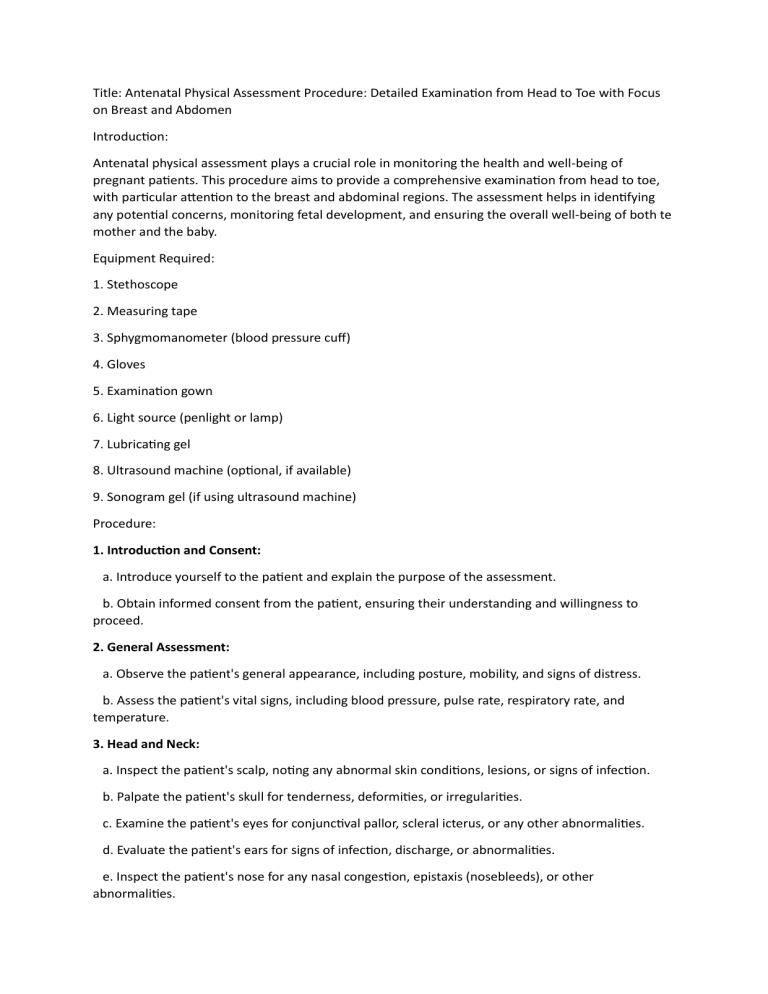
Title: Antenatal Physical Assessment Procedure: Detailed Examination from Head to Toe with Focus on Breast and Abdomen Introduction: Antenatal physical assessment plays a crucial role in monitoring the health and well-being of pregnant patients. This procedure aims to provide a comprehensive examination from head to toe, with particular attention to the breast and abdominal regions. The assessment helps in identifying any potential concerns, monitoring fetal development, and ensuring the overall well-being of both te mother and the baby. Equipment Required: 1. Stethoscope 2. Measuring tape 3. Sphygmomanometer (blood pressure cuff) 4. Gloves 5. Examination gown 6. Light source (penlight or lamp) 7. Lubricating gel 8. Ultrasound machine (optional, if available) 9. Sonogram gel (if using ultrasound machine) Procedure: 1. Introduction and Consent: a. Introduce yourself to the patient and explain the purpose of the assessment. b. Obtain informed consent from the patient, ensuring their understanding and willingness to proceed. 2. General Assessment: a. Observe the patient's general appearance, including posture, mobility, and signs of distress. b. Assess the patient's vital signs, including blood pressure, pulse rate, respiratory rate, and temperature. 3. Head and Neck: a. Inspect the patient's scalp, noting any abnormal skin conditions, lesions, or signs of infection. b. Palpate the patient's skull for tenderness, deformities, or irregularities. c. Examine the patient's eyes for conjunctival pallor, scleral icterus, or any other abnormalities. d. Evaluate the patient's ears for signs of infection, discharge, or abnormalities. e. Inspect the patient's nose for any nasal congestion, epistaxis (nosebleeds), or other abnormalities. f. Assess the patient's oral cavity, including the gums, teeth, and tongue, for signs of infection or abnormalities. g. Palpate the patient's neck lymph nodes gently to check for any enlargement or tenderness. 4. Breast Assessment: a. Ask the patient to remove their clothing from the waist up, providing a gown for modesty. b. Inspect both breasts for symmetry, skin changes, rashes, or any visible abnormalities. c. Palpate each breast using a systematic pattern (e.g., circular or vertical strip method) to detect any lumps, masses, or tenderness. d. Assess the patient's nipples for any discharge or abnormalities. e. Teach the patient about breast self-examination and provide educational resources if needed. 5. Abdominal Assessment: a. Ensure the patient is lying comfortably on their back with their abdomen exposed. b. Inspect the abdomen for any visible abnormalities, skin changes, or striae gravidarum (stretch marks). c. Palpate the abdomen gently, starting from the upper quadrants and moving downwards, assessing for tenderness, masses, or abnormal fetal movements. d. Measure the fundal height by placing the measuring tape from the pubic symphysis to the top of the uterus (fundus). e. Auscultate fetal heart sounds using a stethoscope or Doppler device, locating the fetal heart rate (FHR) in different areas of the abdomen. f. Perform Leopold's maneuvers, a series of palpations, to determine the fetal presentation, position, and engagement (if applicable). g. If available, perform an ultrasound examination to evaluate fetal growth, anatomy, and any potential abnormalities. 6. Lower Extremities: a. Inspect the patient's lower extremities for any edema, varicosities, or signs of deep vein thrombosis. b. Palpate pulses in the lower extremities, including the femoral, popliteal, posterior tibial, and dorsalis pedis pulses. 7. Conclusion: a. Thank the patient for their cooperation and reassure them about the findings during the assessment. b. Provide appropriate recommendations, advice, or referrals based on the assessment results. c. Address any questions or concerns the patient may have regarding their pregnancy or the assessment. Note: It is essential to maintain patient comfort, privacy, and dignity throughout the procedure. Obtain consent, explain each step to the patient, and address their questions or concerns. Documentation of the findings and appropriate follow-up is crucial for continuity of care.