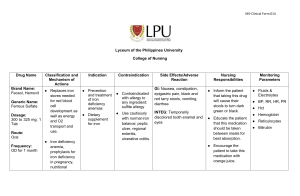
Lilley: Pharmacology and the Nursing Process, 10th Edition Chapter 54: Anemia Drugs Key Points Anatomy, Physiology, and Pathophysiology Overview The formation of new blood cells is one of the primary functions of bones. This process is known as hematopoiesis, and it includes the production of erythrocytes, as well as leukocytes and thrombocytes. This process takes place in the myeloid tissue or bone marrow. Erythropoiesis is the process of erythrocyte formation. When red blood cells (RBCs) are manufactured in the bone marrow by myeloid tissue, they are released into the circulation as immature RBCs called reticulocytes. Once in the circulation, reticulocytes undergo a 24- to 36-hour maturation process to become mature, fully functional RBCs. After this, they have a lifespan of about 120 days. More than one third of an RBC is composed of hemoglobin. Hemoglobin (abbreviated Hgb) is composed of two parts: heme and globin. Heme is a red pigment. Each heme group contains one atom of iron. Globin is a protein chain. Types of Anemia Anemias are classified into four main types based on the underlying causes. Anemia of chronic disease is another common type of anemia. Anemias can be caused by maturation defects or can be secondary to excessive RBC destruction. Excessive RBC destruction can be either intrinsic or extrinsic. Two types of maturation defects lead to anemias, categorized by the location of the defect within the cell: cytoplasmic maturation defects occur in the cell cytoplasm, and nuclear maturation defects occur in the cell nucleus. Major examples of anemias arising from cytoplasmic maturation defects include irondeficiency anemia and genetic disorders such as thalassemia, which result in defective globin synthesis. For each of these anemias, the RBCs appear hypochromic (lighter red than normal) and microcytic (smaller than normal) on blood smear. Pernicious anemia results from deficiency of vitamin B12, which is used in the formation of new RBCs. The usual underlying cause is the failure of the stomach lining to produce intrinsic factor. Both pernicious anemia and folic acid deficiency anemia are also known as types of megaloblastic anemia, because they are both characterized by large, immature RBCs. Megaloblastic anemias not caused from a lack of intrinsic factor are usually related to poor dietary intake and are most commonly seen in infancy, childhood, and pregnancy. Some types of anemias arise from excessive RBC destruction (hemolytic anemias). These can occur because of abnormalities within the RBCs themselves (intrinsic factors) or as a result of factors outside of (extrinsic to) the RBCs. In both cases, the erythrocytes appear on blood smear as spherocytes. Pharmacology Overview Key Points 54-2 Erythropoiesis-Stimulating Agents Blood-forming drugs are often used in the treatment of pernicious anemia, malabsorption syndromes, hemolytic anemias, hemorrhage, and renal and liver diseases. Epoetin alfa (Epogen) is a biosynthetic form of the natural hormone erythropoietin, which is normally secreted by the kidneys in response to a decrease in RBCs. It promotes the synthesis of erythrocytes (RBCs) by stimulating RBC progenitor cells in the bone marrow. Epoetin alfa is used to treat anemia that is associated with end-stage renal disease, chemotherapy-induced anemia, and for anemia associated with zidovudine therapy. Erythropoiesis-stimulating agents are ineffective without adequate body iron stores. Most patients receiving epoetin alfa also need to receive an oral iron preparation. A longer-acting form of epoetin called darbepoetin (Aranesp) is also available and a biosimilar product, Retacrit is also available and is dosed the same as Epogen or Procrit. Use of epoetin and darbepoetin is contraindicated in cases of uncontrolled hypertension and when hemoglobin levels are above 10 g/dL for cancer patients and 12 g/dL for renal patients. Use in patients with head or neck cancers or patients at risk for thrombosis is controversial as these medications increase tumor growth and risk for thrombosis. The Food and Drug Administration (FDA) issued a public health advisory regarding the overzealous use of epoetin. It was found that when hemoglobin levels are above 12 g/dL and the drug is continued, patients experienced serious adverse events, including heart attack, stroke, and death. Abuse of erythropoietin by athletes hoping to increase oxygen-carrying capacity and improve performance places them at risk for diseases caused by increased blood viscosity (stroke, myocardial infarction). All erythropoietin drugs carry a black box warning regarding these potential adverse effects. Iron Iron is a mineral that is essential for the proper function of all biologic systems in the body. It is stored in many sites (liver, spleen, and bone marrow). Deficiency of this mineral is the principal nutritional deficiency resulting in anemia. Individuals who require the highest amount of iron are women (especially pregnant women) and children, and they are the groups most likely to develop iron-deficiency anemia. Iron and folic acid are very important in the treatment of many disorders and diseases (e.g., malignancies) to achieve RBC and hemoglobin formation that is as adequate as possible and to help prevent nutritional deficits that can affect all body systems, especially the immune system. Oral iron preparations are available as ferrous salts. There are four injectable iron products available: iron dextran (INFeD), iron sucrose (Venofer), ferric gluconate (Ferrlecit, Nulecit), and