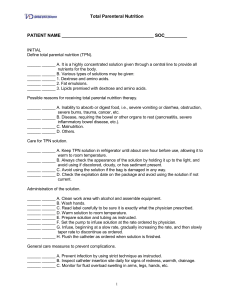
Exam 2 Powerpoint Notes Titrated Meds: ● Critically ill patients given potent medication thru IV process called titration ● Titrated meds are added to a specific amount of fluid and adjusted to infuse at a rate to reach desired effect ● Types of Titrated meds: antiarrhythmics (Diltiazem), Vasopressors (Norepinephrine), Vasodilators (Nitroglycerin), Sedatives (Propofol), Analgesics (Morphine), Anticoagulants (Heparin) ● Titrated Medications are ordered with parameters for desired outcomes, each medication varies. ● General Guidelines: ❖ Monitor closely due to potency, small changes can affect the patient rapidly ❖ Usually started at lowest dose then adjusted up or down, higher doses can be used first by physician order ❖ Must follow med protocol & facility protocols ❖ Dose is determined by physician or practitioner ❖ Never exceed upper dose limit without physician’s order ❖ Titrations are performed based on the assessment findings of the patient ● Med Errors: ❖ Can be fatal. ❖ Should be checked by another nurse. ❖ Nurses need to have knowledge of: the medication, proper dosage, proper dosage adjustment, calculations for dosing and adjustments, frequency of adjustments/titrations, and usage of the IV pumps at the facility ● IV Pumps: ❖ smart pump have a library for medications, dose, volumes to choose from ❖ Nurse should always verify medication dose/rate regardless of pump, titrated medications need to be verified by 2 nurses ❖ If medication/dose/volume/rate cannot be found on pump, nurse should run basic infusion and input information manually ● Bolus is given for fast reaction or emergency & drip is continued after for maintenance ● Nursing Responsibilities ❖ Check IV med compatibility ❖ Obtain baseline vitals ❖ Find appropriate IV pump/ears ❖ Check patency of patient’s IV sites ❖ Know drug actions, dosing, side and adverse effects ❖ Monitor vital signs and perform appropriate assessments per protocols (typically 15 minutes after infusion has started. May be every 15 minutes x 4, then every 30 minutes x 2, then every hour x 4. ❖ Know which medications can be administered on your unit. (ER & ICU can give all titrated medications. Med-Surg and Tele units may only be able to administer these medications, but not titrate them). ❖ If a medication cannot be administered safely on your unit, they will need to transfer to the appropriate area for that medication to be initiated. Blood Draw from Central Line: ● Types of CVAD ❖ Peripherally Inserted Central Catheter (PICC): through the basilic, cephalic, or median cubital veins of the arm ❖ Central Venous Catheter (CVC): inserted through the subclavian vein or the internal and external jugular veins which terminate in the superior vena cava or inserted through the femoral vein where the catheter is threaded into the inferior vena cava. Both are used for short term therapy. ❖ Tunneled Central Venous Catheters(TCVC): for long term therapy; inserted surgically with tip in the superior vena cava; catheter exits through the chest or abdomen ❖ Implanted subcutaneous vascular access ports or devices (VAP or VAD)functions in the same manner as a TCVC; implantable port with no exit sites. Consists of a single or double port with a self sealing septum that is connected to a catheter. The distal end of the catheter is positioned in the superior vena cava. ● People that can draw blood from a central line: ❖ Nurses ❖ Physicians ❖ Interventional Radiologist (IR) Specialists ❖ Health care providers with specialized training and/or certifications ● Contraindications: ❖ Assess: when was the last time it was accessed, by whom? What medication(s) have they been receiving through it? Any issues? ➔ Depending on what the patient or family member report to you, you may not be able to draw blood from their central line ❖ Chemotherapy—need order from an MD ❖ Dialysis-need an order from an MD, requires specialized teaching and/or certifications ● Equipment: ❖ Flushes ❖ several 5-10 ml syringes ❖ Vacutainer Blood Transfer Device with Luer Adapter ❖ Large bore needles ❖ Alcohol pads (or hospital policy prep pads) ❖ Masks on yourself and/or the patient (coughing patients, neutropenic precautions, isolation) ❖ Blood tubes ❖ Specimen label(s) ❖ WOW (to scan in specimens for documentation) depending on hospital policy/equipment ● ● ● ● ❖ Remote lab specimen scanner (to scan in specimens for documentation) depending on hospital policy/equipment Flushing Central Line ❖ Flushing is the most important mechanism used to maintain the patency of a central line and prevent occlusion. ❖ If resistance is met, never force the irrigant into the line. ❖ Always use a 5-10cc syringe depending on hospital