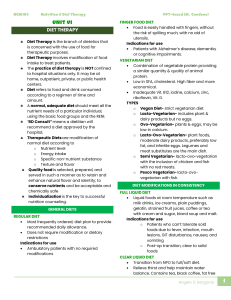
LECTURE | 2ND SEMESTER | FINALS | WEEK 11 CANCER ▶ diseases characterized by the uncontrolled growth of a group of abnormal cells, which can destroy adjacent tissues and spread to other areas of the body via the lymph or blood. CARCINOGENESIS: The development of cancer TUMOR (NEOPLASM): abnormal mass of cells ▶ a network of blood vessels forms to supply the tumor with the nutrients it needs to support its growth. ▶ tumor can disrupt the functioning of the normal tissue around it, and some tumor cells may metastasize, spreading to other regions in the body. APOPTOSIS: program cell death CARCINOGENS: cancer-causing substances, may induce genetic mutations that lead to cancer NURTITION AND CANCER RISK NUTRITION-RELATED FACTORS THAT INFLUENCE CANCER RISK FACTORS THAT MAY INCREASE CANCER RISK Obesity Esophagus, stomach, colon, rectum, pancreas, liver, gallbladder, kidney, breast (postmenopausal), ovary, endometrium, prostate Red meat, Colon, rectum processed meats Salted and saltStomach preserved foods Beta-carotene supplements High-calcium diets (over 1500 mg daily) Prostate Alcoholc Lungb Mouth, pharynx, larynx, esophagus, stomach, colon, rectum, liver, breast Low level of Colon, breast d physical activity (postmenopausal), endometrium FACTORS THAT MAY DECREASE CANCER RISK Fruits and Lung, mouth, pharynx, nonstarchy larynx vegetables CarotenoidLung, mouth, pharynx, containing foods larynx, esophagus Tomato products Prostate Allium vegetables Stomach, colon, rectum (onion, garlic) Vitamin C– Esophagus containing foods Folate-containing Pancreas, colon, rectum foods Fiber-containing Colon, rectum foods Milk products and Colon, rectum calcium supplements High level of Colon, breast physical activityd (postmenopausal), endometrium VIRUSES LINKED TO CANCER EPSTEIN BARR: nasopharyngeal cancer, T- cell lymphoma, Hodgkin's disease, and gastric carcinoma MONONUCLEOSIS (KISSING’S DISEASE) ▶ viral infection caused by Epstein-Barr virus HEPATITIS B: liver cancer LECTURE | 2ND SEMESTER | FINALS | WEEK 11 HUMAN PAPILLOMAVIRUS (HPV): cervical cancer ▶ a common sexually transmitted infection. Almost all sexually active people will be infected at some point in their lives, usually without symptoms. CLASSIFICATIONS OF CANCERS • PREVENT CANCER • • • Cancers are classified by the tissues or cells from which they develop: • • • • • • • CARCINOMAS arise from epithelial tissues; most common; arises from cells that cover external and internal body surfaces; lung, breast, and colon SARCOMAS arise from connective (supporting) tissues, such as muscle or bone, cartilage, fats LYMPHOMAS arise from lymphoid tissue; lymph nodes LEUKEMIAS arise from white blood cell precursors; problem in bone marrow MYELOMAS arise from plasma cells in the bone marrow; leads to overproduction of abnormal antibodies ADENOCARCINOMAS arise from glandular tissues. MELANOMAS arise from pigmented skin cells. • • • • • • Nitrates in cured and smoked foods (sausages, tinapa, hotdog, ham) associated with stomach and esophagus cancer High-fat diets associated with uterine, breast, prostate, and colon cancers Excessive caloric intake associated with gallbladder and endometrial cancer May cause unexplained weight loss, weakness, early satiety, and anorexia May lead to loss of muscle tissue, hypoalbuminemia, and anemia Effect of cancer on the client depends on the location of the tumor TREATMENT OF CANCER • RELATIONSHIP OF FOOD AND CANCER • Increase fiber Vitamin C and A against stomach and esophageal cancer Cruciferous vegetables—such as cauliflower, broccoli, and brussels sprouts—may inhibit several types of cancer, including cancers of the prostate, bladder, and lung. High intake of soy foods THE EFFECTS OF CANCER • Certain substances in foods are thought to be carcinogenic: Alcohol and cigarettes associated with lung, mouth, pharynx, and esophagus cancer Surgical removal, radiation, chemotherapy, or a combination of these methods used to treat cancer Side effects of these treatments can affect nutrition. RADIATION AND CHEMOTHERAPY MAY CAUSE: • • • • • Xerostomia (dry mouth); take frequent sips of water, ice cubes or another sugarless beverage. Dysphagia (difficulty in swallowing); soft diet or give thickened liquid, pureed diet Anorexia; home cooked meals Nausea and vomiting; meds: metoclopramide Diarrhea with possible fluid and electrolyte imbalances; low residue diet, increase fluid, high protein-high calorie diet LECTURE | 2ND SEMESTER | FINALS | WEEK 11 GUIDELINES FOR REDUCING CANCER RISK Achieve and maintain a healthy body weight throughout life: • Be as lean as possible within the normal range of body weight for your height. • Avoid weight gain and increases in waist circumference throughout adulthood. Be physically active as part of everyday life: • For adults: engage in moderate physical activity (equivalent to brisk walking) for at least 30 minutes each day; increase duration or intensity of activity as fitness improves. • For children and adolescents: engage in moderate-to-vigorous activity for at least 60 minutes each day. • Limit sedentary habits such as watching television. Choose a healthy diet that emphasizes plant sources: • Limit consumption of energy-dense foods (.225 kcal per 100 g food) and sugary drinks that contribute to weight gain. • Consume relatively unprocessed grains and/or legumes with every meal. Choose whole-grain products instead of processed (refined) grains. • Consume at least 2½ cups of nonstarchy vegetables and fruit every day. Limit consumption of foods that may increase cancer risk: • Limit consumption of red meat (beef, pork, and lamb) to 18 ounces per week. • Limit consumption of processed meats (those preserved by smoking, curing, or salting). • Avoid salt-preserved, salted, and salty foods. • Avoid moldy grains and legumes. Limit consumption of alcoholic beverages. • For women: consume no more than one drink daily. • For men: consume no more than two drinks daily. Aim to meet nutritional needs through the diet. • Obtain necessary nutrients from the diet. Dietary supplements are not recommended for cancer prevention, and they may have unexpected adverse effects. Avoid using tobacco in any form. CONCLUSIONS • • • • • • Cancer is a disease characterized by abnormal cell growth. Energy needs increase because of the hypermetabolic state and the tumor's need for energy nutrients. Surgery, radiation, and chemotherapy can cause side effects that affect nutrition. Improving the nutritional state is difficult because of the illness and anorexia. Parenteral or enteral nutrition may be necessary. The health care professional can help the client improve nutrition. DIETS AND CLIENTS WITH SPECIAL NEEDS NUTRITIONAL CARE OF SURGERY CLIENTS • • • • If the surgery is elective, nutritional status should be evaluated before surgery. Extra protein, carbohydrates, vitamins C, and minerals may be needed. For overweight clients, improved nutritional status may include weight reduction before surgery whenever possible. NPO to prevent aspiration; provide IV fluids NUTRITIONAL CARE AFTER SURGERY LECTURE | 2ND SEMESTER | FINALS | WEEK 11 • • • When peristalsis returns, ice chips may be given followed by a clear liquid diet. Progress to a regular diet depends on the type of surgery Some clients may need parenteral or enteral feedings. DUMPING SYNDROME (Rapid gastric emptying) • • • • May occur following gastric surgery Characterized by dizziness, weakness, cramps, vomiting, and diarrhea shortly after eating Caused by food moving too quickly from the stomach into the small intestine To prevent, eat small meal, avoid high sugar foods, eat a diet high in protein and fat, and restricted in carbohydrates. METHODS OF NUTRITION SUPPORT • • ORAL: nourishment through the regular Gl route by oral feedings; may include a variety of diet plans, textures, and meal replacement liquid supplements ENTERAL: technically refers to nourishment through the regular GI route either by regular oral feedings or by tube feedings; however, in medical nutrition therapy, enteral feedings imply tube feedings • PARENTERAL: nourishment through the veins (either small peripheral