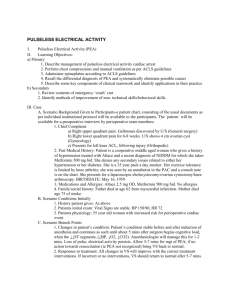
Pulseless electrical activity (PEA) is the presence of cardiac electrical activity with organized or partially organized cardiac rhythms without a palpable pulse. PEA is formerly known as electromechanical dissociation (EMD). PEA can present as any organized or partially organized rhythm on an electrocardiogram (ECG). PEA occur due to an event that takes place within the respiratory, cardiovascular, or gastrointestinal systems of the body which contributes to insufficient force generated by the heart following electrical depolarization. This insufficient force results in a weakened ability of the heart to contract, which can lead to a worsening cascade of pathophysiological changes. • Primary PEA is associated with cardiac causes (such as cardiac arrest), whereas secondary pulseless electrical activity is due to noncardiac causes. • Secondary PEA is due to potential reversible causes, known as the Hs & Ts. o H’s: Hypoxia; Hypovolemia; Hypo/hyperkalemia; Hydrogen ion (acidosis); Hypothermia. o T’s: Tension pneumothorax; Tamponade; Trauma; Thrombosis (coronary); Thrombosis (pulmonary) • Hypoxia and hypovolemia are two of the most common and potentially reversible causes of PEA. • Medications may increase susceptibility for the development of PEA. E.g., patients who use BBs or CCBs are at an increased risk for PEA because of decreased contractility of the heart due to altered intracellular calcium levels. • Pulmonary Embolus is a major cause of PEA in maternal health • Rhythm: vary depending on the underlying rhythm • Rate: vary depending on the underlying rhythm • P wave: varies; PEA may occur with and without visible P waves • PR interval: normal or prolonged, depending on underlying rhythm • QRS Complex: normal or wide, depending on underlying rhythm ✓ Absence of a palpable pulse ✓ Apnea ✓ Cyanosis ✓ Respiratory acidosis ✓ Hypothermia ✓ Electrolyte imbalance (e.g., hypo- or hyperkalemia) ✓ Blood loss/hemorrhage (resulting in hypovolemia) ✓ Pallor ✓ Hypoxia ✓ Jugular venous distention ✓ Tracheal deviation Important Note: a pulse that cannot be palpated does not always indicate PEA⎯ this could also occur due to abnormalities of the peripheral vascular system The first step in managing pulseless electrical activity is to begin chest compressions according to the advanced cardiac life support (ACLS) protocol followed by administrating epinephrine every 3 to 5 minutes, while simultaneously looking for any reversible causes. • CPR: o Effective CPR should be started, with minimal interruptions o Administer oxygen o Attach the defibrillator or cardiac monitor and evaluate the cardiac rhythm o Consider establishing an advanced airway and capnography • Medications o Epinephrine ▪ For a patient with cardiac arrest and a non-shockable rhythm such as pulseless electrical activity, administer epinephrine as early as possible ▪ 1mg IV/IO should be administered, eligible for additional doses every 3-5 minutes followed by 20 ml of flush ▪ Be sure to administer medications during CPR - do not stop CPR during medication administration o Atropine ▪ If the detected rhythm is bradycardia that is associated with hypotension ▪ Administer 1 mg IV every 3-5 min, up to three doses • Underlying Causes Interventions for managing pulseless electrical activity are focused on tending to the underlying cause of cardiac arrest rather than converting the cardiac rhythm. o Caring for the patient with pulseless electrical activity requires considerations outside of the algorithm o When assessing the patient, determine if there are any contributing and reversible underlying causes of the patient’s clinical condition (H’s and T’s) o Hypovolemia and hypoxia are two of the most common causes of pulseless electrical activity that are potentially reversible o Sodium bicarbonate may be used only in patients with severe, systemic acidosis, hyperkalemia, or tricarboxylic acid overdose. The dose is 1 mEq/kg