policy. Smaller syringes exert more pressure and can cause the catheter to rupture. ❖ After every use: Flush the lumen with 10 mls of saline (or whatever hospital policy designates) ❖ For non used lumens: Flush with saline and heparin per hospital policy. It may be once a shift or every 12 hours. ❖ When flushing the line, the push-pause method should be used rather than the continual, even push of saline into the catheter. ❖ The continual push method is a non turbulent movement of fluid in a single direction and may not remove particles that adhere to the catheter lumen. ❖ Whereas the push-pause method creates turbulence with a swirling effect inside the catheter lumen, thus removing fibrin and other residues of medications. Triple Lumen Port ❖ Each lumen exits at proximally different points of the catheter ❖ Proximal port: blood administration and withdrawal ❖ Middle port: TPN & lipids ❖ Distal port: IVPB, IVP, & CVP monitoring Blood Draw Methods ❖ Waste/Discard method: involves aspirating at least 6 mLs blood with a syringe then discarding that sample; followed by the use of a new syringe for specimen collection. ❖ Push/Pull or Flush then Waste method: involves flushing with saline, then aspirating a predetermined amount of blood to waste/discard; followed by using separate equipment for the blood specimen collection. (This is the method most widely used in the hospitals in our communities; which we will use) ❖ Reinfusion method: involves attaching a syringe, aspirating blood into the syringe, re-infusing that blood, and without disconnecting that syringe, repeating the process three times. After this procedure, then a new syringe is attached to collect the needed blood specimen(s). This method was meant for blood conservation. ❖ Dead Space method: involves aspirating two times the amount of dead space with a syringe then discarding that sample. If the line is heparinized, then aspirate 6 times the dead space; followed by the use of a new syringe for specimen collection. Blood Draw Procedure ❖ Verify Physician order ❖ Assemble equipment/ Hand Hygiene/ Don PPE required for patient ❖ Identify patient TPN ● ● A hypertonic solution containing 20% to 50% dextrose, proteins, vitamins, and minerals that is administered into the venous system. ❖ Explain procedure to patient ❖ Position patient with central line site below the heart ❖ Clamp catheter to be accessed (Not necessary if using power caps) ❖ Stop all other infusions (if applicable) ❖ Remove alcohol based cap from port ❖ Cleanse port with alcohol swab for 15 seconds ❖ Attach flush, Unclamp line (Not necessary if using power caps) ❖ Flush line with 0.5-1 mL of saline ❖ Aspirate for blood return to check placement ❖ If able to aspirate for blood return, flush remaining mLs of saline over 1 minute ❖ Depending on hospital policy, you will either: ❖ Draw back at least 6 mL of blood with the flush syringe to discard OR ❖ Clamp the line, remove the empty syringe, attach a Vacutainer Blood Transfer Device With Luer ❖ Adapter, and connect 1-2 blood tubes (6-12 mLs) to use as initial waste ❖ Depending on hospital policy, you will then either: ❖ Attach new syringes and continue to draw the amount of blood you need OR ❖ Collect samples of blood you need by connecting blood tubes to the Vacutainer Blood Transfer Device With Luer Adapter ❖ The order of the tubes you collect will be based on hospital policy ❖ If you are collecting blood with syringes, the amount of blood you will need to collect will say in mLs on the blood tubes ❖ Clamp the line when you have collected enough blood for your specimens (Not necessary if using power caps) ❖ Flush the line with 10-20 mLs of saline using the push-pause method or per hospital policy ❖ Clamp the line (Not necessary if using power caps) ❖ Apply a new alcohol-based cap If you are collecting blood with syringes, you will then need to attach a large bore needle or a blood draw vacutainer and fill the appropriate blood tubes ❖ Label the specimen, Place in a biohazard bag, & Take or send to lab Additional Info ❖ Do not use syringes less than 5 mL to aspirate blood as a smaller syringe may ❖ fracture the catheter ❖ Avoid drawing specimens from lines that have TPN infusing ❖ Heparin should not be used prior to blood specimen collection ❖ Some CVC lines will follow the SASH, SAS, or AS methods ❖ S = saline ❖ A = antibiotic ❖ H = heparin ● ● ● ● TPN is indicated when there is interference with nutrient absorption from the gastrointestinal tract or when complete bowel rest is necessary for healing. TPN can only be administered through central venous access. TPN must be administered through tubing with an in-line filter and controlled with an electronic infusion