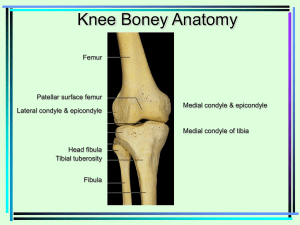
ANATOMY AND BIOMECHANICS OF THE MENISCUS ANSWORTH A. ALLEN, MD, GEORGE L. CALDWELL, JR, MD, and FREDDIE H. FU, MD The menisci appear at approximately the 8th to 10th week of fetal development. They are discernible in the adult knee joint as crescent-shaped fibrocartilagenous wedges between the femoral and tibial condyles. Their unique design, structure, composition, and anatomic attachments allow the menisci to play an integral role in normal knee joint function. The primary biomechanical function of the meniscus is load transmission. Other functions include shock absorption, joint stability and congruity, and joint lubrication and nutrition. KEY WORDS: menisci, fibrocartilagenous structure, composition, anatomic, biomechanical, load transmission Our understanding of the meniscus has evolved significantly during this century Initially regarded as functionless remains of leg muscle, 1 the meniscus is now recognized as an important component of the functional anatomy and biomechanics of the knee joint. Meniscal injury is one of the more common injuries sustained by athletes. 2 Although Fairbanks 3 noted changes in the joints consistent with degenerative arthritis after total meniscectomy, this relationship was not clearly appreciated, and it was not until the mid-1960s that the wisdom of total meniscectomy was questioned. 4 As recently as 1971, Smillie s advocated total meniscectomy during anterior arthrotomy if damage to the posterior horn of the meniscus was even suspected. Over the past two decades, tremendous strides have been made in our understanding of the basic anatomy and biomechanics of the meniscus. It is now recognized that total meniscectomy is not a benign procedure. The surgical philosophy today is to preserve as much of the healthy meniscus as possible and to repair the meniscus w h e n feasible. Meniscal replacement with allograft tissue is also possible. 6-s This article reviews the anatomy and biomechanics of the meniscus. ANATOMY Embryology The menisci are discernible as distinct structures between the 8th and 10th week of fetal development. 9 They arise from a condensation of the intermediate layer of mesenFrom the Hospital for Special Surgery, New York; the Department of Orthopaedics, Cornell Medical College, New York, NY; the Cleveland Clinic, Fort Lauderdale, FL; Department of Orthopaedic Surgery, Blue Cross of Western Pennsylvania, Pittsburgh; and the Department of Orthopaedic Surgery, University of Pittsburgh, Pittsburgh, PA. Address reprint requests to Freddie H. Fu, MD, Blue Cross of Western Pennsylvania, Universityof Pittsburgh, Craig Ave and Baum Blvd, Pittsburgh, PA 15213. Copyright © 1995 by W. B. Saunders Company 1048-6666/95/0501-0002505.00/0 2 chymal tissue and form attachments to the surrounding joint capsule and the cruciate ligaments. 10 The developing menisci are highly cellular and vascular. There is a gradual decrease in the cellularity of the meniscus with a concomitant increase in the collagen content, and the blood vessels retract to the outer region of the meniscus. 11 This transition occurs from the prenatal to the postnatal stages of development. These histological changes seem to be a reflection of the meniscal response to joint motion and the stress of weight bearing. These changes are most significant between 1 to 3 years of age, when a child becomes ambulatory. 11 FUNCTIONAL ANATOMY Although the menisci are distinct structures, they act as a functional extension of the tibial plateau to increase the relative depth of the tibial articular surface.12-15 The menisci are located on the peripheral rim of the tibial condyles, from which they extend into the middle of the joint. They are triangular in cross-section, with a thicker, more convex region peripherally that tapers into a thin, free edge centrally (Figs 1 and 2). 16 The proximal meniscal surfaces articulate with the femoral condyles. They are concave to accommodate the convexity of the femoral condyles. The inferior or distal surface is flat and articulates with the convex tibial condyle laterally and the concave tibial condyle medially to form the meniscotibial socket. This socket may contribute to the stability of the knee joint, Although the medial and lateral menisci are histologically similar, they are unique structures with different shapes, sizes, and attachments. Medial Meniscus The medial meniscus is more frequently injured than the lateral meniscus. This is a reflection of its functional anatomy and its relationship to the surrounding structures in the joint. It is semilunar in shape and is approx- Operative Techniques in Orthopaedics, Vol 5, No 1 (January), 1995: pp 2-9 gament .