veins or a large central vein) bypassing the Gl Tract Criteria for Selecting a Nutrition Support Method The physician and dietitian will decide the most appropriate method of medical nutrition therapy for the patient with the use of the following criteria. Either the pharmacist or the registered dietitian nutritionist will make the calculations for the enteral formula or parenteral nutrition solution that will be used. ENTERAL NUTRITION SUPPORT Is indicated for patients with the following characteristics: • They have enough functional gastrointestinal tract to allow adequate digestion and absorption. • They cannot eat enough to meet their nutrient needs orally. • They are at risk for malnutrition without nutrition support. PARENTERAL NUTRITION SUPPORT Is indicated for patients with the following characteristics: • They do not have sufficient gastrointestinal tract function and they need long-term nutrition support. • They are unable to meet nutrient needs after 7 to 10 days of enteral nutrition. • There is a need for bowel rest (e.g., enteral fistulas, acute inflammatory bowel disease). • They do not have access for feeding tube placement and need nutrition support. • They repeatedly pull out their feeding tubes. The decision is then made for which form of parenteral nutrition support: ❑ Peripheral Parenteral Nutrition Length of therapy of ≤10 to 14 days LECTURE | 2ND SEMESTER | FINALS | WEEK 11 Not hypermetabolic No fluid restriction ❑ Central Parenteral Nutrition Long-term therapy needed Hypermetabolic Fluid restriction Poor peripheral access or central access already in place • • • • • intractable (not controlled) vomiting or diarrhea high-output fistulas severe malabsorption nutrition support is < 5-7 days in a malnourished patient 7-9 days in an adequately nourished patient ENTERAL NUTRITION TYPES OF ENTERAL FORMULAS CANDIDATES FOR TUBE FEEDINGS STANDARD (POLYMERIC) FORMULAS • • • • • • • • • Severe swallowing disorders Impaired motility in the upper Gl tract Gl obstructions and fistulas that can be bypassed with a feeding tube Certain types of intestinal surgeries Little or no appetite for extended periods, especially if the patient is malnourished Extremely high nutrient requirements Mechanical ventilation Mental incapacitation due to confusion, neurological disorders, or coma • Contain intact macronutrients that the body must break down to be absorbed provided to individuals who can digest and absorb nutrients without difficulty. Pre-Digested: HYDROLYZED • • • • • a.k.a. elemental, chemically defined, monomeric formulas Contain macronutrients that are already broken down to maximize absorption Used for patient with pancreatitis, abdominal pain, diarrhea because pre digested But studies have not consistently been shown to be better tolerated than polymeric formulas. It is best practice to start with a standard formula and investigate all other possible causes of intolerances before switching to predigested. DISEASE-SPECIFIC (SPECIALIZED) FORMULAS • • • Have a nutrient profile that addresses a metabolic condition/organ dysfunction intended to meet the nutrient needs of patients with particular illnesses CONTRAINDICATED FOR TUBE FEEDINGS BLENDERIZED • • Severe GI bleeding Contain a mixture of whole foods that have been pulverized into a liquid LECTURE | 2ND SEMESTER | FINALS | WEEK 11 • • whole foods such as chicken, vegetables, fruit, and oil, along with some added vitamins and mineral. Whether a liquid form of a medication is available and, if so, the appropriate dosage of the liquid form • If only tablets are available, whether the tablets can be crushed and mixed with water. Enteric-coated and sustained-release medications should not be crushed due to the potential for adverse effects. In general, it is best to give medications by mouth instead of by tube whenever possible. In some cases, the injectable form of a medication may be the best option. For medications that must be given by feeding tube: • Do not mix medications with enteral formulas. Do not mix medications together. • Before administering medications, ensure