device. Complications for which monitoring is needed include: ❖ Pneumothorax ❖ Air embolism ❖ Infection ❖ Fluid overload ❖ Metabolic complications NOTES FROM CLASS TPN ● ● ● ● ● ● ● ● ● Proximal catheter- blood Medial catheter- TPN Distal- drugs/medications Goes in subclavian TPN tubing only good for 24 hrs because bacteria can grow We monitor electrolytes in patients receiving TPN, imbalance of electrolytes can cause arrhythmias Filter must be used for lipids, to prevent fat embolisms Egg allergies with lipids, should not be administered TPN should be given by itself, never given with anything else CVAD ● Used at least 5 ml to 10 ml syringe for meds Drugs ● Lispro ❖ rapid acting insulin, Do not give until you have a tray, SUB Q route, can cause Hypoglycemia ● Monitor these labs when giving: ❖ Heparin- PTT ❖ Coumadin PT,INR ● Nitro ❖ comes in glass bottle ❖ Used for chest pain ❖ Sensitive to light ❖ Glass is not breathable (Tubing has opening so you can squeeze liquid into chamber, leave open) ● Protonix: Dilute in 10mL’s ● ❖ Push over 2 minutes and flush for same amount of time KCL ❖ Can cause burning at IV site ❖ Can cause arrhythmias INCOMPATIBILITIES ● Protonix not compatible with Flagyl ● Flagyl compatible with Ancef but should not be given together ● Do not piggyback anything with electrolytes EX: POTASSIUM SIM NOTES: ● Always ID patient, perform hand hygiene, introduce yourself to patient & family ● Explain everything you are doing as you go ● Assessment: ❖ lines/tubes/drains (running meds/dressings/SCDs/oxygen/suction/etc) ❖ Focused assessment depending on patient’s condition ❖ Baseline vitals/glucose ❖ Ask about pain/bowel/urine ❖ Check labs before administering meds ❖ Always reassess pain/bp after medications ❖ Use proper body mechanics, have bed up ❖ Address pain before anything else ❖ LISTEN TO YOUR PATIENT ● CVAD: ❖ Never leave CVAD open to air, keep clamped until you are pushing/flushing ❖ Always scrub with alcohol for 15 seconds between everything ❖ Pull back for blood return & to check patency MINI EXAM 2 REVIEW 3/3 ● Titrated meds: ❖ Math for heparin, VTBI, weight based heparin, weight x kg per min, ● Central Lines: ❖ SATA: nursing responsibilities ❖ Patency, clean, dry ❖ Where central line catheter tip is located and where it goes ❖ What to do if you can't flush a CVAD (call MD and label lumen do not use) ❖ NO IVP through lumen of TPN ❖ Proper technique of solumedrol ❖ Proper syringe size ( 5 to 10 ml) ❖ waste/discard method for blood draw ❖ Why we waste the 1st 6 ml of blood ❖ valsalva maneuver ● TPN: ❖ PPN vs TPN ❖ Nursing responsibilities (monitoring/strict I&O/micron filter/weight/glucose) ❖ Complications: infection, hypo/hyperglycemia, labs Nursing Responsibilities of the central line when giving medication through a central line? 5-10 ml syringe check for blood return Push pause method where is the tip of the central line located? superior vena cava patient does not have a positive pressure cap? what are some things you have to be careful when pushing a medication? make sure it's a clamp before removing syringe, clean, puts around, unclamp, close clamp before removing syringe. how can you have your patient help you prevent an embolism? valsalva maneuver I be piggyback medications what are some things we have to do before we give it? check compatibility. assess for fluid overload ( crackles, edema, jugular vein distention) central line ports, if a port is not being used, and you had to give us give Solu-Medrol what do you do start to finish? 1) assess site 2) Clean 3) 5-10mL flush 4) blood return to check for placement 5) and still remaining Saline 6) give medication 7) flush with 10 mL unable to flush PICC line? don't use it label it, notify physician lesson learned on Mary Banks? pain medication first, to see if pain was causing high blood pressure. medications cannot be given through the same port that the tpn is running from. why do we need to use 5-10 ml syringe? anything less than five will break the catheter three nursing assessments for patients everyday? Strict I&O , glucose q6 , micron filter Difference between PPN and tpn? TPN: fat concentration is higher, more dextrose ( check for hyperkalemia and hyperglycemia) if Pharmacy is late with tpn? hang a D5 or d10 risk for lipid therapy? fat embolism What 3 methods are acceptable for drawing blood? Reinfusion method, waste discard, where can nurses draw blood from? PICC line, Central line, peripheral, port. NEVER!!!!!!!!! From dialysis port Nitroglycerin: very potent vasodilator ( Nitroglycerin headache normal) Tylenol gets it to go away only., needs vented tubing, sublingual tab sensitive to light. * monitor vital signs given for chest pain have saline ready