ferumoxytol (Feraheme). Because of the potential of iron dextran to cause anaphylaxis, its use has been replaced by use of the newer products, ferric gluconate and iron sucrose. Iron dextran is available only for injection. The newest injectable iron product is ferumoxytol (Feraheme). It offers the advantage of being given undiluted as IV push in 1 minute. Key Points 54-3 Administration of iron corrects iron-deficiency symptoms such as anemia, dysphagia, dystrophy of the nails and skin, and fissuring of the angles of the lips. Supplemental iron contained in multivitamins plus iron or iron supplements alone are indicated for the prevention or treatment of iron-deficiency anemia. In all cases, an underlying cause needs to be identified and treated. Contraindications to the use of iron products include known drug allergy, hemochromatosis (iron overload), hemolytic anemia, and any other anemia not associated with iron deficiency. Iron supplementation is also used in erythropoietin therapy because it is essential for the production of RBCs. The most common adverse effects associated with oral iron preparations are nausea, vomiting, diarrhea, constipation, stomach cramps, and stomach pain. Excess iron intake can lead to accumulation and iron toxicity. Iron overdose is the most common cause of pediatric poisoning deaths reported to U.S. poison control centers. Toxicity from iron ingestion results from a combination of the corrosive effects on the gastrointestinal mucosa and the metabolic and hemodynamic effects caused by the presence of excessive elemental iron. Treatment of iron overdose is based on symptomatic and supportive measures, including suction and maintenance of the airway, correction of acidosis, and control of shock and dehydration with intravenous fluids or blood, oxygen, and vasopressors. In patients with severe symptoms of iron intoxication, such as coma, shock, or seizures, chelation therapy with deferoxamine is initiated. Iron absorption is enhanced when given with ascorbic acid and decreased when given with antacids and calcium. Iron preparations can decrease the absorption of certain antibiotics, including tetracyclines and quinolones. Iron products are contraindicated with known drug allergy and in patients with ulcerative colitis and regional enteritis, conditions of excessive body iron stores (e.g., hemosiderosis, hemochromatosis), peptic ulcer disease, cirrhosis, gastritis, esophagitis, hemolytic anemia, and any other anemia not associated with iron deficiency. Goals of therapy include maintenance of normal hemoglobin and hematocrit levels and energy level. Folic Acid Because folic acid is absorbed in the upper duodenum, malabsorption syndromes are the most common cause of deficiency. Folic acid is converted in the body to tetrahydrofolic acid, which is used for erythropoiesis and for synthesis of nucleic acids (deoxyribonucleic acid [DNA] and ribonucleic acid [RNA]). Dietary ingestion of folate is required for the production of DNA and RNA. It is also essential for normal erythropoiesis. Anemias caused by folic acid deficiency are treated with folic acid. There is much evidence to support the use of folic acid in the prevention of neural tube defects such as spina bifida, anencephaly, and encephalocele. Folic acid is also indicated for the treatment of tropical sprue, a malabsorption syndrome. Key Points 54-4 Other Anemia Drugs Cyanocobalamin (vitamin B12) is used to treat pernicious anemia and other megaloblastic anemias. It can be given orally or intranasally to treat vitamin B12 deficiency but is usually given by deep intramuscular injection to treat pernicious anemia. Nursing Process Assess for and document any signs and symptoms of anemia, such as difficulty swallowing, changes in nails and skin, and fissuring/cracking of the angles of the lip. Before any drug is given to treat anemia, assess the patient’s past and present medical history; compile a medication profile, including all prescriptions, OTC, and herbal medications the patient is taking; and assess for drug allergies. Perform a nutritional assessment with a focus on the amount of iron in the patient’s diet. Ask questions about the patient’s energy levels, ability to carry out activities of daily living, overall immunity to illnesses, and state of health. Have patients sip oral iron through a plastic straw to avoid discoloration of tooth enamel. Oral forms of iron need to be given with plenty of fluids but not with antacids or milk, and preferably not with meals, because of the risk for decreased absorption of the drug. Parenteral dosage forms may cause anaphylaxis and orthostatic hypotension. It may be necessary for the patient to remain recumbent for 30 minutes after the intravenous injection to prevent drug-induced orthostatic hypotension. Keep epinephrine and resuscitative equipment available in case of anaphylactic reaction. Therapeutic responses to iron products include improved nutritional status, increased weight, increased activity tolerance and well-being, and absence of fatigue. Adverse effects of iron products include nausea, constipation, epigastric pain, black and tarry stools, and vomiting. Signs of toxicity include nausea, diarrhea, hematemesis, pallor, cyanosis, shock, and coma. Instruct patients to take iron products exactly as ordered. Parenteral dosage forms may cause anaphylaxis and orthostatic hypotension. Be aware of the potential for poisoning if these drugs are taken in greater than the recommended amounts. Oral iron products must be taken in their original dosage form without alteration.