~ral 3iscus Posterior cruciate ligament Fig 1. Drawing of the tibial plateau showing the shape and attachments of the medial and lateral menisci. The transverse ligament and the cruciate ligaments are also shown. (Reprinted with permission, is) Fig 2. Photograph of a frontal section through the medial compartment of a human knee. The meniscal articulation with the femoral and tibial condyles is shown. The triangular cross-section of the meniscus is also shown (arrow). (Reprinted with permission, is) imately 3.5-cm long w h e n measured in the anteriorposterior direction. It is significantly broader posteriorly and becomes progressively more narrow as the anterior horn is approached. Ferrer-Roca and Vilalta 17 measured the width of the meniscus along the radius of the tibial plateau and showed that the width of the posterior horn averaged 10.6 mm at its widest point. The midpoint averaged 9.6 mm, and the anterior horn averaged 7.7 m m . The anterior horn attachment of the medial meniscus is in the front of the anterior cruciate ligament in the region of the anterior intercondylar fossa, whereas the posterior horn attaches to the posterior intercondylar fossa anteromedial to the posterior cruciate ligament. Johnson et al is recently re-examined the tibial insertion sites of the menisci a n d their topographical relationships to surrounding anatomical landmarks in the knee. They found that the anterior- and posterior-horn insertion sites of the medial meniscus were larger than those of the lateral meniscus. The area of the anterior-horn insertion site of the medial meniscus was the largest overall and ANATOMY AND BIOMECHANICS OF THE MENISCUS measured 1.12 cm 2, whereas that of the posterior horn was 0.68 cm 2. It was also apparent that the medial meniscai horns were not as close to the anterior cruciate ligaments as previously thought (Fig 3). The transverse ligament is a fibrous band of tissue that connects the anterior horn of the medial meniscus to the anterior horn of the lateral meniscus (Fig 1). The medial meniscus is attached through its periphery to the joint capsule. The deep medial collateral ligament represents a distinct thickening of the joint capsule. It is attached to the midportion of the meniscus. The coronary ligament is the inferior portion of the capsule that attaches the meniscus to the tibial plateau. There is decreased mobility of the medial meniscus secondary to its capsular and bony attachments. 19 Lateral Meniscus The lateral meniscus is almost circular, with the anterior and posterior horns in relatively close proximity. It has a more uniform width than the medial meniscus and occupies a larger portion of the tibial articular surface. 12 Ferrer-Roca and Vilalta 17 also showed that the lateral meniscus is 10.6-mm wide at the posterior horn, 11.6 m m at its midpoint, and 10.2 at the anterior horn. The area of the anterior horn is 0.76 cm 2, whereas that of the posterior horn is 0.94 cm2.18 The meniscal horns are in close proximity to the anterior cruciate ligament. The anterior horn of the lateral meniscus is adjacent and parallel to the anterior half of the anterior cruciate ligament tibial insertion site. The posterior horn of the lateral meniscus inserts slightly more medially at the posterior border of the anterior cruciate ligament tibial insertion site. 18 The lateral meniscus is loosely attached to the joint capsule throughout its periphery, except at the popliteal hiatus. 2° The posterior convexity of the lateral meniscus Fig 3. Schematic drawing of an axial view of a right tibial plateau showing sections of the meniscus and their relationship to the cruciate ligaments. AL, anterior insertion of the lateral meniscus; PL, posterior insertion of lateral meniscus; AM, anterior insertion of the medial meniscus; PM, posterior of medial meniscus. 