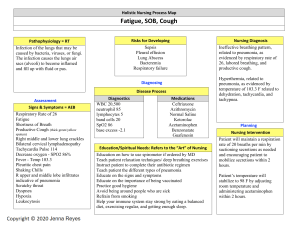
Respiratory System Dr. SITESH Kr. SAH RESPIRATORY SYSTEM: OVERVIEW The respiratory system is the network of Tissues and Organs that help breathe. Parts: Nose. Mouth. Throat (pharynx) Voice box (larynx) Windpipe (trachea) Airways (bronchi) Lungs. Definition: Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing PROGRESS OF INFECTION: Most of the time, the body filters organisms, and keeps the lungs healthy. But sometimes body fails to filter the organisms, It enter the lungs and cause infections. • The microorganism reaches the lungs by: —Inhalation or aspiration —Hematogenious way —Direct invasion from the neighbouring tissues SEVERITY OF INFECTION: The amount of the organism inoculated, The virulance factors and The immunity of the host Risk factors Pneumonia can affect anyone. But the two age groups at highest risk are: 1. Children who are 2 years old or younger 2. People who are age 65 or older RISK FACTOR IN ADULT Being hospitalized: greater risk in a hospital intensive care unit, especially if on a ventilator. Chronic disease: more likely with asthma, chronic obstructive pulmonary disease (COPD) or heart disease. Smoking. Smoking damages your body's natural defenses against the bacteria and viruses that cause pneumonia. Weakened or suppressed immune system. People who have HIV/AIDS, who've had an organ transplant, or who receive chemotherapy or long-term steroids are at risk. Alcohol : Daily alcohol consmption Corticosteroid therapy for Past 3 months Old age: Age >65 is at higher risk RISK FACTOR IN CHILDREN Classifications: CLINICAL CLASSIFICATION: 1. Community-acquired: defined as pneumonia that is acquired outside the hospital. The most commonly identified pathogens are Streptococcus pneumoniae, Haemophilus influenzae, atypical bacteria 2. Hospital-acquired: occurs during a hospital stay. This type of pneumonia can be very severe. Sometimes, it can be fatal. 3. Aspiration pneumonia: occurs when food or liquid is breathed into the airways or lungs, instead of being swallowed. ANATOMICAL CLASSIFICATION : 1. Bronchopneumonia 2. Lobar pneumonia 3. Interstitial pneumonia • ETIOLOGICAL CLASSIFICATION 1. Bacterial 2. Viral 3. Fungal ANATOMICAL CLASSIFICATION Bronchopneumonia affects the lungs in patches around bronchi (affects the bronchi in the lungs) Lobar pneumonia is an infection that only involves a single lobe, or section, of a lung. Interstitial pneumonia involves the areas in between the alveoli Etiology: Bacteria: Streptococcus pneumonia (50% Cases) Haemophilus influenzae (20% Cases) Chlamydophila pneumoniae (3% Cases) Mycoplasma pneumoniae (3% Cases) ETIOLOGY Viruses: • In adults: one third of pneumonia cases, and • In children: about 15% Common agents : rhinoviruses, coronaviruses, influenza virus, respiratory syncytial virus (RSV), adenovirus, and parainfluenza. Notes: organ transplantation and immunocompromised persons,: cytomegalovirus pneumonia. Fungus: • Fungal pneumonia is uncommon, • Occurs commonly in weakened immune systems due to AIDS, immunosuppressive drugs, or other medical problems. Common agents: Histoplasma capsulatum, Blastomyces, Cryptococcus neoformans, Pneumocystis jiroveci (pneumocystis pneumonia, or PCP), and Coccidioides immitis Diagnosis: Medical history: Physical exam: Laboratory investigation: Radiological investigation: Others investigation: CLINICAL EVALUATION: MEDICAL HISTORY Fever, sweating and shaking chills Cough, which may produce greenish, yellow or even bloody mucus Shortness of breath Rapid, shallow breathing Other Clinical Manifestation: The signs and symptoms of pneumonia may include: Sharp or stabbing chest pain that gets worse when you breathe deeply or cough Loss of appetite, low energy, and fatigue Nausea and vomiting, especially in small children Confusion, especially in older people PHYSICAL EXAMINATION: GENERAL EXAM: • High fever, • Tachicardia, • Tachypnea, • Hypotension, • Confusion, • Drowsiness, • Altered mental status • Cyanosis RESPIRATORY SYSTEM: • Inspection: — Usually normal — Ortopnea — Respiratory disstress • Palpation — increased Vibration thoracic (lober pneumonia) — Decreased hemithoracal movement • • Percution — Normal sonority — Dullness (Matite) Oscultation — End inspiratory fine crackles — Local diminished breath sounds — Bronchial voice Laboratory investigation Complete Blood Count: Arterial Blood Gasses. Blood Culture. Pleural fluid culture Sputum Tests. Gram Staining (A Gram