that the feeding tube is placed correctly, that it is not clogged, and that the gastric residual volume is not excessive. • Position the patient in a semi-upright position (30 degrees or higher) to prevent aspiration. • Flush the feeding tube with 15 to 30 milliliters of warm water before and after administering a medication. When more than one medication is administered, flush the feeding tube with water between medications • Use liquid forms of medications whenever possible. Dilute viscous or hypertonic liquid medications with at least 30 milliliters of water before administering them through the feeding tube. • If tablets are used, crush tablets to a fine powder and mix with 30 to 60 milliliters of warm water before administering. MODULAR FORMULAS • for patients who require specific nutrient combinations; customized HOW TO Administer Medications to Patients Receiving Tube Feedings The pharmacist is your best resource for learning how and when medications can be administered via feeding tubes, especially when you are dealing with an unfamiliar drug. Check with the pharmacist to learn the following: • Whether a particular medication is known to be incompatible with formulas. • The proper timing of medication administration to avoid diet-drug interactions. • Whether a medication can be absorbed without exposure to stomach acid in patients using intestinal feedings. METHODS OF ADMINISTRATION • • • CONTINUOUS: ongoing over 16- to 24-hour period INTERMITTENT: at night, with food eaten during the day BOLUS: given over a 15-minute period LECTURE | 2ND SEMESTER | FINALS | WEEK 11 LECTURE | 2ND SEMESTER | FINALS | WEEK 11 PARENTERAL NUTRITION (HYPERALIMENTATION) Accessing Central Veins for Total Parenteral Nutrition • • • • • • • Gallbladder disease Hyperglycemia, hypoglycemia Hypertriglyceridemia Liver disease Metabolic bone disease Nutrient deficiencies Refeeding syndrome: occurs due to rapid shifts in electrolytes (such as potassium, magnesium, and phosphorus) and fluid balance when someone starts eating after a period of starvation or malnutrition. CLIENT WITH BURNS NUTRITION THERAPY FOR CLIENTS WITH BURNS Potential Complications of Parenteral Nutrition • CATHETER-RELATED • • • • • • • • Air embolism Blood clotting at catheter tip Clogging of catheter Dislodgment of catheter Improper placement Infection, sepsi Phlebitis Tissue injury METABOLIC • Electrolyte imbalances • • Increased need for vitamin C and zinc for healing Vitamin B is needed for the metabolism of the extra nutrients. Sufficient fluids are needed to maintain kidney function. High carbs, high protein diet THE CLIENT WITH INFECTIONS • • Fever is a hypermetabolic state in which each degree of fever on the Fahrenheit scale raises the basal metabolic rate (BMR) 7%. If extra calories are not provided, the body uses its sources of stored energy. LECTURE | 2ND SEMESTER | FINALS | WEEK 11 • • • • Protein intake should be increased. Minerals are needed to help build and repair body tissue and to maintain acid-base, electrolyte, and fluid balance. Extra vitamins are also necessary for the increased metabolic rate and to help fight the infection causing the fever. Extra liquid is needed to replace losses. THE CLIENT WITH AIDS • • • • • • • • Human immunodeficiency virus (HIV) invades the T cells, which are white blood cells that protect the body from infections. When T cells cannot function normally, body has no resistance to opportunistic infections. Persons diagnosed as being HIV positive should have a baseline nutrition and diet assessment. A healthful diet may delay the onset of AIDS. Unhealthful eating habits can be corrected at an early stage of the disease, and future nutritional needs explained. Clients with AIDS experience serious proteinenergy malnutrition (PEM) and thus, body wasting known as "wasting syndrome." This results in hypoalbuminemia and weight loss. Opportunistic infections (OIs): infections that occur more often in people with weakened immune systems than with healthy immune systems CONCLUSIONS • • • • • Surgery, burns, fevers, and infections