3 receives an aponeurotic extension from the popliteus muscle, 21"22 as the popliteus tendon grooves the meniscus. A portion of the arcuate ligament is also attached to the upper portion of the posterior convexity of the meniscus. The posterior meniscofemoral ligament (ligament of Wrisberg) extends from the posterior horn of the lateral meniscus to the medial femoral condyle. There is increased excursion of the lateral meniscus 19'22 during knee motion compared with the medial meniscus. This occurs because of the lack of a rigid circumferential attachment and the dynamic contributions from the meniscofemoral ligaments and the popliteus muscle. Meniscofemoral Ligaments The meniscofemoral ligaments consist of the anterior ligament, Humphrey's ligament, and the posterior ligament of Wrisberg (Fig 4). They are accessory knee ligaments that attach to the medial femoral condyle in the region of the posterior cruciate ligament. The presence and size of the meniscofemoral ligaments are variable. Heller and Langman 23 reported meniscofemoral ligaments in 71% of the knees they dissected; however, their reported presence has varied, ranging up to 100%. The posterior meniscofemoral ligament (ligament of Wrisberg) arises from the posterior horn of the lateral meniscus, posterior tibia, or posterior capsule and crosses obliquely, posterior to the posterior cruciate ligament to a distinct insertion site on the medial femoral condyle. It may be as large as one half the diameter of the posterior cruciate ligament. A dominant posterior meniscofemoral ligament was found in 36% of the specimens dissected by Heller and Langman. 23 The anterior meniscofemoral ligament (Humphrey's ligament) arises from the posterior horn of the lateral meniscus and passes along the anterior aspect of the posterior cruciate ligament to insert on the medial femoral condyle. Although the meniscofemoral ligament may serve as a minor restraint to posterior translation of the tibia after the posterior cruciate ligament is cut, the ligaments are believed to play an important role in the normal meniscal kinematics. They increase the congruity between the lateral meniscus and the lateral femoral condyle during flexion, extension, and rotation of the knee. In our studies of the cross-sectional areas of the ligaments, the meniscofemoral ligament averaged 20% (range, 7% to 35%) of the size of the posterior cruciate ligament. 24,25 VASCULAR ANATOMY The menisci have a very limited blood supply and are essentially avascular structures. Their limited vascularity is confined to the peripheral region. The blood supply to the menisci comes from the superior and inferior branches of the medial and lateral geniculate arteries. 12"26-3° Branches from these vessels form a perimeniscal capillary plexus in the synovium and capsular tissues of the knee joint. 26 This network of vessels supplies the peripheral portions of the menisci throughout their attachment to the joint capsule and the synovium. These vessels are arranged predominantly in a circumferential pattern, with radial branches directed toward the central portion of the menisci. 26 Arnoczky and Warren have shown that only the pe- Fig 4. Photograph of a sagittal section of a cadaveric knee-joint specimen showing the anterior meniscofemoral ligament (Humphrey's ligament) (arrow) and its relationship to the posterior cruciate ligament (A) and the posterior meniscofemoral ligament (ligament of Wrisberg) (arrow) and its relationship to the posterior cruciate ligament (B), (Reprinted with permission, s) 4 ALLEN, CALDWELL JR, AND FU ripheral 10% to 30% of the width of the medial meniscus and 10% to 25% of the width of the lateral meniscus are penetrated by these vessels (Fig 5). 26 They also described branches [hat arise from the middle geniculate artery and the terminal branches of the medial and lateral geniculate arteries that supply the anterior and posterior horn attachments of the menisci. This occurs through endoligamentous vessels in the vascular synovium that covers the meniscal horns. The inner 65% to 75% of the menisci is avascular and probably receives most of its nutrition from the synovial fluid by diffusion or mechanical pumping. 3~'32 A system of microcanals in the menisci, which may also play a role in the transport of nutrients, has been described by Bird and Sweet. 33"34 NEUROANATOMY Several different types of neurological receptors have been identified within meniscal tissue. 