, and ethical approval was obtained from the UCD animal research ethics committee. Fourteen badgers were used in the study, all obtained from wild populations that were free of tuberculosis (as assessed by historical record and immunological assays at least twice prior to vaccination). The badgers were maintained in captivity in groups of 2–4, in outdoor pens each with an area of ∼200 m2 , with earthen floors covered in grass and containing some shrubs. In each pen were two or three wooden setts that each contained an inner nest box. The badgers were fed proprietary dog biscuits, raw peanuts and fresh chicken pieces. Fresh water was available ad libitum. The badgers were acclimatised to captivity for at least 6 weeks prior to the commencement of the experiment. The badgers were allocated to either a vaccine group (seven badgers) or a non-vaccinated control group (seven badgers). Badgers in the vaccine group were housed separately from the control badgers and the groups contained similar numbers of male and female badgers. For handling, the badgers were anaesthetised with ketamine hydrochloride (10 mg/kg) and medetomidine hydrochloride (0.1 mg/kg, Domitor® , Pfizer) co-administered by intramuscular injection. The badgers were examined 2 weeks before vaccination and at 0, 2, 4, 7, 10 and 13 weeks post-vaccination and 2, 4, 6, 9, 12 and 16 weeks after infection. Badgers were challenged at week 13 post-vaccination. On each occasion the badgers were weighed and examined for signs of disease or injury, and blood was collected by jugular venopuncture. A tracheal aspirate was collected by passing a 1.5 mm (outside diameter, OD) catheter down the trachea to the bifurcation and as the catheter was withdrawn mucus was drawn into the lumen of the catheter. The mucus was flushed from the lumen of the catheter and washed from the outside of the catheter with phosphate buffered saline containing 0.05% Tween-80 (PBST) and collected for culture. M. bovis strain M2137, originally isolated from a tuberculous badger, was grown to stationary phase in Middlebrook 7H9 broth (Difco, Becton Dickinson and Company, Sparks, MD, USA) supplemented with 0.1% Tween-80, centrifuged, and the pellet resuspended and washed in PBS containing 0.05% Tween-80 (PBST). The suspension, containing approximately 1 × 108 cfu/ml, was stored at −70 ◦ C in 2.5 ml aliquots [29]. For inoculation the suspension was thawed and adjusted to the required concentration with PBST. The badgers were anaesthetised and a small animal endoscope (3.7 mm OD fibre optic endoscope, Veterinary Endoscopy Systems, UK) was introduced into the bronchus of the right middle lobe (RMD). When in place a 1 mm OD cannula with a void volume of 0.8 ml was inserted deep into the bronchus and 1.0 ml of the M. bovis suspension instilled. The cannula was flushed with 1.0 ml of sterile PBS. The badgers were immediately placed in right lateral recumbency and allowed to recover. The inoculum stock was then re-cultured to determine the precise dose delivered to the badgers. The actual suspension used for inoculation contained 8 × 103 cfu/ml. 2.4. Post-mortem examination At 17 weeks post-infection (pi) all the badgers were anaesthetised and then euthanased with an intravenous overdose of sodium pentabarbitone. The euthanased badgers were subjected to a detailed necropsy. The severity of the gross lesions in lymph nodes and organs were scored according to the scheme described previously and individual scores of lesions were added to generate an overall pathology score [29]. The anatomical sites examined for gross pathology and by histopathology, and the samples collected for bacteriological examination are listed in Table 1. All the lymph nodes (LN) visible at each site were collected and a small portion of each was fixed for histological examination and the remainder retained for bacteriology. Tissues for bacteriology were collected L.A.L. Corner et al. / Vaccine 28 (2010) 6265–6272 Table 1 Vaccination of badgers with BCG by the oral route and response to experimental infection with Mycobacterium bovis: distribution of infection. Tissue or samplea Left mandibular LN Right mandibular LN Left parotid LN Right parotid LN Left deep cervical LN Right deep cervical LN Left caudal cervical LN Right caudal cervical LN Left axillary LN Right axillary LN Left inguinal LN Right inguinal LN Left popliteal LN Right popliteal LN Left bronchial LN Right bronchial LN Anterior mediastinal LN Posterior mediastinal LN Left cranial lobe Left caudal lobe Right cranial lobe Right middle lobe Right caudal lobe Accessory lobe Pleura Mesenteric LN Hepatic LN Liver Spleen Left kidney Right kidney Faecesc Urinec Group Vaccinate N=7 Control N=7 0 0 0 0 3 (1–3) 3 (2–3) 0 0 0 0 0 0 0 1 (2) 3 (1–2) 7 (3–5) 2 (2) 5 (3–4) 0 0 0 7 (2–5) 3 (1–3) 2 (2) 3 (1–5) 4 (2–3) 5 (2–4) 0 0 0 0 1 0 0 0 1 (1–2)b 0 0 2 (1–2) 0 0 1(1) 3 (1–2) 0 0 0 1 (1) 4 (1–3) 7 (4–6) 1 (3) 7 (2–6) 2 (1–2) 1 (2) 3 (1–4) 5 (2–5) 2 (1–6) 