stain is a test that checks for bacteria at the site of a suspected infection such as the throat, lungs, genitals, or in skin wounds. Gram stains may also be used to check for bacteria in certain body fluids, such as blood or urine. AFB (acid-fast bacillus) a type of bacteria that causes tuberculosis and certain other infections. Giemsa or methenamine silver stain KOH (potassium hydroxide) mount (Presence of Fungus) RADIOLOGICAL EXAMINATION: X-ray: SUGGESTIVE FEATURE OF BACTERIAL LRI SUGGESTIVE FEATURE OF VIRAL LRI OTHERS INVESTIGATION: Pulse Oximetry: CT Scan. Bronchoscopy Thoracoscopy Percutaneous aspiration/biopsy Open lung biopsy GENERAL MANAGEMENT AT HOME FEVER: Treat with aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs, such as ibuprofen or naproxen), or acetaminophen. DO NOT give aspirin to children. Drink plenty of fluids to help loosen secretions and bring up phlegm. Do not take cough medicines : Coughing is one way your body works to get rid of an infection, UNLESS cough is preventing you from getting the rest you need. Drink warm beverages: take steamy baths and use a humidifier to help open your airways and ease your breathing. Stay away from smoke: Let your lungs heal. This includes smoking, secondhand smoke and wood smoke. This would be a good time to think about quitting for good. Get lots of rest:You may need to stay in bed for a while. Get as much help as you can with meal preparation and household works until you are feeling stronger. AT HOSPITAL: OPD /ER SEVERITY ASSESSMENT In child In old age 20 mg/dL >30 breaths <90/60 CURB 65 C onfusion – Altered mental status U remia – Blood urea nitrogen (BUN) level greater than 20 mg/dL R espiratory rate –30 breaths or more per minute B lood pressure – Systolic pressure less than 90 mm Hg or diastolic pressure less than 60 mm Hg Age older than 65 years Score evaluation and treatment : Score of 0-1 – Outpatient treatment Score of 2 – Admission to hospital(No ICU) Score of 3 or higher – Admission to intensive care unit (ICU) Outpatient Treatment: Outpatients Treatment(empirical): For MILD Pneumonia and CURB 65 Score of 1 Previously healthy and no antibiotics in past 3 months : Treat for 7days AMOXICILLIN – 1 gm TDS Plus MACROLIDE (clarithromycin 500 mg BID) OR Respiratory FLUOROQUINOLONES [moxifloxacin ,levofloxacin ] OR DOXYCYCLINE 200 Mg STAT then 100 Mg BID Comorbidities or antibiotics in past 3 months: AMOXICILLIN – 1 gm TDS / AUGMENTIN 625 Mg- TDS Plus MACROLIDE (clarithromycin 500 mg BID/ Azithromycin- 500 Mg OD) Respiratory FLUOROQUINOLONES [moxifloxacin 400 Mg OD ,levofloxacin 750 Mg OD ] MILD PNEUMONIA INDICATION FOR ADMISSION , Severe Pneumonia in children And CURB 65 Score of 2 in older Inpatients, Non- ICU IV fluoroquinolone [moxifloxacin-400 mg OD ,levofloxacin- 750 Mg OD] OR IV AMOXICILLIN or AUGMENTIN plus a macrolide [IV clarithromycin or azithromycin) Inpatients, ICU • IV β -lactam (ceftriaxone – 1 gm BID ) plus • IV Azithromycin OR • IV fluoroquinolone Pseudomonas IV β-lactam [piperacillin/tazobactam OR cefepime )plus IV flouroquinolons [levofloxacin -750 mg IV OD ] Methicillin-resistant Staphylococcus aureus (MRSA) add linezolid or vancomycin ASSPIRATION PNEUMONIA: IV CLINDAMYCIN 600 Mg TID OR IV CEFTRIAXONE 1 gm OD plus METRONIDAZOLE 500 Mg QID OR PIPERACILLINE-TAZOBACTUM 4.5 Gm QID EMPHYEMA: IV- CLINDAMYCIN 600 Mg TID Plus CEFTRIAXONE 1 gm OD OR CEFEPIME 2 Gm BID IV CEFTRIAXONE 1 gm OD plus METRONIDAZOLE 500 Mg QID/1 Gm BID OR PIPERACILLINE-TAZOBACTUM 4.5 Gm QID Complications: Bacteria in the bloodstream (bacteremia). Bacteria that enter the bloodstream from your lungs can spread the infection to other organs, potentially causing organ failure. Difficulty breathing. If your pneumonia is severe or you have chronic underlying lung diseases, you may have trouble breathing in enough oxygen.You may need to be hospitalized and use a ventilator while your lung heals. Fluid accumulation around the lungs (pleural effusion). Pneumonia may cause fluid to build up in the thin space between layers of tissue that line the lungs and chest cavity (pleura). If the fluid becomes infected, you may need to have it drained through a chest tube or removed with surgery. Lung abscess. An abscess occurs if pus forms in a cavity in the lung. An abscess is usually treated with antibiotics. Sometimes, surgery or drainage with a long needle or tube placed into the abscess is needed to remove the pus. Pleurisy. Septic arthritis. Endocarditis.