29'35"36 According to Hilton's law, any nerve that crosses a given joint will send branches to that joint. Nerve supplies to the knee joint come from the posterior articular branch of the posterior tibial nerve, the terminal portion of the obturator nerve, and the terminal branches of the femoral nerve to the quadriceps muscles. Nerve supplies to the lateral portion of the capsule arises from the recurrent peroneal branch of the common peroneal nerve. These nerve fibers penetrate the capsule and follow the vascular supply to the peripheral portion of the menisci and the anterior and posterior horns, where most of the nerve fibers are concentrated. 3s'37 This concentration of sensory receptors in the meniscal horns may implicate the meniscus in some kind of a proprioceptive function in the knee joint. According to Wilson et a136 there are also free-standing nerve fibers in the menisci that are not surrounded by vessels. These fibers are present predominantly in the middle third of the menisci, an area that is devoid of Fig 5. Frontal section 5-mm thick of the medial compartment of the knee (Spalteholz preparation, original magnification x65, x 1.65). Branchiing radial vessels from the perimeniscal capillary plexus (PCP) penetrate the peripheral border of the medial meniscus. F, femur; T, tibia. (Reprinted with permission. 26) ANATOMY AND BIOMECHANICS OF THE MENISCUS penetrating vessels. pain conduction. 36 They have been implicated in slow MICROANATOMY Composition and Structure The meniscus is fibrocartilagenous tissue composed of collagen, with interposed cells. These cells are either fibrochondrocytes or a mixture of fibroblasts and chondrocytes. There are two types of cells: the more superficial fusiform cells and the deeper ovoid cells. These cells synthesize and maintain the extra cellular matrix, which is primarily collagen. 12 Approximately 74% of the normal meniscus is water. The dry organic matrix is composed of 75% collagen, with 8% to 13% n o n c o l l a g e n o u s p r o t e i n s a n d 1% hexosamines. Type I collagen predominates and is approximately 90% of the total collagen. Smaller amounts of types II, III, V, and VI collagens are also present. 3s The predominance of type I collagen distinguishes the fibrocartilage of the menisci from the hyaline cartilage of the joint surface, where type II cartilage predominates. The type V collagen seems to be concentrated on the articular surfaces of the menisci. 12 As previously stated, the collagen content of the menisci increases from the prenatal to the postnatal stages in response to the stress of weight bearing and joint motion} 1 According to Ghosh et a139 the collagen content increases until approximately age 30 and remains fairly constant until it begins to decrease at around age 80. The crimping pattern of collagen fibers observed in tendons is also present in the menisci. This pattern disappears when stress is applied to the tissue. 39 The collagen fiber arrangement is ideal for transferring a vertical compressive load into circumferential stresses. 39 Type I collagen fibers are oriented circumferentially in the deeper layers of the meniscus, parallel to the peripheral border. These fibers blend into the ligamentous connections of the meniscal horns to the tibial articular surface. 12"4°-42 In the most superficial region of the menisci, the type I fibers are oriented in a more radial direction. Some radially oriented fibers are also present in the deeper layers. The radial fibers come in from the periphery and are interspersed or woven between the circumferential fibers to provide structural rigidity. 4°-43 This arrangement of the fibers is important in resisting large hoop or circumferential stresses that are produced at the periphery of the menisci during weight bearing (Fig 6).12,40-42 Proteoglycans are located between the collagen fibers. The amount of proteoglycans in the meniscus is significantly less than that of hyaline articular cartilage, 12 and there may be considerable variation, depending on the site from which the sample was taken and the age of the specimenY This may contribute to the regional variation of the stiffness and strength of the normal meniscus. 44 Proteoglycans provide a function in the menisci similar to the function they provide in articular cartilage: they give the menisci the ability to resist large compressive loads} 2 5 Fig 6. Schematic drawing of the meniscus showing the collagen fiber orientation (Modified and reprinted with permission. 