4 (2–5) 3 (4) 2 (1) 6 (1–4) 0 2 (1–2) 1 (1) 1 (3) 0 1 6267 in the sample could be calculated (cfu/g). Tissue samples were cultured without decontamination except for lungs; these along with urine and tracheal aspirates were decontaminated with 0.075% w/v cetylpyridinium chloride (CPC) prior to culture. Faeces were decontaminated with 0.75% w/v CPC prior to culture. For each specimen two plates of modified Middlebrook 7H11 medium (Difco, Becton Dickinson and Company, Sparks, MD, USA) containing a mixture of antibiotics (polymyxin B 200,000 unit/l, ticarcillin 100 mg/l, amphotericin B 10 mg/l and trimethoprim 10 mg/l; Mycobacteria selectatab, Mast Diagnostics, Derby Road, Bootle, UK), two slopes of Lowenstein–Jensen with pyruvate (LJP) medium, two slopes of Stonebrink’s medium with pyruvate (SB) and one tube of BACTEC 12B medium were inoculated. When primary cultures of tissue samples were contaminated, a stored portion of the macerated sample was decontaminated with 0.075% w/v CPC and media reinoculated. All inoculated media were incubated at 37 ◦ C for 12 weeks. BACTEC 12B media were checked for growth using the BACTEC 460 radiometric system (Becton Dickinson and Company, Sparks, MD). The mean number of colonies on the 7H11 plates was used to calculate the concentration of M. bovis in the sample. Where a specimen was positive only in BACTEC 12B, and for urine, faeces and tracheal aspirates, results were recorded as only positive or negative. Preliminary isolate identification was based on colony morphology, growth rate, pigmentation and cording characteristics [31]. Spoligotyping of selected isolates, which confirmed isolates as M. bovis and differentiates between BCG and the challenge strain, was performed according to the method of Kamerbeek et al. [32]. All of the isolates from clinical and post-mortem samples had either the wild type M. bovis or BCG profile on spoligotyping and those from the faeces collected in the same pens, a BCG profile (data not shown). 2.6. Mycobacterial antigens and immunological assays a M. bovis was not isolated from the adrenal glands nor organs of the reproductive tract (testicles and seminal vesicles, or uterus and mammary glands). b The number of badgers from which M. bovis was isolated and in parentheses the concentration of bacilli in the tissue, expressed as log10 colony forming units per gram of tissue cultured. c The culture of urine and faeces was recorded only as positive or negative. using an aseptic technique to minimise contamination (including cross-contamination with M. bovis) and so that culturing could be done without decontamination or with a low concentration of the decontaminant. Also cultured were urine aspirated from the bladder, rectal faeces, and samples of liver (∼2 g), spleen (∼2 g), half of each kidney and 2–5 g taken from the centre of each lung lobe. Where macroscopic lesions were observed on the surface of a lung lobe or a lesion was palpated within the parenchyma, these were collected separately for culture. After the samples for culture had been collected, the lungs were fixed in buffered formalin. After fixation for a minimum of 14 days, the fixed lungs were sliced at 2 mm intervals and the cut surfaces examined for macroscopic lesions. After fixation, histopathology samples were embedded in paraffin, sectioned at 3 m and stained with haematoxylin and eosin, and by the Ziehl–Neelsen method for acid-fast bacteria. The histopathological examination consisted of the detection of lesions of tuberculosis, i.e., granulomas containing acid-fast bacteria [30]. Only gross lesions confirmed as tuberculosis by histology and/or bacteriology are listed in Table 2. 2.5. Bacteriology Specimens for culture were processed as previously described [29] and each specimen was cultured separately. Tissue samples were weighed before culture so that the concentration of M. bovis PBMC were isolated from whole blood as described previously [33]. The levels of badger IFN-␥ in PBMC cultures stimulated with bovine tuberculin and CFP10 was measured by ELISA [34]. Briefly, up to 10 ml of heparinised blood was collected from each animal and 0.75 ml aliquots were dispensed into individual wells of 24-well tissue culture plates (Costar, UK). In addition, wells contained 0.75 ml of each of the following: 30 g/ml purified protein derivative of M. bovis (PPD-Bov, Weybridge VLA), 5 g/ml CFP10 (kind gift of Lionex GmbH, Germany), a negative control or 5 g/ml pokeweed mitogen (PWM, Sigma) as a positive control, diluted in RPMI (Invitrogen Life Technologies) supplemented with 25 UI/ml of heparin (Roche Diagnostics). The endotoxin levels of CFP10 were measured at <0.4 EU/g antigen. The cultures were incubated for 16 h at 37 ◦ C in a humidified atmosphere with 5% CO2 before harvesting of plasma supernatants after centrifugation. IFN-␥ production was measured for each antigen in duplicate, in a sandwich ELISA using mouse anti-badger IFN-␥ monoclonal antibody mAb 11b9 (VLA, Weybridge UK) for capture (diluted 1/200) and rabbit anti-badger IFN-␥ polyclonal antibody Rb300 for detection (diluted 1/200) [34]. The mean optical density (OD) values were calculated for each antigen–blood combination and the results are expressed as mean OD of stimulated PBMC minus OD of PBMC cultured in the absence of antigen. The badger IFN-␥ Elispot was carried out as described previously [35]. Briefly, 96-well ELISPOT plates (Millipore multi-screen, Millipore Ltd., UK) were coated with capture mAb 11b9 at 10 g/ml in carbonate/bicarbonate buffer, pH 9.6 overnight at 4 ◦ C. Lymphocytes were isolated from heparinised whole blood and 100 l of cells (final concentration 2 × 106 cells/ml) resuspended in RPMI, supplemented with 5% fetal calf serum, (Invitrogen Life Technolo- 6268 L.A.L. Corner et al. / Vaccine 28 (2010) 6265–6272 Table 2 Vaccination of badgers with BCG by the oral route and response to experimental infection with Mycobacterium bovis: distribution of gross lesions subsequently confirmed as tuberculosis. PM groupa Vaccine Control Badger BR4-30 BR4-50 BR4-53 BR4-55 BR4-62 BR4-89 BR4-91 BR4-17 BR4-23 BR4-56 BR4-66 BR4-79 BR4-94 BR4-97 Tissueb Total score BrL BrR MedA MedP 1c 0 0 0 0 0 0 0 0 0 0 0 1 1 3 3 1 2 1 3 4 1 3 4 3 4 4 1 0 0 0 0 0 0 0 0 0 0 0 0 4 0 3 0 0 0 0 0 0 2 1 2 4 1 1 1 Lung lobe LCR LCD RCR RMD RCD Acc 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 1 0 0 1 0 0 0 3 0 0 0 1 0 2 3 2 2 3 4 4 0 3 4 0 4 4 0 2 0 0 0 0 0 1 1 1 0 4 1 0 0 1 0 0 0 0 0 0 4 0 0 0 0 0 4 Pleura Hep Kid 0 0 1 1 0 1 1 0 0 1 0 0 1 2 0 0 0 0 1 0 0 0 0 0 0 0 2 0 0 0 0 0 0 0 0 0 0 0 3 0 0 0 12 7 4 5 6 8 10 8 11 11 14 10 18 9 a Badgers were examined post-mortem at 17 weeks after infection. No macroscopic lesions were observed in the reproductive tract (testicles and seminal vesicles, or uterus and mammary glands), the lymph nodes (LN) of the head (mandibular, parotid, deep cervical), the tonsils, superficial body LNs (caudal cervical, axillary, inguinal or popliteal), nor in the spleen, liver, adrenal glands, or mesenteric LN. b BrL, left tracheobronchial LN; BrR, right tracheobronchial LN; MedA, anterior mediastinal LN; MedP, posterior mediastinal LN; LCR, left cranial lobe; LCD, left caudal lobe; RCR, right cranial lobe; RMD, right middle lobe; RCD, right caudal lobe; Acc, right accessory lobe; Hep, hepatic LN and Kid, kidney. c Lesions severity score. gies), non-essential amino acids, 5 × 10−5 M -mercaptoethanol (Invitrogen Life Technologies) and 100 U penicillin/100 g streptomycin per ml (Invitrogen Life Technologies) was diluted in 100 l with one of each of the following: PPD-Bov (30 g/ml, Institute of Animal Science and Health, Lelystad, Netherlands), CFP10 (5 g/ml), Con-A (5 g/ml) diluted in supplemented RPMI. Negative controls were incubated in supplemented RPMI without antigen. The plates were incubated for 16 h at 37 ◦ C and 5% CO2 . The liquid was discarded, the plates washed three times in distilled water, followed by three washes with buffer (PBS, 0.05% Tween-20, v/v). 100 l of mAb Rb300 diluted 1/400 in PBS, 0.05% Tween-20, 0.1% albumin, was added to each well and the plates incubated at 37 ◦ C for 1 h. The plates were then washed three times with wash buffer. Biotinylated mouse rabbit anti-mouse IgG (Sigma, Ireland) was diluted 1/1000 in PBS, 0.05% Tween-20, 0.1% albumin, and added to the plates, which were incubated at 37 ◦ C for 1 h. The plates were washed and 100 l of streptavidinalkaline-phosphatase (Mabtech AB, Hamburg, Germany) diluted 1/4000 in PBS, 0.05% Tween-20, 0.1% albumin, and incubated at 37 ◦ C for 1 h. Again the plates were washed with wash buffer and 100 l of BCIP/NBT (bromo-4-chloro-3-indolyl phosphate – Nitro blue tetrazolium, Sigma–Aldrich) substrate added to each well and the reaction was stopped after 10–20 min by liberal washing with water. The plates were allowed to dry and spots counted using an automated AID ELISPOT reader (Autoimmun Diagnostika GmbH, Strasberg, Germany) and the net spot forming units (SFU) were calculated. 2.7. Statistical analysis The data were tested for normality using GraphPad Prism version 4.00 for Windows (GraphPad Software, USA, www.graphpad.com). Differences between groups were analysed using Mann–Whitney test or t-test using GraphPad and SPSS version 12.0.1 for Windows (Apache Software Foundation, USA, www.spss.com). 