are traumas that cause the body to respond in a hypermetabolic manner. This response creates the need for additional nutrients at the same time that the injury causes a loss of nutrients. Care must be taken to provide extra fluids, proteins, calories, vitamins, minerals, and carbohydrates as needed in these situations. When surgery is elective, nutritional status should be improved before surgery. When food cannot be taken orally, enteral or parenteral nutrition should be used. NUTRITIONAL CARE OF ELDERLY CLIENTS PROTEIN ENERGY MALNUTRITION • • • • • When food intake does not meet body needs, the body uses its own stores of energy. When glycogen and fat stores are exhausted, the body must break down its own tissues to provide protein for energy = severe muscle wasting Protein-energy malnutrition (PEM) can be a problem among hospitalized clients. PEM can delay wound healing, contribute to anemia, depress the immune system, and increase susceptibility to infections. Iatrogenic malnutrition: caused by medications, complications, and negligence; hospital acquired IMPROVING CLIENT'S NUTRITION • • Formal nutritional assessments should be made on a regular basis. All members of the health care team should be alert to signs of malnutrition every day. LECTURE | 2ND SEMESTER | FINALS | WEEK 11 • • • • • Listen to client's concerns and watch the reaction to food served. Include the dietitian in the plan of care. In the home, the family menu should serve as the basis for the client's meal whenever possible. Omit or add certain foods as necessary. Vary the method of preparation if needed. SERVING THE MEAL • • • • • • • • • • Make tray and food arrangement as attractive as possible. Serve water, as well as another beverage. Serve food at proper temperature. Client should be in a comfortable position with tray and utensils placed conveniently. Offer bedpan and hygiene care before and after the meal Any unpleasant sights should be removed. Open containers and try to anticipate the client's needs Give sufficient time to eat and reheat food as needed. Document intake per facility policy. Heracline: drug that increase appetite PHYSICAL PROBLEMS OF THE INSTITUTIONALIZED ELDERLY • • PEM is a major problem for this population. Anemia can develop and contribute to fatigue, confusion, and depression. • Sufficient animal protein and vitamin C should be provided in the diet. • Pressure ulcers (bedsores) can develop in bedridden clients and must be prevented. • Healing of pressure ulcers requires treatment of the ulcer, relief of the pressure, a highcalorie diet with sufficient protein, vitamin C, and zinc supplements. • Constipation – give adequate fluid, fiber, and exercise, stool softener, walking • Diarrhea • The sense of smell declines with age and the appetite diminishes. • Xerostomia (dry mouth) • Dysphagia (difficulty swallowing) – give thickened liquids, upright position CONCLUSIONS • • • FEEDING A CLIENT WHO REQUIRES ASSISTANCE • • • • • • Sit near the side of the bed. Small amounts of food should be placed toward the back of the mouth with a slight pressure on the tongue with the spoon or fork. Do not feed a client with a syringe. If paralyzed, food and straw should be placed on nonparalyzed side of the mouth. If client begins to choke, help her or him sit up straight. A client diagnosed with dysphagia will require a specialized diet. A client with dysphagia should not use a straw. • • • • • • Illness and surgery can have devastating effects on a client's nutritional status. PEM can be a significant problem in hospitals. Bed-bound clients should be offered the bedpan and assistance with hygiene care before meals. Clients should be encouraged to feed themselves. However, help should be offered and needs anticipated. The client who is blind can eat more easily if food is arranged in a set pattern on the plate. Provide pleasant conversation and atmosphere. Record the type of diet, time of meal, client's appetite, and type and amount of food eaten. Nutrition-related health problems in the elderly can sometimes be relieved with proper treatment.