4°) Meniscal Motion Normal knee kinematics is an intricate combination of flexion, extension, rolling, and gliding motion within 6° of freedom. Meniscal motion was recently demonstrated in a study by Thompson et a1.19 They used human cadaveric knees and a 3-dimensional magnetic resonance imaging reconstruction technique to demonstrate motion of the menisci as the knee was moved through 0° to 120° of flexion. The images were shown in a cinematic format to demonstrate meniscal deformation (Figs 7 and 8). The quantitative excursion of the menisci was also assessed. Excursion of the medial meniscus averaged 5.1 + 0.96 m m as compared with 11.2 --- 3.27 mm mean lateral meniscal excursion. On both sides, the mean excursion of the posterior horn was less than that of the anterior horn. The ratio of mean posterior- to anterior-horn excursion was 1:2.4 --- 0.8 medially and 1:1.13 --- 0.23 laterally (Fig 9). 19 Thompson et al demonstrated the limitation of medial meniscal excursion in the posteromedial corner caused by the meniscocapsular attachments and the articular geometry in this region. The increased excursion of the lateral meniscus was attributed t o its unconstrained popliteal margin and close central tibial attachments. They also pointed out that the menisci deform and change their radii to remain congruent to the tibiofemoral articular surface throughout range of knee motion. The increased excursion of the lateral meniscus relative to the medial meniscus was confirmed. This presumably is because of the greater soft tissue and bony constraints of the medial meniscus. 19 BIOMECHANICS The biomechanical function of the meniscus is a reflection of its gross and ultra structural anatomy and of its relationship to the surrounding intra-articular and extraarticular structures. Biomechanical functions performed by the menisci include load transmission, 12"45-48shock ab6 Fig 7. (A-C) Superior 3-dimensional meniscal images in 60 ° increments from 0 ° to 120 ° of flexion (A, anterior; P, posterior; M, medial; L, lateral). (Reprinted with permission. 19) sorption, 12'41"49 joint stability, 5°'52 joint lubrication, 53"55 and joint nutrition. 33'56'57 Load Transmission Although Kings8 was the first to imply that the meniscus may have a role in load transmission across the knee joint, it was Fairbanks 3 who first hypothesized that the meniscus may have some load-bearing function. His hypothesis was based on the changes he observed in postmeniscectomy knees. A number of clinical and biomechanical studies have supported Fairbanks hypothesis. 34,45-48,51,59-68 One of the more attractive models of load transmission was put forth by Shrive et al. 62"67 They proposed that because of the wedge shape of the meniscus, a net resultant force is generated in response to an applied load, which tends to extrude the menisci from the joint. This ALLEN, CALDWELL JR, AND FU P/A 1:1.3"x" P/A 1:2.4 "X" 7.0 ~m ANT ,,ss,.-" 1' " ' ~ . . I 12.8 % .....,~,~%~:~ t 5.1 mme 11.2 rome "~:.~ %% POST LATERAL MEDIAL I I 1:2.3" Fig 9. Diagram of mean meniscal along t h e tibial plateau (ANT, anterior; POST, posterior; MME, mean meniscal excursion; P/A, ratio of posterior to anterior meniscal translation during flexion; *, P < 0.05 by Student's t-test analysis). (Reprinted with permission. TM) knee ranges of motion from 0° to 90 °, with more load transmission at full extension. Load transmission may be one of the more important meniscal functions. The menisci protect the articular cartilage from excessive stresses and prevent early degenerative changes in the joint. Joint Stability and Congruity Fig 8. (A-C) Lateral 3-dimensional meniscal images in 60 ° increments from 0 ° to 120 ° of flexion (A, anterior; P, posterior; M, medial; L, lateral). (Reprinted with permission. 19) is resisted by the circumferentially oriented collagen fibers and their a t t a c h m e n t s to the meniscal horns. Therefore, large circumferential hoop stresses are generated to balance this net resultant force. They estimated that approximately 45% of the knee-joint load is carried by the meniscus. Baratz et al 6° have shown that total meniscectomy decreased the tibia-femoral contact area up to 75%, with increased peak load of up to 235%. Partial meniscectomy decreased the contact area by only 10% and increased the peak load by 65%. Malalignment of the joint in postmeniscectomy knees can decrease the contact areas and increase the peak stresses in the knee joint. 