3. Results 3.1. Post-mortem examination of badgers Thirteen weeks after vaccination all the badgers in both groups were challenged with 8 × 103 cfu of M. bovis by endobronchial inoculation. At 17 weeks post-infection all the badgers were examined post-mortem to assess the pathological and bacteriological responses to challenge. Infection was found to be established in all of the badgers as judged by the presence of gross lesions and culture for M. bovis. The lesions in the vaccine group were restricted to the thoracic cavity in all except one badger, BR4-62 (Table 2). Lesions in the thoracic lymph nodes were only present in the right tracheobronchial LN (BrR) in 6/7 badgers, but were seen in the BrR, left tracheobronchial (BrL) LN and posterior mediastinal LN (Med P) in the seventh badger (BR4-30). The most severe lung lesions were associated with the RMD (right middle lobe) in vaccinated badgers. Lesions were observed in a second lobe in three badgers and in two additional lobes in BR4-30. Other gross lesions observed were pleurisy in four badgers and lesions in the hepatic LN (Hep) of one badger (BR4-62). When compared with the control sham-vaccinated group, the vaccine group had significantly fewer (MW test, p = 0.036) lesions than the control group (Fig. 1A). Gross lesions in the control group were observed in two thoracic lymph nodes (BrR and MedP LN) in all badgers and also in the BrL in BR4-97, and the BrL and anterior mediastinal (MedA) LN in BR4-94 (Table 2). The most severe lung lesions in the control group were associated with the RMD in four badgers, the accessory lobe (Acc) in two badgers and the right caudal lobe (RCD) in another badger, BR4-66. Lesions were also seen in two or more lobes in four badgers. Other gross changes observed were pleurisy in three badgers, lesions in an HEP of BR4-94 and a kidney lesion in BR4-66. The kidney lesion was in the papilla of the right kidney and there was exudate containing AFB present in the renal pelvis. In addition to the number of gross lesions observed, the severity of the lesions in the vaccine group was significantly lower than in the control group (t-test, p = 0.015, Fig. 1B). Following histological examination the vaccine group had marginally fewer sites L.A.L. Corner et al. / Vaccine 28 (2010) 6265–6272 6269 Fig. 1. Vaccination of badgers with BCG by the oral route and response to experimental endobronchial infection with Mycobacterium bovis. (A) Number of confirmed gross lesions of tuberculosis. The vaccine group had fewer lesions (median 3) than the control group (median 4) and the difference was significant (MW test, p = 0.036). Line indicates median value. (B) Severity of disease based on severity score for each tissue. The vaccine group had significantly lower severity scores than the control group (t-test, p = 0.015). Line indicates mean value. (C) Bacterial load in the most severely affected lung lobe. The vaccine group had a lower bacterial load than the control group and the difference was significant (t-test, p = 0.036). Line indicates mean value. (D) Number of sites of infection. There were fewer sites in the vaccine group (mean 7.1) than in the control group (mean 8.7) and the difference was significant (t-test, p = 0.031). Line indicates mean value. with histological lesions (median 5, range 2–6) than the control group (median 5, range 4–6) but the difference was not significant. 3.2. Bacteriological examination of badgers The distribution of samples from which M. bovis was isolated and the bacterial load in each sample is shown in Table 1. In the vaccine group the bacterial load in the most heavily infected lung lobes was significantly less (t-test, p = 0.036) than in the control group (Fig. 1C). There were fewer sites of infection in the vaccine group (mean 7.1) than the control group (mean 8.7) and the difference was significant (t-test, p = 0.031, Fig. 1D). In the vaccine group the bacterial load in the most severely infected thoracic LNs (mean 4.43 ± 0.30) was less than in the control group (mean 5.00 ± 0.31) however, the difference was non-significant (t-test, p = 0.104, data not shown). There were some differences between groups in the extra-thoracic sites of infection. M. bovis was isolated from the spleen and both kidneys of one control and the spleen of another, but not from these organs in the vaccine group. M. bovis was isolated from the urine of one control badger (3 log10 cfu/ml) that had renal lesions (BR4-66), and from the faeces of vaccinated badger BR4-55. Only one tracheal aspirate was culture positive and that was collected from a control badger, BR4-66, 3 weeks after challenge. BCG was also isolated from tissues of four vaccinated badgers (Table 3). In three of these badgers BCG was isolated along with the M. bovis challenge strain. Seventeen faecal samples were collected from pens containing vaccinated badgers over a period of 17 days post-vaccination. These included multiple samples collected on a single day from one pen. BCG was isolated on only two occasions and from the same pen, one that contained three vaccinated badgers. In addition, BCG was only found in low numbers: at a concentration of 20 cfu/g faeces on day 3 post-vaccination and at 1 cfu/g faeces on day 17 post-vaccination. 