69 The posterior horns of the menisci carry more load than the anterior horns, and the load distribution is a function of the knee flexion angle. Ahmed and Burke 59 used pressure gradient transducers to show that the menisci transmit at least 50% of the compression load in the knee joint in ANATOMY AND BIOMECHANICS OF THE MENISCUS The role of the menisci in increasing joint congruity and enhancing stability is conceptually apparent w h e n the articular surfaces of the tibiofemoral joint are examined. However, a consensus of opinion regarding the stabilizing role of the meniscus in the intact knee has not been reached. 12 The joint surfaces are noncongruous, and the proximal surface of the meniscus provides a concave surface that accommodates the convexity of the femoral condyles. In doing so, the meniscus not only obliterates the dead space between the femur and the tibia, but also increases the congruity of the tibiofemoral joint. 12"15 In essence, the menisci act like wedges to perform the so-called "socket-forming function" of the meniscus described by Virchow. 7° Joint stability may also be facilitated through the meniscoligamentous and meniscocapsular connections. The medial meniscus is a secondary stabilizer of the knee, decreasing anterior knee translation in anterior cruciate-ligament-deficient knees. 71 There is little effect on anterior-posterior knee translation after medial meniscectomy in anterior cruciate-ligament-intact knees. 69 The medial meniscus is prone to injury in patients with chronic anterior cruciate-ligament-deficient knees. 71 As the meniscus attempts to prevent anterior translation of the anterior cruciate-ligament-deficient knee, it is exposed to increased shear stresses, and meniscal damage can occur. Joint Lubrication and Nutrition The role of the meniscus in joint lubrication has been extrapolated from the studies that have shown that the coefficient friction of the joint is increased by 20% after 7 meniscectomy. 53-55 Although fluid is extruded from the hyaline cartilage of the articular surface during weight bearing, it is not clear whether this is true of the meniscus. 12 Bird and S w e e t 33'56 have found a system of microcanals within the meniscus that not only communicates with the synovial cavity but is also located close to the blood vessels. These canals have been implicated in fluid transport for nutritional purposes and joint lubrication. It would seem likely that the peripheral portion of the menisci receives its nutrition from the vasculature at the periphery of the meniscus. The inner portion of the meniscus, ie, the remaining 65% to 75%, most likely receives its nutrition from diffusion, the synovial cavity, or m e c h a n i c a l p u m p i n g s e c o n d a r y to joint motion.12 Microcanals may also serve as a conduit for nutrients. 33,56 CONCLUSION The menisci are integral to normal knee function. A fundamental knowledge of meniscal anatomy and biomechanics is necessary to predict the meniscal response to injury and repair. Although we have made significant strides in our understanding of the basic science of the menisci, there are still questions that need to be resolved. Future studies will focus on the biochemistry, microanatomy, and biomechanics of the menisci. REFERENCES 1. Sutton JB: Ligaments: Their nature and morphology. London, England, M. K. Lewis, 1897 2. Sonne-Holm S, Fledelius I, Ahn N: Results after meniscectomy in 147 athletes. Acta Orthop Scand 51:303-309, 1980 3. Fairbanks TJ: Knee joint changes after meniscectomy. J Bone Joint Surg [Br] 30:664-670, 1948 4 Huckell J: Is meniscectomy a benign procedure? Can J Surg 8:254260, 1965 5. Smillie JS: Injuries of the Knee Joint (ed 4). London, Churchill Livingstone, 1970, p 31 6. Arnoczky SP, Warren RF: Anatomy of the cruciate ligaments, in Feagin JA (ed): The Cruciate Ligaments (ed 2). New York, NY, Churchill Livingstone, 1994, pp 269-287 7. Garrett JC: Meniscal transplantation in the human knee: A preliminary report. Arthroscopy 7:57-62, 1991 8. Milachowski KA, Weismeier K, Wirth CJ: Homologous meniscus transplantation. Experimental and clinical results. Int Orthop 13:111, i989 9. Gray DJ, Gardner E: Pre-natal development of the human knee and superior tibial fibula joints. Am J Anat 86:235-288, 1950 10. McDermott LJ: Development of the human knee joint. Arch Surg 46:705-719, 1943 11. Clark CR, Ogden JA: Development of the menisci of the human knee joint. J Bone Joint Surg [Am] 65:530, 1983 12. Arnoczky S, Adams M, DeHaven K, et al: Meniscus, in Woo SY, Buckwalter