3.3. Clinical examination Throughout the study, the general health of all badgers was monitored routinely to detect evidence of any adverse effects resulting from vaccination and/or challenge. The body weights of the badgers in both treatment groups increased from the time of vaccination in June (mean 10.39 kg ± sd 1.07) to challenge in September (mean 13.02 kg ± sd 1.57), were maximum in November at 9 weeks pi (mean 14.21 kg ± sd 1.59), and declined towards the end of the study in January (mean 12.29 kg ± sd 1.62). There was no difference between groups in the way the body weights changed. In addition, the body weights of the badgers were higher at the time of post-mortem than at the time of vaccination (mean increase 2.28 kg ± sd 1.22). No clinical signs related to vaccination or the experimental infections were seen in any badger. The body weights of badgers in both treatment groups increased from the time of vaccination (mean overall body weight 10.39 ± sd 1.07) to”. There was no difference between groups in the way the body weights changed. Table 3 Vaccination of badgers with BCG by the oral route and response to experimental infection with Mycobacterium bovis: distribution of isolated strains in cervical lymph nodes. Badger BR4-30 BR4-50 BR4-53 BR4-55 BR4-62 BR4-89 BR4-91 a Tissuea RDC LDC – BCG + M. bovis – BCG BCG + M. bovis M. bovis – – M. bovis – M. bovis – BCG + M. bovis – LDC, left deep cervical lymph node, RDC, right deep cervical lymph node. 6270 L.A.L. Corner et al. / Vaccine 28 (2010) 6265–6272 Fig. 2. Badger IFN-␥ release from PBMC stimulated with PPD-Bov (A and C) and CFP10 (B and D) as measured by ELISA (A and B) and ELISPOT (C and D). Arrow indicates time of infection with M. bovis at week 13. Time points are weeks post-vaccination (T0). Results are presented as mean values ± SD. 3.4. IFN- responses of badgers following BCG vaccination and infection with M. bovis The IFN-␥ responses in PBMC of all badgers were monitored in vitro by the badger IFN-␥ ELISA and ELISPOT assay using PPDBov and CFP10 as stimulating antigen. The response profiles of both vaccinated and control groups were similar using either assay (Fig. 2A–D) and were consistent with the observed severity of pathology at the end of the study in both groups. Antigen specific responses were not observed following vaccination with BCG but were detected as early as 2 weeks post-challenge in both groups. The responses peaked between 4 and 6 weeks post-challenge in both vaccine and control groups. Thereafter, the production of IFN-␥ declined in both groups but remained higher than the preinfection levels. The mean ELISA antigen specific IFN-␥ response was higher in the control group compared with the vaccine group. In contrast the response in the vaccine group was higher when the ELISPOT assay was used. With both assays, however, the differences were not statistically significant between the groups except for one time-point 2 weeks post-challenge where the control group was significantly higher in the response to stimulation with PPD-Bov, measured by ELISPOT. 4. Discussion In this study orally delivered lipid-formulated BCG vaccine induced a protective response in the vaccinated badgers. The protective response was measured as fewer sites with gross lesions, a decrease in the severity of gross lesions, fewer sites of infection, and lower bacterial load in the lungs and thoracic lymph nodes compared with the control group. The results are consistent with those obtained following subcutaneous and mucosal vaccination of badgers with BCG, and are also consistent with the development of a protective response obtained when lipid-formulated BCG vaccine was studied in mice [22], possums [18], guinea pigs [23,24] and cattle [26]. Vaccination with oral BCG did not prevent infection in the badgers, as all badgers of both treatment groups were found infected at post-mortem. Badgers are very susceptible to endobronchial infection and we have previously shown that they can be experimentally infected with as few as 10 cfu [29]. However, in order to obtain uniform results, we used a high challenge dose of 104 cfu of M. bovis [11]. The immune protection demonstrated in the vaccinated group is therefore likely to be an underestimate of the true vaccine effect, given the severity of the challenge. The use of an endoscope permitted the delivery of the M. bovis suspension directly to the right middle and caudal lobes of the lung. The disease produced was similar to that in naturally infected badgers [36,37]. In the majority the infection was mild and respiratory excretion of M. bovis after challenge was rare, detected only once in a tracheal aspirate of a control group badger. There was dissemination of infection to extra-thoracic sites in badgers of both treatment groups. Overall, the distribution of infection was wider than that shown by histology, with the latter generally consistent with the distribution of gross pathology. BCG was recovered from faeces and tissues of vaccinated badgers. Faecal excretion of BCG occurred for at least 17 days after vaccination, although only low concentrations of bacilli were detected. In similar studies with orally vaccinated possums maximum excretion of BCG in faeces (103 cfu/g of faeces) occurred on day 2 and excretion was undetectable beyond 7 days postvaccination [25]. In addition, BCG was not cultured from possum faeces when exposed for 1 week on pasture. It was concluded from this observation that, due to the loss of viability of BCG in faeces exposed on pasture, environmental contamination with BCG in faeces would be short-lived and unlikely to pose a problem to cattle grazing the pasture. BCG was isolated from one tissue collected at post-mortem from each of four badgers and in each instance a deep cervical LN (syn. medial retropharyngeal LN) was infected. In three of these badgers there was concurrent infection with BCG and the M. bovis challenge strain in the affected tissue. After oral BCG vaccination BCG has been shown to persist for up to 30 weeks in mice where it was recovered from the mesenteric LNs [21] and 8 weeks in brushtail possums [25]. Co-infection with BCG and virulent M. bovis in vaccinated animals has not been reported previously. L.A.L. Corner et al. / Vaccine 28 (2010) 6265–6272 As with previous badgers studies there was limited CMI responses following vaccination with BCG [38]. The BCG dose of 108 cfu was chosen for this study as it conferred significant protection against infection with virulent M. bovis in other animal species [19,26]. The immunogenicity of BCG in badgers has been investigated in a number of previous studies and low CMI responses were reported, irrespective of the route of vaccination [35,39,40]. It was suggested that a relatively low T lymphocyte response to PPD-Bov following BCG vaccination might be a feature characteristic of the mustelid response. The reason for the low response is unclear though it may be dose-dependent and the response was too low to be detectable in peripheral blood. In another study carried out with captive badgers, subcutaneous injection of badgers with high doses (107 –108 cfu) of BCG generated relatively high IFN-␥ levels when PBMC were stimulated with PPD-Bov and IFN-␥ responses measured by ELISPOT [35]. That study provided evidence of a BCG dependent CMI response in badgers, as has been found in cattle and mice [5,41]. The generation of elevated immune responses following BCG vaccination by the oral route has been associated with increased levels of protection in possums [25]. However, in the current study the lack of response of badgers to the oral BCG vaccination was not associated with a failure of the vaccine to protect. It is reasonable to assume that oral-delivered BCG must have survived passage through the stomach and crossed the intestinal mucosa to establish infection and induce protective immunity. We have previously shown that the production of IFN-␥ by badger T lymphocytes in response to mycobacterial antigens is indicative of a cellular response to active infection [38]. The IFN␥ responses of the vaccinated group were significantly higher 2 weeks post-challenge than the non-vaccinated controls when measured by ELISPOT. This apparent anamnestic response in vaccinated badgers is consistent with observations reported previously for BCG-vaccinated cattle. These studies showed that BCG vaccinated calves that were protected against M. bovis challenge developed cellular immune responses very early after M. bovis challenge at a time-point when no responses were yet detectable in unvaccinated controls [42]. From 4 weeks post-challenge, however, the response of both groups (vaccinates and controls) was similar. Although some of the pathology scores were significantly lower in the vaccinated badgers than in the controls, the difference in the extent of lesions was not reflected in distinct immunological profiles, and it was not possible to correlate post-vaccination peripheral immune responses induced by oral BCG with the levels of protection that were measured. The success of oral vaccination of captive badgers significantly advances the possibility of vaccinating wild badger populations for the control of M. bovis infection [2]. However, before BCG vaccine can be utilised to control bovine tuberculosis in wild badger populations it will be essential to study the responses of wild badgers to oral BCG vaccination. Whereas infection of captive badgers in a vaccination-challenge experiment can at best reveal the potential of oral BCG vaccination, studies in free-ranging wild animals under conditions of natural M. bovis transmission will reveal the full potential of BCG induced protection. Before oral vaccination is incorporated into the national bovine tuberculosis eradication program, further studies will be required to determine the presentation and type of bait required for targeting the oral vaccine to free-ranging badgers and the optimal dose of oral BCG required for protecting badgers against natural infection with M. bovis. Acknowledgements The study described in this paper was funded by the Department of Agriculture, Fisheries and Food (DAFF), Republic of Ireland. 