JA (eds): Injury and Repair of the Musculoskeletal Soft Tissues. American Academy of Orthopaedic Surgeons, Chicago, IL, 1987, p 487 13. Bullough PG, Vosburgh F, Arnoczky SP, et ah The menisci of the knee, in Insall JN (ed): Surgery of the Knee. New York, NY, Churchill Livingstone, 1984, pp 135-146 14. Insall JN: Anatomy of the knee, in Insall JN (ed): Surgery of the Knee. New York, NY, Churchill Livingstone, 1984, pp 1-20 15. Warren R, Arnoczky SP, Wickiewicz TL: Anatomy of the knee, in 8 Nicholas JA, Hershman EB (eds): The Lower Extremity and Spine in Sports Medicine. St. Louis, MO, Mosby, 1986, pp 657-694 16. Arnoczky SP: Gross and vascular anatomy of the meniscus and its role in meniscal healing, regeneration and remodeling, in Mow VC, Arnoczky SP, Jackson DW (eds): Knee Meniscus: Basic and Chemical Foundations. New York, NY, Raven, 1992, pp 1-4 17. Ferrer-Roca O, Vilalta C: Lesions of the meniscus, part 1: Macroscopic and histologic findings. Clin Orthop 146:289-300, 1980 18. Johnson DL, Swenson TD, Harner CD: Arthroscopic meniscal transplantation: Anatomic and technical considerations. Presented at the Nineteenth Annual Meeting of the American Orthopaedic Society for Sports Medicine, Sun Valley, ID, July 12-14, 1993 19. Thompson WO, Thaete FL, Fu FH, et al: Tibial meniscal dynamics using three dimensional reconstruction of magnetic resonance images. Am J Sports Med 19:210-216, 1991 20. Seebacher JR, Inglis AE, Marshall JL: The structure of the posterolateral aspect of the knee. J Bone Joint Surg [Am] 64:536-541, 1982 21. Last RJ: Some anatomical details of knee joint. J Bone Joint Surg [Br] 30:683, 1948 22. Last RJ: The popliteus muscle and the lateral meniscus. J Bone Joint Surg [Br] 32:93-99, 1950 23. Heller L, Langman J: The meniscofemerol ligaments of the human knee. J Bone Joint Surg [Br] 46:307-313, 1964 24. Harner CD, Kusayama T, Carlin G, et al: Structural and mechanical properties of the human posterior cruciate and meniscofemoral ligaments. Transaction of the 40th Annual Meeting, Orthopaedic Research Society, 19:629, 1992 25. Harner CD, Livesgay GA, Choi NY, et al: Evaluation of the sizes and shapes of the human anterior and posterior cruciate ligaments: A comparative study. Trans Orthop Res Soc 17:123, 1992 26. Arnoczky SP, Warren RF: Microvasculature of the human meniscus. Am J Sports Med 10:90-95, 1982 27. Danzig L, Resnick D, Gonsalves M, et al: Blood supply to the normal and abnormal menisci of the human knee. Clin Orthop 172:271, 1983 28. Davies DU, Edwards DAW: Blood supply of the synovial membrane and intra-articular structures. Ann R Coll Surg Engl 2:142-156, 1948 29. Day B, Mackenzie WG, Shimm SS, et al: The vascular and nerve supply of the human meniscus. Arthroscopy 1:58, 1985 30. Scapinelli R: Studies of the vasculature of the human knee joint. Acta Anat 70:305-331, 1968 31. Mow VC, Fithian DC, Kelly MA: Fundamentals of articular cartilage and meniscus biomechanics, in Ewing JW (ed): Articular Cartilage and Knee Joint Function. New York, NY, Raven, 1989, pp 1-18 32. Myers ER, Zhu W, Mow VC: Viscoelastic properties of articular cartilage and meniscus, in Nimni ME (ed): Collagen: Chemistry, Biology and Biotechnology. Boca Raton, FL, CRC, 1988, pp 268-288 33. Bird MDT, Sweet MBE: Canals in the semilunar meniscus: Brief report. J Bone Joint Surg [Br] 70:839, 1988 34. Bourne RB, Finlay JB, Papadopoulos P, et al: The effect of medial meniscectomy on strain distribution in the proximal part of the tibia. J Bone Joint Surg [Am] 66:1431-1437, 1984 35. Kennedy JC, Alexander IJ, Hayes KL: Nerve supply of the human knee and its functional importance. Am J Sports Med 10:329-335, 1982 36. Wilson AS, Legg PG, McNeur JC: Studies of the innervation of the medial meniscus in the human knee joint. Anat Rec 165:485-492, 1969 37. Gardner E: The innervation of the knee joint. Anat Rec 101:109-130, 1948 38. Ingman AM, Ghosh P, Taylor TKF: Variation of collagenous and non-collagenousproteins of human knee joint menisci with age and degeneration. Gerontologia 20:212-233, 1974 39. Ghosh P, Ingman AM, Taylor TKF: Variations in collagen, noncollagenous proteins, and hexosamine in menisci derived from osteoarthritic and rheumatoid arthritic knee joints. J Rheumatol 2:100, 1975 40. Bullough PG, Munuera L, Murphy J, et al: The strength of the menisci of the knee as it relates to their fine structure. J Bone Joint Surg [Am] 52:564, 1970 41. Fithian