6271 S. Lesellier was also supported through a project funded by the Department for Environment, Food and Rural Affairs (DEFRA), GB. Matt Lambeth (Immune Solutions Ltd.) is gratefully acknowledged for assistance with preparing the oral BCG vaccine. The help of staff in the Mycobacteriology Laboratory at the Central Veterinary Research Laboratory (Backweston, Co. Kildare) is appreciated. We also acknowledge the help and support provided by Ian O’Boyle (DAFF), Michael Sheridan (DAFF), Margaret Good (DAFF), Paddy Sleeman (UCC) and Prof. Dan Collins (UCD). References [1] Clifton-Hadley RS, Wilesmith JW, Richards MS, Upton P, Johnston S. The occurrence of Mycobacterium bovis infection in cattle in and around an area subject to extensive badger (Meles meles) control. Epidemiol Infect 1995;114(1): 179–93. [2] Gormley E, Collins JD. The development of wildlife control strategies for eradication of tuberculosis in cattle in Ireland. Tuber Lung Dis 2000;80(4/5):229–36. [3] Griffin JM, Williams DH, Kelly GE, Clegg TA, O’Boyle I, Collins JD, et al. The impact of badger removal on the control of tuberculosis in cattle herds in Ireland. Prev Vet Med 2005;67(4):237–66. [4] Donnelly CA, Wei G, Johnston WT, Cox DR, Woodroffe R, Bourne FJ, et al. Impacts of widespread badger culling on cattle tuberculosis: concluding analyses from a large-scale field trial. Int J Infect Dis 2007;11(4):300–8. [5] Buddle BM, de Lisle GW, Pfeffer A, Aldwell FE. Immunological responses and protection against Mycobacterium bovis in calves vaccinated with a low dose of BCG. Vaccine 1995;13(12):1123–30. [6] Griffin JFT, Mackintosh CG, Slobbe L, Thomson AJ, Buchan GS. Vaccine protocols to optimise the protective eficacy of BCG. Tuber Lung Dis 1999;79(3):135–43. [7] Aldwell FE, Pfeffer A, DeLisle GW, Jowett G, Heslop J, Keen D, et al. Effectiveness of BCG vaccination in protecting possums against bovine tuberculosis. Res Vet Sci 1995;58(1):90–5. [8] Qureshi T, Labes RE, Cross ML, Griffin JF, Mackintosh CG. Partial protection against oral challenge with Mycobacterium bovis in ferrets (Mustela furo) following oral vaccination with BCG. Int J Tuberc Lung Dis 1999;3(11):1025–33. [9] Ballesteros C, Garrido JM, Vicente J, Romero B, Galindo RC, Minguijon E, et al. First data on Eurasian wild boar response to oral immunization with BCG and challenge with a Mycobacterium bovis field strain. Vaccine 2009;27(48):6662–8. [10] Stuart FA, Mahmood KH, Stanford JL, Pritchard DG. Development of diagnostic tests for, and vaccination against, tuberculosis in badgers. Mammal Rev 1988;18:74–5. [11] Corner LA, Costello E, Lesellier S, O’Meara D, Gormley E. Vaccination of European badgers (Meles meles) with BCG by the subcutaneous and mucosal routes induces protective immunity against endobronchial challenge with Mycobacterium bovis. Tuberculosis (Edinb) 2008;88(6):601–9. [12] Corner LA, Buddle BM, Pfeiffer DU, Morris RS. Vaccination of the brushtail possum (Trichosurus vulpecula) against Mycobacterium bovis infection with Bacille Calmette–Guerin: the response to multiple doses. Vet Microbiol 2002;84(4):327–36. [13] Tompkins DM, Ramsey DS, Cross ML, Aldwell FE, de Lisle GW, Buddle BM. Oral vaccination reduces the incidence of tuberculosis in free-living brushtail possums. Proc Biol Sci 2009;276(1669):2987–95. [14] Stohr K, Meslin FM. Progress and setbacks in the oral immunisation of foxes against rabies in Europe. Vet Rec 1996;139(2):32–5. [15] Brochier B, Aubert MF, Pastoret PP, Masson E, Schon J, Lombard M, et al. Field use of a vaccinia-rabies recombinant vaccine for the control of sylvatic rabies in Europe and North America. Rev Sci Tech 1996;15(3):947–70. [16] Buddle BM, Aldwell FE, Keen DL, Parlane NA, Hamel KL, de Lisle GW. Oral vaccination of brushtail possums with BCG: investigation into factors that may influence vaccine efficacy and determination of duration of protection. N Z Vet J 2006;54(5):224–30. [17] Buddle BM, Aldwell FE, Keen DL, Parlane NA, Yates G, de Lisle GW. Intraduodenal vaccination of brushtail possums with bacille Calmette–Guerin enhances immune responses and protection against Mycobacterium bovis infection. Int J Tuberc Lung Dis 1997;1(4):377–83. [18] Aldwell FE, Keen DL, Parlane NA, Skinner MA, de Lisle GW, Buddle BM. Oral vaccination with Mycobacterium bovis BCG in a lipid formulation induces resistance to pulmonary tuberculosis in brushtail possums. Vaccine 2003;22(1):70–6. [19] Aldwell FE, Tucker IG, de Lisle GW, Buddle BM. Oral delivery of Mycobacterium bovis BCG in a lipid formulation induces resistance to pulmonary tuberculosis in mice. Infect Immun 2003;71(1):101–8. [20] Aldwell FE, Baird MA, Fitzpatrick CE, McLellan AD, Cross ML, Lambeth MR, et al. Oral vaccination of mice with lipid-encapsulated Mycobacterium bovis BCG: anatomical sites of bacterial replication and immune activity. Immunol Cell Biol 2005;83(5):549–53. [21] Aldwell FE, Cross ML, Fitzpatrick CE, Lambeth MR, de Lisle GW, Buddle BM. Oral delivery of lipid-encapsulated Mycobacterium bovis BCG extends survival of the bacillus in vivo and induces a long-term protective immune response against tuberculosis. Vaccine 2006;24(12):2071–8. [22] Aldwell FE, Brandt L, Fitzpatrick C, Orme IM. Mice fed lipid-encapsulated Mycobacterium bovis BCG are protected against aerosol challenge with Mycobacterium tuberculosis. Infect Immun 2005;73(3):1903–5. 