DC, Kelly MA, Mow VC: Material properties and structurefunction relationships in the meniscus. Clin Orthop 252:19-31, 1990 42. Skaags DL, Mow VC: Function of the radial tie fibers in the meniscus. Trans Orthop Res Soc 15:248, 1990 ALLEN, CALDWELL JR, AND FU 43. Aspden RM, Yarker YE, Hukins DWL: Collagen orientations in the meniscus of the knee joint. J Anat 140:371, 1985 44. Procter CS, Schmidt M, Whipple RR, et al: Material properties of normal medial bovine meniscus. J Orthop Res 7:771-782, 1989 45. Fukubayashi T, Kurosawa H: The contact area and pressure distribution pattern of the knee. Acta Orthop Scand 51:871-879, 1980 46. Seedholm BB: Transmission on the load in the knee joint with special reference to the role of the menisci: I. Anatomy, analysis and apparatus. New Engl J Med 8:207-219, 1979 47. Seedholm BB, Hargreaves DJ: Transmission of the load in the knee joint with special reference to the role of the menisci: II. Experimental results, discussion and conclusions. New Engl J Med 8:220, 1979 48. Walker PS, Erkman MJ: The role of the menisci in force transmission across the knee. Clin Orthop 109:184, 1975 49. Voloshin AS, Wosk J: Shock absorption of meniscectomized and painful knees: A comparative in-vivo study. J Biomed Eng 5:157, 1983 50. Fukubayashi T, Torzilli PA, Sherman MF, et al: An in vitro biomechanical analysis of anterior-posterior motion of the knee, tibial displacement, rotation, and torque. J Bone Joint Surg [Am] 64:258-264, 1982 51. Krause WE, Pope MD, Johnson RJ, et al: Mechanical changes in the knee after meniscectomy. J Bone Joint Surg [Am] 58:599, 1976 52. Shoemaker SC, Markolf KL: The role of the meniscus in the anterior-posterior stability of the loaded anterior cruciate deficient knee. J Bone Joint Surg [Am] 68:71-79, 1986 53. MacConaill MA: The function of intra-articular fibrocartilages with special reference to the knee and inferior radio-ulnar joints. J Anat 66:210-227, 1932 54. MacConaill MA: Studies in the mechanics of synovial joints II. Displacements on articular surfaces and the significance of saddle joints. Ir J Med Sci 6:223-235, 1946 55. MacConaill MA: The movements of bones and joints. III: The synovial fluid and its assistants. J Bone Joint Surg [Br] 32:244, 1950 56. Bird MDT, Sweet MBE: A system of canals in semilunar menisci. Ann Rheum Dis 46:670-673, 1987 ANATOMY AND BIOMECHANICS OF THE MENISCUS 57. Johnson RJ, Pope MH: Functional anatomy of the meniscus. Symposium on Reconstruction of the Knee. American Academy of Orthopaedic Surgeons. St. Louis, MO, Mosby, 1978, p 3 58. King D: The function of semilunar cartilages. J Bone Joint Surg [Am] 18:1068, 1936 59. Ahmed AM, Burke DL: In vitro measurement of static pressure distribution in synovial joint: I. Tibial surface of the knee. J Biomech Eng 105:216-225, 1983 60. Baratz ME, Fu FH, Mengato R: Meniscal tears: The effect of meniscectomy and of repair on intra-articular contact areas and stress in the human knee. Am J Sports Med 14:270, 1986 61. Johnson RJ, Kettlekamp DB, Clark W, et al: Factors affecting late results after meniscectomy. J Bone Joint Surg [Am] 56:719-729, 1974 62. Shrive N: The weight-bearing role of the menisci of the knee. J Bone Joint Surg [Br] 56:381, 1974 63. Kettlekemp D, Jacobs A: Tibiofemoral contact area-determination and implications. J Bone Joint Surg [Am] 54:349-356, 1972 64. Lysholm J, Gilquist J, Lijedahl S-O: Long-term results after early treatment of knee injuries. Acta Orthop Seand 53:109-118, 1982 65. Lynch MA, Henning CE, Glick KR Jr: Knee joint surface changes. Long-term follow-up meniscus tear treatment in stable anterior cruciate ligament construction. Clin Orthop 172:148-153, 1983 66. Noble J, Erat K: In defense of the meniscus. A prospective study of 200 meniscectomy patients. J Bone Joint Surg [Br] 62:7, 1980 67. Shrive NG, O'Connor JJ, Goodfellow JW: Load bearing in the knee joint. Clin Orthop 131:279, 1978 68. Yocum LA, Kerlan RK, Jobe FW, et al: Isolated lateral meniscectomy. A study of twenty-six patients with isolated tears. J Bone Joint Surg [Am] 61:338-342, 1979 69. Bargar WL, Moreland JR, Markoff KL, et al: In-vivo stability testing of post-meniscectomy knees. Clin Orthop 150:247, 1980 70. Renstrom P, Johnson RJ: Anatomy and biomechanics of the menisci. Clin Sports Med 9:523-538, 1990 71. Levy IM, Torzilli PA, Warren RF: The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg [Am] 64:883-888, 1982 9