6272 L.A.L. Corner et al. / Vaccine 28 (2010) 6265–6272 [23] Clark S, Cross ML, Nadian A, Vipond J, Court P, Williams A, et al. Oral vaccination of guinea pigs with a Mycobacterium bovis bacillus Calmette–Guerin vaccine in a lipid matrix protects against aerosol infection with virulent M. bovis. Infect Immun 2008;76(8):3771–6. [24] Clark S, Cross ML, Smith A, Court P, Vipond J, Nadian A, et al. Assessment of different formulations of oral Mycobacterium bovis bacille Calmette–Guerin (BCG) vaccine in rodent models for immunogenicity and protection against aerosol challenge with M. bovis. Vaccine 2008;26(46): 5791–7. [25] Wedlock DN, Aldwell FE, Keen D, Skinner MA, Buddle BM. Oral vaccination of brushtail possums (Tichosurus vulpecula) with BCG: immune responses, persistence of BCG in lymphoid organs and excretion in faeces. N Z Vet J 2005;53(5):301–6. [26] Buddle BM, Aldwell FE, Skinner MA, de Lisle GW, Denis M, Vordermeier HM, et al. Effect of oral vaccination of cattle with lipid-formulated BCG on immune responses and protection against bovine tuberculosis. Vaccine 2005;23(27):3581–9. [27] Corner LA, Norton S, Buddle BM, Morris RS. The efficacy of bacille Calmette–Guerin vaccine in wild brushtail possums (Trichosurus vulpecula). Res Vet Sci 2002;73(2):145–52. [28] Report of a WHO/FAO/OIE Consultation on Animal Tuberculosis Vaccines. Geneva; 1994. [29] Corner LA, Costello E, Lesellier S, O’Meara D, Sleeman DP, Gormley E. Experimental tuberculosis in the European badger (Meles meles) after endobronchial inoculation of Mycobacterium bovis: I. Pathology and bacteriology. Res Vet Sci 2007;83(1):53–62. [30] Gavier-Widen D, Chambers MA, Palmer N, Newell DG, Hewinson RG. Pathology of natural Mycobacterium bovis infection in European badgers (Meles meles) and its relationship with bacterial excretion. Vet Rec 2001;148(10): 299–304. [31] Collins CH, Grange JM, Yates MD. Tuberculosis bacteriology: organisation and practice. 2nd ed. Oxford; 1997. [32] Kamerbeek J, Schouls L, Kolk A, van Agterveld M, van Soolingen D, Kuijper S, et al. Simultaneous detection and strain differentiation of Mycobacterium tuberculosis for diagnosis and epidemiology. J Clin Microbiol 1997;35(4): 907–14. [33] Dalley D, Chambers MA, Cockle P, Pressling W, Gavier-Widen D, Hewinson RG. A lymphocyte transformation assay for the detection of Mycobacterium bovis infection in the Eurasian badger (Meles meles). Vet Immunol Immunopathol 1999;70(1–2):85–94. [34] Dalley D, Dave D, Lesellier S, Palmer S, Crawshaw T, Hewinson RG, et al. Development and evaluation of a gamma-interferon assay for tuberculosis in badgers (Meles meles). Tuberculosis (Edinb) 2008;88(3):235–43. [35] Lesellier S, Palmer S, Dalley DJ, Dave D, Johnson L, Hewinson RG, et al. The safety and immunogenicity of bacillus Calmette–Guerin (BCG) vaccine in European badgers (Meles meles). Vet Immunol Immunopathol 2006;112(1–2):24–37. [36] Gallagher J, Monies R, Gavier-Widen M, Rule B. Role of infected, nondiseased badgers in the pathogenesis of tuberculosis in the badger. Vet Rec 1998;142(26):710–4. [37] Gavier-Widen D, Cooke MM, Gallagher J, Chambers MA, Gortazar C. A review of infection of wildlife hosts with Mycobacterium bovis and the diagnostic difficulties of the ‘no visible lesion’ presentation. N Z Vet J 2009;57(3):122–31. [38] Lesellier S, Corner L, Costello E, Lyashchenko K, Greenwald R, Esfandiari J, et al. Immunological responses and protective immunity in BCG vaccinated badgers following endobronchial infection with Mycobacterium bovis. Vaccine 2009;27(3):402–9. [39] Lesellier S, Corner L, Costello E, Sleeman P, Lyashchenko KP, Greenwald R, et al. Immunological responses following experimental endobronchial infection of badgers (Meles meles) with different doses of Mycobacterium bovis. Vet Immunol Immunopathol 2009;127(1–2):174–80. [40] Southey A, Sleeman DP, Lloyd K, Dalley D, Chambers MA, Hewinson RG, et al. Immunological responses of Eurasian badgers (Meles meles) vaccinated with Mycobacterium bovis BCG (bacillus Calmette Guerin). Vet Immunol Immunopathol 2001;79(3–4):197–207. [41] Power CA, Wei G, Bretscher PA. Mycobacterial dose defines the Th1/Th2 nature of the immune response independently of whether immunization is administered by the intravenous, subcutaneous, or intradermal route. Infect Immun 1998;66(12):5743–50. [42] Vordermeier HM, Chambers MA, Cockle PJ, Whelan AO, Simmons J, Hewinson RG. Correlation of ESAT-6-specific gamma interferon production with pathology in cattle following Mycobacterium bovis BCG vaccination against experimental bovine tuberculosis. Infect Immun 2002;70(6):3026–32.